Abstract
Background
Despite the availability of more accurate imaging modalities, specifically multidetector computed tomography (MDCT), the diagnosis of non-ischemic (NI-) and ischemic (I-) blunt hollow viscus and mesenteric injury (BHVMI) remains challenging. We hypothesized that BHVMI can be still missed with newer generations of MDCT and that patients with I-BHVMI have a poorer outcome than those with NI-BHVMI.
Methods
We performed an eight-year retrospective review at a level 1 trauma center. Ischemic-BHVMI was defined as devascularization confirmed at laparotomy. Non-ischemic-BHVMI included perforation, laceration, and hematoma without devascularization. The sensitivity of each generation of MDCT for BHVMI was calculated. Potential predictors and outcomes of I-BHVMI were compared to the NI-BHVMI group.
Results
Of 7,875 blunt trauma patients, 67 patients (0.8 %) were included in the BHVMI group; 13 patients did not have any CT findings suggestive of BHVMI (sensitivity 81 %), and 11 of them underwent surgical intervention without delay (<5 h). Newer generations of MDCT were not associated with higher sensitivity. Patients with I-BHVMI had a significantly higher rate of delayed laparotomy ≥12 h (23 % versus 2 %; p = 0.01) and a significantly longer length of hospital stay (median 14 versus 9 days; p = 0.02) than those with NI-BHVMI.
Conclusions
Even using an advanced imaging technique, the diagnosis of I-BHVMI can be delayed, with significant negative impact on patient outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multidetector computed tomographic (MDCT) scanning has assumed a greater role in the diagnosis of injured patients, often replacing other imaging modalities [1–3]. For example, conventional angiography, long considered the “gold standard” in the diagnosis of traumatic vascular injury, has been progressively replaced by CT angiography [4–6]. Furthermore, many trauma management guidelines are now based on the findings of MDCT, such as those for the treatment of hemodynamically stable patients with solid organ injury [7, 8].
However, there are organ injuries for which the accuracy of MDCT diagnosis may still be questioned [9, 10]. Blunt hollow viscus and mesenteric injury (BHVMI) is one such condition. Before the era of MDCT scanning, a large retrospective multi-institutional study revealed that CT scan findings were entirely normal in up to 13.0 % of patients with blunt small bowel perforation [11]. The fairly high false negative rate of CT diagnosis of BHVMI resulted in the frequent use of diagnostic peritoneal lavage (DPL) as an adjunctive test, with imperfect accuracy [12].
With recent enthusiasm for the use of MDCT in the management of injured patients, an increasing body of literature has re-evaluated the efficacy of this newer modality for BHVMI [13–21]. This work is widely disparate, with some authors reporting an accuracy rate approaching 100 %, while others demonstrate that as many as 20 % of BHVMI can be missed by MDCT. The discrepancy in these results may be related to the lack of discrimination between ischemic (I-) and non-ischemic (NI-) BHVMI.
Devascularizing injury is categorized as the highest grade of BHVMI in the organ injury scale of the American Association for the Surgery of Trauma (AAST) [22]. Severe mesenteric injury compromising visceral blood flow can cause ischemia and delayed necrosis. Although most severe mesenteric injury should result in concomitant active bleeding that can be identified on CT scan by contrast extravasation or formation of a hematoma, initial imaging can also be entirely normal or demonstrate only subtle findings [13]. In such cases, the timing of therapeutic laparotomy can be delayed significantly, with impaired clinical outcomes.
The purpose of the present study was to evaluate the sensitivity of MDCT for the diagnosis of BHVMI. We also sought to investigate the outcome of I-BHVMI compared with NI-BHVMI. We hypothesized that the use of the newer generations of MDCT improves the diagnosis of BHVMI, but that definitive treatment can be still delayed in I-BHVMI patients whose clinical outcome is poorer than the outcomes recorded in NI-BHVMI.
