Abstract
Background
Cancer of the thyroid gland is rare in children and adolescents. A history of neck irradiation is a well-established risk factor for tumor development, and most previous reports focused on cases that were induced by radiation exposure. We present here a retrospective review of the clinical features, treatment, and long-term outcome of children and adolescents with papillary thyroid cancer (PTC) without a history of radiation exposure who were treated at our institution over a period of ~50 years.
Methods
We retrospectively investigated 142 PTC patients without an irradiation history who were younger than 20 years of age when treated from 1961 to 2005 (17 males and 125 females; mean age = 16.3 ± 2.7 years; follow-up = 21.8 ± 12.0 years). The clinicopathological results were evaluated using the medical records. Disease-free survival (DFS) and cause-specific survival (CSS) were assessed with the Kaplan-Meier method and compared with the log-rank test. Parametric analyses were performed using Student’s t test and nonparametric analyses were performed using the Mann–Whitney U test.
Results
At diagnosis, three patients had distant lung metastasis and 33 had gross neck lymph node (LN) metastasis. All patients were treated with surgery (hemi/partial thyroidectomy in 45 patients, subtotal thyroidectomy in 85, total thyroidectomy in 12, no LN dissection in 50, central compartment dissection in 20, and modified radical neck dissection in 72), and postoperative external beam radiation therapy was administered to 59. Postoperative ablative therapy using I131 was not performed in this series. Recurrence was found for regional LN (n = 25), lung (n = 9), remnant thyroid (n = 5), and others (n = 4). DFS and CSS at 40 years were 74.1 and 97.5%, respectively. DFS was significantly worse in patients aged <16 years with a family history of thyroid cancer, preoperative neck gross LN metastasis, maximum tumor diameter, and extrathyroidal invasion. Preoperative gross neck LN metastasis and distant metastasis at diagnosis were significant factors for CSS. No other factors contributed to DFS and CSS. When the clinical features of children and adolescents were compared, the incidence of preoperative gross neck LN metastasis and distant metastasis at diagnosis and tumors with a maximum diameter >10 mm were significantly higher in the children group than in the adolescent group. DFS was significantly shorter in the children group than in the adolescent group, but no significant difference was found in CSS between these two groups.
Conclusions
The prognosis of PTC in children and adolescents is excellent, regardless of the extent of thyroidectomy and LN dissection. We recommend that only children or adolescents with preoperative gross neck LN metastasis and distant metastasis at diagnosis should be subjected to postoperative ablative therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignancy of the thyroid gland is rare in children and adolescents, with a reported incidence of 2.6–12.9% of all thyroid malignancy patients [1–6]. Papillary thyroid cancer (PTC) is the most common thyroid malignancy in pediatric and adult patients [1–5]. Radiation exposure in children has been reported to be associated with the occurrence of PTC [7–10]. The majority of previous reports focused on the incidence of PTC in children that was induced by radiation exposure, which is associated mainly with the Chernobyl accident [11, 12]. Indeed, only a few studies have focused on the incidence of PTC in children and adolescents in the absence of radiation exposure.
Many studies have reported higher recurrence and survival rates for PTC in children without radiation exposure than in adults [1–6], with recurrence and mortality rates in children of 15–40 and 0–13%, respectively [13–17]. Long-term follow-up periods are needed and the outcome should be discussed in the long-term context, especially for children. The majority of studies had follow-up periods of 10–20 years and only a few studies have provided results for a period longer than 30 years [6, 18, 19].
We present here a retrospective review of the clinical features, treatment, and long-term outcome of PTC in children and adolescents without a history of radiation exposure over a period of 50 years.
Patients and methods
We performed 142 primary surgical resections of PTC in patients younger than 20 years without a history of irradiation who were treated from 1961 to 2005 at the Noguchi Thyroid Clinic and Hospital Foundation. The details of the patients’ presentations, family history, radiation history, surgical and pathological findings, adjunctive therapy, and outcome were obtained from our hospital’s computerized database, and these data were confirmed using the medical records. The patients were 17 males and 125 females with a median age at initial operation of 16.3 ± 2.7 years (range = 6–19 years). There were 40 patients aged ≤15 years old (children group) and 72 patients aged >15 years (adolescent group). The median follow-up period was 21.8 ± 12.0 years. A familial history of thyroid cancer was seen in 12 patients. We did not include PTC with specific pathology in this study, e.g., poorly differentiated carcinoma and variants of PTC (cribriform-morula, tall cell, and follicular variants).
