Abstract
Background
Wound infections following vascular procedures occur in 1–7 % of patients and can lead to severe problems including amputation and death. There are no established treatment options for this complication. The aim of our study was to introduce continuous irrigation as a new treatment technique.
Methods
We retrospectively evaluated patients who had undergone bypass surgery involving the groin and had been treated with continuous irrigation because of deep wound infections. The irrigation solution was saline in all cases. The patients were additionally treated with antibiotics. The end point of the study was either complete wound healing or complications such as recurrent infection, amputation, or death.
Results
Wound complications occurred in 65 (15.3 %) of 424 operations. Overall, 20 patients (4.7 %) developed a deep wound infection involving prosthetic graft material. They were treated with continuous irrigation. Complete wound healing was achieved in 13 cases (65.0 %). One patient died. No amputations were necessary.
Conclusions
Based on our results, constant irrigation may be a therapeutic option in patients with deep wound infections. The main advantages of continuous irrigation over other treatments are ongoing bacterial reduction despite primary wound closure and the ability to measure the remaining colonization by microbiologic examination of the irrigation fluid.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Wound infections occur in 1–7 % of patients who undergo vascular procedures [1, 2]. Especially in cases where graft material has been implanted, a wound-healing disturbance can turn into a life-threatening deep wound infection [3, 4]. Thus, patients with vascular diseases are a special challenge for every surgeon [5, 6]. Additionally, in patients with critical leg ischemia, peripheral lesions infected with multiple bacteria can lead to lymphatic invasion [7, 8].
The groin is of special importance for the development of deep wound infections [2, 4, 6]. This area is frequently involved during bypass surgery. Also, because of the adjacent lymphatic pathways/lymphatic nodes, the region is prone to developing bacterial ascension and local infection [8]. It is close to the anogenital area as well, making it vulnerable to further contamination. These problems gain even greater importance in the presence of poor nursing care [7].
Wound and graft infections have always been a major problem. Accordingly, certain classification systems were established decades ago [9, 10]. Since then, the prevention of postoperative infections has been a highly discussed topic [11–14].
When a wound infection has already occurred, however, it is a quite different situation than attempting to prevent it. In such cases, adequate treatment is mandatory to control the acute infection and, as a long-term aim, to maintain the vascular reconstruction [15, 16]. Various therapeutic options are recognized, from conservative to expanded surgical treatment, including the use of autologous, homologous, or prosthetic grafts as well as xenografts [2–8, 17]. To achieve wound closure, surgical options such as use of a vacuum-assisted system, muscle flap, or dermal transplantation have been described [4, 8, 18–20]. Despite these available options, no standard treatment can be recommended. Surgical-site infections, especially those associated with vascular surgery, remain a problem when dealing with such a severe problem in an aging society in which elderly patients are undergoing an increasing number of vascular procedures.
At our vascular center in a university teaching hospital, we use a continuous irrigation technique with a constant flow to decontaminate the infected site. As far as we know, this treatment has not been previously described. Accordingly, this retrospective survey was performed not only to discuss our own results of treating groin infections after arterial reconstruction but also to compare our technique with other treatment options.
Material and methods
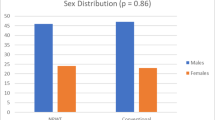
This retrospective study included 424 patients (285 men and 139 women, ages 41–90 years) at our vascular center who underwent surgery of the arterial system involving the groin area between June 2010 and June 2012. Surgical procedures included central and peripheral bypass reconstructions as well as reconstruction of the femoral junction. Patients whose operations were distal origin bypasses (proximal anastomosis distal of the groin), hemodialysis shunts, or that were performed at other hospitals were excluded from the study.
We defined a “wound complication” as a wound that did not heal primarily. The wounds were further divided into wound healing disturbances that could be treated conservatively (superficial wound dehiscence, necrosis of the margins, seroma, hematoma) and more severe wound complications that required a re-do operation. In the latter cases, we divided patients into two more groups based on Samson’s classification. The first group included those who required surgery for superficial wound infections that could not be treated conservatively (Samson 1 and 2). The second group included patients with severe bleeding or a deep infection (Samson 3–5).
Surgical steps at primary operation
Every patient was given a perioperative antibiotic 30 minutes before the surgical cut-down. Hair was removed in the operating room shortly before skin disinfection. A transurethral catheter (removed the following day) was inserted to avoid urinary contamination during the surgery. The bypass materials we used were polytetrafluoroethylene (PTFE) or Dacron. The patches were Dacron, polyurethane, or bovine pericardium. Before wound closure a drain was placed (usually 12 charriere), which was removed on postoperative day (POD) 2. Patient mobilization was restrained until then. Wound closure is performed by intracutaneous sutures, which were removed on POD 10.