Patients and methods
This study was approved by the institutional review board of Penn State College of Medicine. Penn State Milton S. Hershey Medical Center is a regional academic level 1 trauma center with a catchment area of approximately 1.2 million. Patient data were extracted from the institutional trauma database. Study data were collected from 2002 to 2009 based on the following injury codes: stomach, duodenum, small bowel, colon, rectum, and small bowel/colon mesentery. Patients who sustained penetrating injury or who were taken to the operating room (OR) immediately for exploratory laparotomy without a prior CT scan were excluded from this study.
The BHVMI group was defined as patients who had laparotomy-confirmed perforation, laceration, hematoma, or devascularization of the mesentery, stomach, small intestine, and large intestine. Patient baseline characteristics, clinically relevant data, and potential risk factors for BHVMI were collected from the database and hospital medical records. The decision of whether to obtain an abdominal CT scan was at the discretion of the attending trauma surgeon based on clinical judgment.
At the beginning of the study period in 2002, CT imaging was performed with a 4-slice MDCT scanner that was upgraded serially to a 16-slice scanner in 2005, a 40-slice scanner in 2007, and a 64-slice scanner (Siemens Medical Systems, Erlangen, Germany) in 2008. All CT images were obtained after administration of low osmolar intravenous contrast (Omnipaque, GE Healthcare, Little Chalfont, UK) without oral, nasogastric, or rectal contrast. The CT images were reviewed by a radiology resident and subsequently finalized by a board-certified attending radiologist. The radiology resident assigned to the emergency department reviewed the CT images at the time of study, and the findings were discussed with the senior trauma resident or attending trauma surgeon. Seven CT findings suggestive of possible BVHMI (BHVMI CT findings: mesenteric stranding, mesenteric hematoma, active mesenteric vessel extravasation, bowel wall thickening, extraluminal air, abnormal bowel wall enhancement, intraperitoneal free fluid in the absence of solid viscus injury) were evaluated for all patients [11, 15]. The overall sensitivity of MDCT for these seven BHVMI findings was calculated, along with the sensitivities for each generation of MDCT scanner.
We subsequently stratified the BHVMI patients into I-BHVMI and NI-BHVMI subgroups, and tested for associations between groups with patient characteristics, associated injuries, laboratory tests, and CT results [23, 24]. For this purpose, we used Wilcoxon tests to compare continuous variables and Fisher’s exact tests to compare binary variables. The same tests were used to compare outcomes (mortality, major complication, and length of hospital stay) between groups. Because of the small sample size, no multivariate models were fitted.
Results
A total of 7,875 blunt-injured patients were identified during the study period from our institutional registry, 84 of whom had BHVMI. Seventeen cases were excluded from the analysis as these patients were taken to the operating room immediately for exploratory laparotomy based on clinical judgment without a CT scan. Therefore, 67 patients (0.8 %) were included.
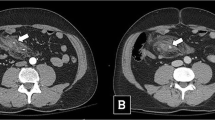
Patient characteristics and BHVMI CT findings are shown in Table 1. Only 61 % of patients had a positive finding during the abdominal examination at admission. Initial WBC count was greater than 10,000 in the majority of patients, whereas the incidence of elevated amylase level was only 16 %. Isolated fluid collection without associated solid organ injury was the most common CT BHVMI finding. Overall sensitivity of MDCT for BHVMI was 81 %. Figure 1 shows the sensitivity of each generation of MDCT scanner for seven BHVMI findings. The highest sensitivity was for the 40-slice MDCT scanner (93 % sensitivity; 95 % CI 66 % to 99 %), the 64-slice scanner showed a sensitivity of only 65 % (95 % CI 38 % to 85 %).
There were no positive BHVMI CT findings for 13 patients (Table 2), most of whom (11/13) were taken to the OR <5 h after arrival in the emergency department. In 9 patients, associated injuries requiring laparotomy were identified on the CT scan. The other 2 patients were taken to the OR emergently because of the development of early peritonitis. Two additional patients developed peritonitis over the course of admission and underwent laparotomy >12 h after presentation. There was no mortality identified in these 13 cases.