We analyzed the differences in the following clinical variables between children (≤15 years) and adolescents (>15 years): gender, familial history of thyroid cancer, preoperative gross neck lymph node (LN) metastasis, distant metastasis at initial presentation, maximum tumor diameter, extrathyroidal invasion at primary site, and tumor multiplicity. Statistical analyses were performed using Fisher’s exact probability test and Welch’s t test. Survival rate from the date of initial surgery until death or loss of contact (cause-specific survival; CSS) and tumor recurrence (disease-free survival; DFS) were estimated by the Kaplan-Meier method. Statistical significance for survival was compared using the log-rank test. The candidate risk factors were compared by DFS and CSS in all patients. A p value <0.05 was considered statistically significant. All analyses were performed using JMP 5.1.1 statistical software (SAS Institute, Cary, NC, USA).
Results
The incidence of childhood PTC in patients <20 years was 1.5% (142 of 9,164 PTC patients underwent thyroidectomy between 1961 and 2005). The distribution of patients according to age and sex are shown in Fig. 1. A familial history of thyroid cancer in first-degree relatives was present in 12 of 142 patients (8.5%). At initial presentation, three patients had distant lung metastasis with gross neck LN metastasis and 30 had gross neck LN metastasis without other metastatic organs. All patients were treated with surgery (hemi/partial thyroidectomy in 45 patients, subtotal thyroidectomy in 85, total thyroidectomy in 12, no LN dissection in 50, central compartment dissection in 20, and modified radical neck dissection in 72). Postoperative external beam radiation therapy was administered to 59 patients. Postoperative radioiodine remnant ablation was not performed on any of the patients with a curative resection at the time of the initial surgery. The patients with lung metastasis at initial presentation underwent a total thyroidectomy following radioiodine therapy. Thyroid-stimulating hormone (TSH) suppression therapy was not administrated and the TSH level was maintained at a low normal level with or without l -thyroxine in all patients.
Table 1 gives the surgical procedures and postoperative complications. Hypoparathyroidism, including temporary hypoparathyroidism, was found in 12 patients (9.2%) and permanent hypoparathyroidism was found in 1 (0.7%). Recurrent laryngeal nerve palsy, including temporary recurrent laryngeal nerve palsy, was found in 17 patients (13.6%) and permanent recurrent laryngeal nerve palsy was found in 4 (2.9%). There was a significant increase in the incidence of postoperative hypoparathyroidism following total thyroidectomy compared to subtotal thyroidectomy (temporary, p < 0.001; permanent only, p = 0.007) and hemi/partial thyroidectomy (temporary, p < 0.001; permanent only, p = 0.051). Similarly, there was a significant increase in the incidence of postoperative laryngeal nerve palsy following total thyroidectomy compared to subtotal thyroidectomy (temporary, p < 0.001; permanent only, p = 0.020) and hemi/partial thyroidectomy (temporary, p = 0.006; permanent only, p = 0.005).
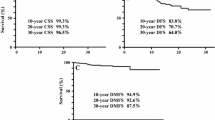
Recurrence was found in 28 (20%) of the 139 patients who underwent a complete operation. The recurrent sites were the neck LN in 25 patients, lung in nine, remnant thyroid in five, mediastinum LN in one, and others in three, including duplication. The patients with recurrence in the neck LN were resected surgically, and the patients with distant metastases in the lung and bone were treated with radioiodine therapy. During follow-up, three patients died of the disease and five patients died of other reasons. DFS and the CSS at 40 years were 74.1 and 97.5%, respectively (Fig. 2).
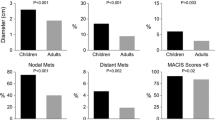
Significant differences in DFS were observed in patients <16 years (p = 0.030) and in those with a familial history of thyroid cancer (p = 0.041), preoperative gross LN metastasis (p = 0.006), tumor diameter >30 mm (p = 0.033), extrathyroidal invasion (p = 0.004), and histological LN metastasis (p = 0.002) (Fig. 3). Preoperative gross LN metastasis (p = 0.010) and distant metastasis at diagnosis (p < 0.001) were significant factors for CSS (Fig. 4). No other factors contributed to DFS and CSS (Table 2).