Surgical procedures in case of wound infection
For superficial infections without involvement of graft material, we performed vacuum therapy followed by secondary wound closure. For deep wound infections with graft material involved, the prosthetic material was removed if it could be replaced with autogenous vein or bovine pericardium (as a nonuniversity hospital, we do not have the facilities to use homologous tissue). Otherwise the graft material was left in place, and continuous drainage was established. We did not use a commercial system for the drainage. Instead, we used a 16-charriere drainage tube with extra holes (made by hand) and diverted it proximal and distal to the wound edges (using a skewer) (Fig. 1). An infusion line (regular saline solution) was connected to the proximal tube (hanging from an infusion rack), thereby continuously flushing and draining the wound. There was a pouch in the distal tube. (Because there was no suction device, the pouch was placed lower than the patient). This setup resulted in a locked gravity drainage system that was left in place for several days (Figs. 2, 3, 4).
We routinely obtained intraoperative specimens for microbiologic testing. Calculated antibiotic therapy was continued postoperatively, being changed depending on the microbiologic test results. Specimens were obtained from the drainage pouch for 4–6 days. When the clinical evaluation (clear drainage fluid) and microbiologic tests (no bacteria or only a few in the fluid) and other laboratory tests were negative, the drainage system was removed at the bedside. Each patient with a wound complication was treated in hospital or at our outpatient clinic until complete wound closure was achieved. Once the wound had completely healed, we discontinued the antibiotic course.
Our clinical patient registry collected the patients’ data. Statistical significance for categoric variables was assessed using the χ 2 test. Data were analyzed using SSPS software (SSPS, Chicago, IL, USA) with differences considered significant at the level of p < 0.05.
Results
Wound complications occurred after 65 of 424 (15.3 %) operations. The study subjects comprised 37 men and 28 women, ages 47–90 years. Surgery had been performed because of peripheral arterial disease (PAD) stage II in 18 patients and critical leg ischemia in 38 patients (with the Fontaine classification, there would have been 8 patients with PAD stage III and 31 patients with PAD stage IV). An aortic aneurysm had been operated on (aortobifemoral prostheses) in two patients. Surgery (suture of the femoral artery) had been necessary because of bleeding after coronary catheter intervention in six patients. Of the 65 wound complications, 25 were successfully treated conservatively (38.5 % of all complications). Re-do surgery was necessary in the other 40 patients: 9 because of bleeding (no infection), 11 because of superficial wound healing disturbances (Samson 1–2) (30.7 % of all wound complications), and 20 because of a deep wound infection involving prosthetic graft material (Samson 3–5) (Table 1).
Operative procedures in patients with deep wound infections were as follows:
-
Wound debridement, continuous irrigation therapy (CIT) (n = 12)
-
Wound debridement, partial explantation of graft material, CIT (n = 4)
-
Wound debridement, total explantation of graft material, CIT (n = 4)
Table 2 shows the patients’ data. Microbiologic examination of the irrigation fluid specimens yielded Staphylococcus aureus in 50.0 % of cases. Among them were two cases of methicillin-resistant S. aureus (MRSA). The patients underwent CIT for 4–12 days (mean 6.8) days. After this therapy, no bacteria were detected in the microbiologic analysis of the drainage pouch in 12 patients and only very low concentrations in 4 patients. Despite clinical and intraoperative signs of infection in three patients, there were no pathologic findings at the time of the re-do operation, possibly due to insufficient sample-taking.
Complete wound healing with no further measurements was achieved in 13 cases (65.0 %). Among these patients, 10 had either graft material that remained intact (n = 7, two bovine pericardial patches) or was partially explanted (n = 3). In the other three patients, a second operation was necessary (total graft explantation, replacement by autologous vein) (Table 2) because of inadequate wound healing. However, all but one of these operations (patient 10: acute anastomotic bleeding with fatal consequences) were performed electively and eventually led to healing of the wound (Table 2). In no case as amputation necessary.
Overall, 11 of the 424 patients died (only 1 of the 65 with wound complications) during the early postoperative course (within 30 days) (in-hospital lethality 2.6 %/1.5 %). Cause of death was the underlying disease in nine cases (PAD stage IV in all nine patients) and severe apoplexia in one patient. One patient (as noted) eventually died because of complications of the wound infection. The follow-up period in patients with deep wound infection was 15 months (patient 17) to 27 months (patient 2) (mean follow-up 18 months). For patients with complete wound healing, follow-up periods were 15–26 months (average 19 months). Two patients (nos. 2 and 19) died after 19 and 20 months, respectively, owing to a heart attack.
Statistical analysis showed significant results between bacteria-free findings after CIT and uncomplicated healing of deep wound infections (p = 0.015). The presence of peripheral lesions (PAD stage IV) did not have any effect concerning the course of events after wound infection (p = NS).