Among 67 BHVMI patients, 26 patients (39 %) were identified as having I-BHVMI. A comparison between the I-BHVMI and NI-BHVMI group is shown in Table 3. An elevated serum amylase level was found in 72 % of NI-BHVMI patients, whereas all I-BHVMI patients had a normal value (p = 0.002). The incidence of associated pelvic fracture was significantly higher in the I-BHVMI group (42 % versus 17 %; p = 0.046). Sensitivity of MDCT for any positive BHVMI CT findings were similar in the I-BHVMI and NI-BHVMI groups (85 % and 78 %; p = 0.75). Although extraluminal gas tended to be found more often in NI-BHVMI group, no CT scan findings were shown to be significant between I-BHVMI and NI-BHVMI.
Six patients (23 %) in the I-BHVMI group were taken to the OR ≥12 h after presentation compared to 1 patient (2 %) in the NI-BHVMI group (p = 0.011) (Tables 4 and 5). At laparotomy, the injury was identified in the ileocecal segment in 12 I-BHVMI cases (46 %). The most frequent site of injury in the NI-BHVMI group was jejunum (37 %). Five patients (12 %) had the injury in the ileocecal segment. Some 96 % of patients in the I-BHVMI group required surgical resection (versus 20 % in the NI- BHVMI group; p < 0.001). However, only 2 I-BHVMI patients (8 %) underwent a diversion procedure (versus 2 % in the NI-BBHVI group; p = 0.56). Two patients in each group died during the course of their hospitalization (8 % versus 5 %; p = 0.64). All deaths were due to associated injuries. Length of hospital stay was significantly longer in the I-BVHMI group (median 14 versus 9 days; p = 0.018). The major complication rate during hospital stay was higher in the I-BHVMI group, but the difference was not statistically significant (46 % versus 22.0 %; p = 0.06).
Discussion
The present study has demonstrated a lower incidence of delayed diagnosis of BHVMI than previous reports [11, 13]. Although the sensitivity of MDCT specifically for BHVMI findings was 81 %, only 6 % of patients had entirely normal CT results. We have also focused on the poorer outcome among I-BHVMI patients and to NI-BHVMI. The diagnosis of I-BHVMI was more likely delayed than NI-BHVMI.
Whereas CT scan, even before the era of MDCT, has been considered the gold standard for the diagnosis of intra-abdominal solid organ injury, its efficacy in the diagnosis of BHVMI has not been established. Nonetheless, 77 % of respondents would use the CT scan as an initial diagnostic imaging for blunt small bowel injury in a nationwide survey performed in the late 1990s [25]. This number is undoubtedly even higher today because of the ready availability of MDCT.
Using logistic regression analysis, Elton and colleagues identified significant CT findings related to BHVMI [26]. Isolated free fluid, pneumoperitoneum, and bowel wall thickening were significantly associated with BHVMI in a 4-slice spiral CT scan. Since the introduction of MDCT, only a few articles have been published regarding BHVMI [13–19]. Brofman and colleagues reported various MDCT findings seen in patients with BHVMI [18]. Bowel wall discontinuity, extraluminal contrast material, and extraluminal air were considered specific for bowel injury. Mesenteric extravasation, mesenteric vascular beading, and termination of mesenteric vessels were considered specific for mesenteric injury. Their group also performed a case–control study using matched groups to determine the accuracy of MDCT for BHVMI requiring surgery [15]. The radiology resident and fellow radiologists successfully made the diagnosis of BHVMI in 36 of 38 cases (95 %). Tan and colleagues reviewed BHVMI patients who required laparotomy and underwent MDCT using a 4-slice or 64-slice scanner [14]. All cases demonstrated an abnormal preoperative CT scan. In contrast, Ekeh and colleagues showed a very high false negative CT rate (20 % with 4-slice MDCT, 17.6 % with 16-slice MDCT) [13]. Our results with ever newer generations of MDCT support their data.