The clinical features of the children and adolescent groups are summarized in Table 3. The male/female ratio was 6/34 (1:5.7) in children and 11/91 (1:8.3) in adolescents. The female ratio tended to be higher in adolescents than in children, although it was not significantly different (p = 0.567). Furthermore, this sex difference was not observed in children <11 years (1:1.3). A familial history of thyroid cancer was observed more frequently in children (six patients, 15%) than in adolescents (six patients, 4.2%), but there was no significant difference (p = 0.097). Preoperative gross LN metastasis was found in seven children (42.5%) and 16 adolescents (15.7%; p = 0.002). Distant lung metastasis at diagnosis was found in three children (7.5%) in contrast to no adolescents (p = 0.021). The maximum tumor diameter was significantly larger in children (25.0 ± 2.7 mm) than in adolescents (18.0 ± 1.7 mm; p = 0.048). The incidence of a tumor with a maximum diameter >10 mm was significantly higher in children (85%) than in adolescents (55.9%; p = 0.001). Extrathyroidal invasion of the tumor was seen in 22 children (55%) and 41 adolescents (40.2%), and multifocal tumors were found in six children (15%) and ten adolescents (9.8%); however, these differences were not significant.
Discussion
Many risk factor analyses of patients with differentiated thyroid cancer have been reported [20–26]. Older age, male gender, familial history of thyroid cancer, tumor size, multifocal tumors, extrathyroidal invasion, LN metastasis, and distant metastasis are well-recognized prognostic risk factors in this field. Various prognostic scoring systems, e.g., TNM Staging System [22], AMES System [23], AGES and MACIS System [24, 25], and Ohio State University Scoring System [26], are determined by combining these factors. These risk factors and the scoring systems are based mainly on the results of adult patients with PTC, while childhood PTC accounts for only a small portion of the data. There are many controversies regarding the proper treatment of pediatric patients, and their long-term survival is excellent, but the risk of local recurrence is rather high.
Recent molecular analysis showed that PTC is caused by the activation of the MAP kinase pathway. In young patients, RET/PTC, AKAP9-BRAF, and NTRK1 recombination events are the main genetic alterations [27]. In contrast, PTC in adults is the result of predominantly point mutations, e.g., in BRAF [27–29]. The difference in oncogenic factor between children and adults may be related to their clinical cause. Identification of the prognostic indicators for PTC that are specific for children and adolescents, which are biologically different, is very important in deciding an appropriate therapeutic strategy.
In this article, we identified age (<16 years), familial history of thyroid cancer, preoperative gross neck LN metastasis, tumor diameter, and extrathyroidal invasion as risk factors for DFS in children and adolescents with PTC without a history of radiation exposure. Furthermore, preoperative gross neck LN metastasis and distant metastasis at diagnosis were significant risk factors for CSS. The patients with these CSS risk factors are considered to belong to a high-risk group and should be treated with total thyroidectomy and radioiodine therapy using I131. The extent of thyroid gland and LN resection was not associated with outcome, while wider resection, especially total thyroidectomy or near-total thyroidectomy, resulted in an increased rate of postoperative hypoparathyroidism. Our sample size may be inadequate to conclude a difference in these variables based on the extent of thyroidectomy. From our long-term survival data, childhood PTC shows a favorable prognosis and we select patients who are indicated for total thyroidectomy with radioiodine therapy from our childhood PTC patients. Our opinion is that stereotypical treatment of total thyroidectomy following radioiodine ablation should not be performed in all childhood patients.
This is the first report to compare the clinical features of childhood and adolescent PTC directly. A high prevalence of PTC in females was observed in both groups, but it was higher in adolescents. Notably, this sex difference was not seen in patients aged <11 years. Sex-related hormonal factors originating from unknown sex chromosome-related genes may contribute to this female preponderance of PTC.
Robinson and Orr [30] first reported familial nonmedullary thyroid cancer (FNMTC) in 1955. The incidence of FNMTC is reportedly 1.8–10.5% among nonmedullary thyroid cancers, but its incidence in childhood PTC is unknown [31–37]. In this series, a familial history of thyroid cancer was seen in 9.2% of patients and, specifically, the incidence of FNMTC was higher in children compared to adolescents. Genetic factors may be more involved with the occurrence of childhood PTC than adolescent PTC.
Preoperative gross neck LN metastasis, distant metastasis at diagnosis, and tumors with a maximum diameter >10 mm were found significantly more frequently in childhood PTC than in adolescent PTC. The diameter of childhood PTC tumors tended to be larger than that of adolescent PTC tumors. These results suggest that PTC in children may be a distinct clinical entity from PTC in adolescents and adults.