Discussion
Postoperative infections of the inguinal region are a severe problem of arterial reconstruction surgery [4]. The involvement of graft material in the infection is the worst-case scenario [9]. Generally, re-do operations of infectious sites are a great challenge. Furthermore, they are often performed under emergency conditions during on-call hours [3, 7, 15]. The therapeutic option of choice is complete resection of the graft material [2, 3]. However, this strategy demands some kind of reconstruction using either autologous material or extra-anatomic techniques. Inappropriate autologous material and poor therapeutic outcomes of extra-anatomic bypass have been described [2, 3]. Conservative treatment (antibiotics) alone may be ineffective [17]. Special graft materials (silver, antibiotic-covered) can also be unsafe in infectious situations [13]. Homografts as an alternative are not available in most hospitals.
Therefore, attention has been directed to trying to stabilize the infectious situation without resecting the graft material—disregarding one of the general surgical principles of removing alloplastic material in case of infection [21]. Still, the problems mentioned above often make it necessary to leave graft material in situ. Especially for groin infections, this often means “squaring the circle”—i.e., eliminating the colonizing bacteria without removing graft material and without the option of open wound treatment. In such cases, sufficient wound debridement to reduce germ colonization is mandatory [3, 18, 22]. The second step requires that wound closure be performed. Technically, this means muscle flap coverage, vacuum-assisted closure, or both. Dosluoglu et al. described 12 patients with exposed grafts who were treated with vacuum-assisted closure alone. Healing occurred in 83 % [18]. Kotsis and Lioupis [23] reported on six patients successfully treated with vacuum therapy. Karl and Storck described 19 patients with graft infections, all of whom were treated with vacuum therapy. There were 5.3 % reinfections and 10.5 % major amputations [24]. Herrera et al. described 11 patients who had deep wound infections and were treated with tissue flap coverage and vacuum therapy. Healing was achieved in 6 of the 11 patients while preserving the graft [2]. In a retrospective analysis. Colwell et al. [25] reported nine successful results.
These reports not only show differences concerning the size of wounds and the infection types and outcomes, there was a limited number of patients and different occurrences of wound infections (early/late postoperative). These factors make it difficult to judge the different approaches [23–27]. As other authors do, we use vacuum therapy only in case of superficial infections without involving deeper layers or graft material [20, 22]. We had had disappointing results in cases of infected graft material in the past. A major problem is the remaining areas in deep wounds that cannot be reached sufficiently by the vacuum sponge, leading to an ineffective healing process. We are of the opinion that a sufficient barrier can be reached only by a biologic closure. Another side effect of vacuum therapy is the long duration of treatment (weeks to months [2, 18, 28]), including long hospital stays and (even in case of ambulant treatment) hindered mobilization.
As an alternative, we developed a modified therapy wherein the main goal is stabilizing the infectious area. We accomplish this state by applying sufficient wound debridement followed by insertion of irrigation drains and wound closure. With this treatment, we intended to reduce bacterial colonization leading to a stabilized patient—followed by further steps as needed. As a result, we did not generally need to resect all graft material (similar to the reports mentioned above), but we were still able to reduce bacterial colonization by constantly irrigating the wound.
In our case series, we achieved total elimination of bacteria in 13 of 20 (56 %) patients. The patients’ wounds healed despite the remaining graft material. In the other cases, total removal of alloplastic material became necessary later in the course of events. However, these operations were performed electively in all but one patient (the only one who died). We were especially successful in patients who had central and peripheral bypasses. By explanting only the peripheral graft, we managed to save the central prosthesis even though it had been infected (femoral anastomosis).
Thus, constant irrigation may be an alternative in the acute situation of deep wound infections of the groin. It allows the patient and surgeon to avoid extended reconstructions, leading to a gain in time for further treatment options.
Limitations of this treatment are the extended infections (total involvement of a prosthetic bypass). In such cases, explantation of the graft is often mandatory, even in such patients in whom the acute inflammatory process can be interrupted by constant irrigation. Further operations can be performed in noninflamed tissue in a stabilized patient and as an elective operation. As no special wound closure measurements were necessary, we did not face problems such as retraction of the wound margins. Our results concerning long-term healing and complications (major amputation, death) were satisfactory. Microbiologic examination of the irrigation fluid seems to be of good use as an indicator of the wound status.
Conclusions
Based on our results, we believe that constant irrigation is a therapeutic option for deep wound infections. Because of the limited number of patients, however, further studies are needed to confirm our results.