To the best of our knowledge, this is the first study that has focused on the I-BHVMI. We found that I-BHVMI was significantly associated with pelvic fracture. Frick and colleagues reported that 22.9 % of their patients with BHVMI had associated pelvic fracture [24]. Shearing forces along the line of attachment of mesentery is believed to be the mechanism of mesenteric injury. Therefore, proximal jejunum and ileocecal mesentery are commonly injured. The most frequent site of I-BHVMI in our study was the ileocecal segment.
Although our study demonstrated a lower incidence of delayed diagnosis of BHVMI compared to previous literature [27, 28], 23 % of I-BHVMI patients still underwent operation ≥12 h after presentation. This was a significantly higher rate than for the NI-BHVMI group. The reason for this result remains unclear. None of the clinical data or BHVMI CT findings were more significantly associated with the I-BHVMI than with NI-BHVMI. Notably, the majority of the pelvic fractures in the I-BHVMI group required surgical fixation early in the hospital course. This would suggest that high grade pelvic fractures may be associated with I-BHVMI. Patients with delayed diagnosis of I-BHVMI frequently underwent pelvic fixation within 24 h of admission. In addition to the surgical procedure itself, postoperative pain could also have delayed the diagnosis of BHVMI in these cases.
The delay in diagnosis of BHVMI is well known to be significantly associated with poor outcome [29]. Classically, the delay in operative intervention beyond 24 h results in increased patient mortality and morbidity [29, 30]. This “cut-off” time for worsened outcome may be as short as 5–8 h [27, 28, 31]. While the mortality rate for I-BHVMI patients was similar to that for the NI-BHVMI group, LOS was significantly longer in the I-BHVMI group. This might be attributed to the difference in the type of procedure between the two groups. Recovery time from bowel resection, particularly advancing diet, is usually longer than simple repair of injury. Also, the in-hospital complication rate in I-BHVMI group tends to be higher than in the NI-BHVMI group. Nevertheless, we were unable to specify the type of complication that could create the increased LOS.
There are several potential limitations to our study. First, it was a retrospective single-institution study with a small sample size because of the low incidence of BHVMI. Second, the generation of MDCT scan was different between the beginning and the end of the study period because of the progressive evolution in technology. Ekeh and colleagues showed that there was no significant difference in the outcome of BHVMI patients between the 4-slice and the 16-slice MDCT technology [13]. Finally, patients with missed injuries could have presented at other institutions.
In conclusion, BHVMI can be missed with the newer generations of MDCT. Patients with I-BHVMI are at a greater risk of delayed diagnosis with poorer outcome than those with NI-BHVMI. A larger scale prospective study is needed to verify the accuracy of the current generation of MDCT scanners for the diagnosis of BHVMI.
References
Huber-Wagner S, Lefering R et al (2009) Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 373:1455–1461
Fang JF, Wong YC, Lin BC et al (2006) Usefulness of multidetector computed tomography for the initial assessment of blunt abdominal trauma patients. World J Surg 30:176–182. doi:10.1007/s00268-005-0194-7
Poletti PA, Mirvis SE, Shanmuganathan K et al (2004) Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma 57:1072–1081
Bruckner BA, DiBardino DJ, Cumbie TC et al (2006) Critical evaluation of chest computed tomography scans for blunt descending thoracic aortic injury. Ann Thorac Surg 81:1339–1346
Seamon MJ, Smoger D, Torres DM et al (2009) A prospective validation of a current practice: the detection of extremity vascular injury with CT angiography. J Trauma 67:238–243
Eastman AL, Chason DP, Perez CL et al (2006) Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: is it ready for primetime? J Trauma 60:925–929
Moore FA, Davis JW, Moore EE Jr et al (2008) Western Trauma Association (WTA) critical decisions in trauma: management of adult blunt splenic trauma. J Trauma 65:1007–1011
Kozar RA, Moore FA, Moore EE et al (2009) Western Trauma Association critical decisions in trauma: nonoperative management of adult blunt hepatic trauma. J Trauma 67:1144–1148
Phelan HA, Velmahos GC, Jurkovich GJ et al (2009) An evaluation of multidetector computed tomography in detecting pancreatic injury: results of a multicenter AAST study. J Trauma 66:641–646
Linsenmaier U, Wirth S, Reiser M et al (2008) Diagnosis and classification of pancreatic and duodenal injuries in emergency radiology. Radiographics 28:1591–1602
Fakhry SM, Watts DD, Luchette FA, EAST Multi-Institutional Hollow Viscus Injury Research Group (2003) Current diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trial. J Trauma 54:295–306
Fang JF, Chen RJ, Lin BC (1998) Cell count ratio: new criterion of diagnostic peritoneal lavage for detection of hollow organ perforation. J Trauma 45:540–544
Ekeh AP, Saxe J, Walusimbi M et al (2008) Diagnosis of blunt intestinal and mesenteric injury in the era of multidetector CT technology—are results better? J Trauma 65:354–359
Tan KK, Liu JZ, Go TS et al (2010) Computed tomography has an important role in hollow viscus and mesenteric injuries after blunt abdominal trauma. Injury 41:475–478
Atri M, Hanson JM, Grinblat L et al (2008) Surgically important bowel and/or mesenteric injury in blunt trauma: accuracy of multidetector CT for evaluation. Radiology 249:524–533
Menegaux F, Trésallet C, Gosgnach M et al (2006) Diagnosis of bowel and mesenteric injuries in blunt abdominal trauma: a prospective study. Am J Emerg Med 24:19–24
Scaglione M, de Lutio di Castelguidone E, Scialpi M et al (2004) Blunt trauma to the gastrointestinal tract and mesentery: is there a role for helical CT in the decision-making process? Eur J Radiol 50:67–73
Brofman N, Atri M, Hanson JM et al (2006) Evaluation of bowel and mesenteric blunt trauma with multidetector CT. Radiographics 26:1119–1131
Yu J, Fulcher AS, Turner MA et al (2011) Blunt bowel and mesenteric injury: MDCT diagnosis. Abdom Imaging 36:50–61
Hanks PW, Brody JM (2003) Blunt injury to mesentery and small bowel: CT evaluation. Radiol Clin North Am 41:1171–1182
Sharma OP, Oswanski MF, Singer D et al (2004) The role of computed tomography in diagnosis of blunt intestinal and mesenteric trauma (BIMT). J Emerg Med 27:55–67
Moore EE, Cogbill TH, Malangoni MA et al (1990) Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma 30:1427–1429
Williams MD, Watts D, Fakhry S (2003) Colon injury after blunt abdominal trauma: results of the EAST Multi-Institutional Hollow Viscus Injury Study. J Trauma 55:906–912
Frick EJ Jr, Pasquale MD, Cipolle MD (1999) Small-bowel and mesentery injuries in blunt trauma. J Trauma 46:920–926
Brownstein MR, Bunting T, Meyer AA et al (2000) Diagnosis and management of blunt small bowel injury: a survey of the membership of the American Association for the Surgery of Trauma. J Trauma 48:402–407
Elton C, Riaz AA, Young N et al (2005) Accuracy of computed tomography in the detection of blunt bowel and mesenteric injuries. Br J Surg 92:1024–1028
Fakhry SM, Brownstein M, Watts DD et al (2000) Relatively short diagnostic delays (< 8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma 48:408–414
Malinoski DJ, Patel MS, Yakar DO et al (2010) A diagnostic delay of 5 hours increases the risk of death after blunt hollow viscus injury. J Trauma 69:84–87
Fang JF, Chen RJ, Lin BC et al (1999) Small bowel perforation: is urgent surgery necessary? J Trauma 47:515–520
Niederee MJ, Byrnes MC, Helmer SD et al (2003) Delay in diagnosis of hollow viscus injuries: effect on outcome. Am Surg 69:293–298
Watts DD, Fakhry SM, EAST Multi-Institutional Hollow Viscus Injury Research Group (2003) Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma 54:289–294
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matsushima, K., Mangel, P.S., Schaefer, E.W. et al. Blunt Hollow Viscus and Mesenteric Injury: Still Underrecognized. World J Surg 37, 759–765 (2013). https://doi.org/10.1007/s00268-012-1896-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1896-2