References
Darouiche R (2004) Treatment of infections associated with surgical implants. N Engl J Med 350:1422–1429
Herrera F, Kohanzadeh S, Nasseri Y et al (2009) Management of vascular graft infections with soft tissue flap coverage: improving limb salvage rates—a Veterans Affairs experience. Am Surg 75:877–881
Hasse B, Husmann L, Zinkernagel A et al (2013) Vascular graft infections: review article. Swiss Med Wkly 143:w13754
Williams I, Milling M, Shandall A (2003) Vascularised muscular flaps and arterial graft infection in the groin. Eur J Vasc Endovasc Surg 25:390–395
Bandyk D (2008) Vascular surgical site infection: risk factors and preventive measures. Semin Vasc Surg 21:119–123
Antonios V, Noel A, Steckelberg J et al (2006) Prosthetic vascular graft infection: a risk factor analysis using a case–control study. J Infect 53:49–55
Debus E (2012) Infektionen in der Gefäßchirurgie. Gefäßchirurgie 17:6–7
Cherry K, Roland C, Pairolero P et al (1992) Infected femorodistal bypass: is graft removal mandatory? J Vasc Surg 5:295–303
Szylagyi E, Smith R, Elliott J et al (1972) Infection in arterial reconstruction with synthetic grafts. Ann Surg 176:321–333
Samson R, Veith F, Janko G (1988) A modified classification and approach to the management of infections involving peripheral arterial prosthetic grafts. J Vasc Surg 8:147–153
Rieger H, Schoop W (2004) Allgemeine Maßnahmen bei Eingriffen am Gefäßsystem. In: Heberer, van Dongen (eds) Gefäßchirurgie. Springer, New York
Kogel H (2001) Möglichkeiten des Gefässersatzes und Einsatz von Nahtmaterialien. In: Hepp H, Kogel H (eds) Gefäßchirurgie. Urban und Schwarzenberg, Jena
Kellersmann R, Assadian O, Zegelman M (2012) Infections of vascular prostheses: options for prophylaxis. Gefässchirurgie 17:12–22
Mangram A, Horan T, Pearson M et al (1999) Guideline for prevention of surgical site infection. Infect Control Hosp Epidemiol 20:247–280
Calligaro K, Veith F, Yuan J et al (2003) Intra-abdominal aortic graft infection: complete or partial graft preservation in patients at very high risk. J Vasc Surg 38:1199–1205
Swain T, Calligar K, Dougherty M (2004) Management of infected aortic prosthetic grafts. Vasc Endovasc Surg 38:75–82
Saleem B, Meerwaldt R, Tielliu I et al (2010) Conservative treatment of vascular prosthetic graft infection is associated with high mortality. Am J Surg 200:47–52
Dosluoglu H, Loghmanee C, Lall P et al (2010) Management of early (<30 days) vascular groin infections using vacuum-assisted closure alone without muscle flap coverage in a consecutive patient series. J Vasc Surg 51:1160–1166
Mayer D, Hasse B, Koelliker J et al (2011) Long-term results of vascular graft and artery preserving treatment with negative pressure wound therapy in Szylagyi grade III infections justify a paradigm shift. Ann Surg 254:754–759
Svensson S, Monsen C, Kölbel T et al (2008) Predictors for outcome after vacuum assisted closure therapy of perivascular surgical site infections in the groin. Eur J Vasc Endovasc Surg 36:84–89
Taylor S, Weatherford D, Langan E et al (1996) Outcomes in the management of vascular prosthetic graft infections confined to the groin: a reappraisal. Ann Vasc Surg 10:117–122
Töpel I, Steinbauer M (2012) Biologische Sicherungsoperationen bei infektiösen Komplikationen in der Leiste. Gefässchirurgie 17:63–73
Kotsis T, Lioupis C (2007) Use of vacuum assisted closure in vascular graft infection confined to the groin. Acta Chir Belg 107:37–44
Karl T, Storck M (2012) Negative pressure wound therapy (NPWT). Gefässchirurgie 17:37–45
Colwell A, Donaldson M, Belkin M et al (2004) Management of early groin vascular bypass graft infections with sartorius and rectus femoris flaps. Ann Plast Surg 52:49–53
Dosluoglu H, Schimpf D, Schultz R et al (2005) Preservation of infected and exposed vascular grafts using vacuum assisted closure without muscle flap coverage. J Vasc Surg 42:989–992
Domingos C, Schulte S, Horsch S (2007) Vacuum assisted wound closure in postoperative periprosthetic groin infections: a new gold standard? J Cardiovasc Surg (Torino) 48:477–483
Berger P, de Bie D, Moll F et al (2012) Negative wound therapy on exposed prosthetic vascular grafts in the groin. J Vasc Surg 56:714–720
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thermann, F., Wollert, U. Continuous Irrigation as a Therapeutic Option for Graft Infections of the Groin. World J Surg 38, 2589–2596 (2014). https://doi.org/10.1007/s00268-014-2650-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2650-8