Conclusion
Children and adolescent PTC patients have an excellent prognosis, regardless of the extent of thyroidectomy and LN dissection. Preoperative neck LN metastasis and distant metastasis at diagnosis emerged as significant risk factors for CSS. We believe that children and adolescents without these risk factors should avoid the extent of thyroidectomy following postoperative ablative therapy.
References
Ceccarelli C, Pacini F, Lippi F et al (1988) Thyroid cancer in children and adolescents. Surgery 104:1143–1148
Fassina AS, Rupolo M, Pelizzo MR et al (1994) Thyroid cancer in children and adolescents. Tumori 80:257–262
Danese D, Gardini A, Farsetti A et al (1997) Thyroid carcinoma in children and adolescents. Eur J Pediatr 156:190–194
Segal K, Shvero J, Stern Y et al (1998) Surgery of thyroid cancer in children and adolescents. Head Neck 20:293–297
Dottorini ME, Vignati A, Mazzucchelli L et al (1997) Differentiated thyroid carcinoma in children and adolescents: a 37-year experience in 85 patients. J Nucl Med 38:669–675
Zimmerman D, Hay ID, Gough IR et al (1988) Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery 104:1157–1166
Pacini F, Vorontsova T, Demidchik EP et al (1997) Post-Chernobyl thyroid carcinoma in Belarus children and adolescents: comparison with naturally occurring thyroid carcinoma in Italy and France. J Clin Endocrinol Metab 82:3563–3569
Demidchik YE, Demidchik EP, Reiners C et al (2006) Comprehensive clinical assessment of 740 cases of surgically treated thyroid cancer in children of Belarus. Ann Surg 243:525–532
Baverstock KF (1993) Thyroid cancer in children in Belarus after Chernobyl. World Health Stat Q 46:204–208
Nikiforov Y, Gnepp DR, Fagin JA (1996) Thyroid lesions in children and adolescents after the Chernobyl disaster: implications for the study of radiation tumorigenesis. J Clin Endocrinol Metab 81:9–14
Tronko MD, Bogdanova TI, Komissarenko IV (1999) Thyroid carcinoma in children and adolescents in Ukraine after the Chernobyl nuclear accident: statistical data and clinicomorphologic characteristics. Cancer 86:149–156
Antonelli A, Miccoli P, Derzhitski VE et al (1996) Epidemiologic and clinical evaluation of thyroid cancer in children from the Gomel region (Belarus). World J Surg 20:867–871. doi:10.1007/s002689900132
La Quaglia MP, Corbally MT, Heller G et al (1988) Recurrence and morbidity in differentiated thyroid carcinoma in children. Surgery 104:1149–1156
Welch Dinauer CA, Tuttle RM, Robie DK et al (1998) Clinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents and young adults. Clin Endocrinol (Oxf) 49:619–628
Newman KD, Black T, Heller G et al (1998) Differentiated thyroid cancer: determinants of disease progression in patients <21 years of age at diagnosis: a report from the Surgical Discipline Committee of the Children’s Cancer Group. Ann Surg 227:533–541
Landau D, Vini L, A’Hern R et al (2000) Thyroid cancer in children: the Royal Marsden Hospital experience. Eur J Cancer 36:214–220
Jarzab B, Handkiewicz Junak D, Włoch J et al (2000) Multivariate analysis of prognostic factors for differentiated thyroid carcinoma in children. Eur J Nucl Med 27:833–841
Hay ID, Gonzalez-Losada T, Reinalda MS et al (2010) Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34:1192–1202. doi:10.1007/s00268-009-0364-0
Brink JS, van Heerden JA, McIver B et al (2000) Papillary thyroid cancer with pulmonary metastases in children: long-term prognosis. Surgery 128:881–886
Noguchi S, Murakami N, Kawamoto H (1994) Classification of papillary cancer of the thyroid based on prognosis. World J Surg 18:552–557. doi:10.1007/BF00353763
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
American Joint Committee on Cancer (2002) Chapter 8: thyroid. In: AJCC cancer staging handbook, 6th ed. Springer, New York, pp 89-98
Cady B (1998) Papillary carcinoma of the thyroid gland: treatment based on risk group definition. Surg Oncol Clin N Am 7:633–644
Schlumberger MJ, Filetti S, Hay ID (2002) Nontoxic goiter and thyroid neoplasia. In: Larsen RP, Kronenberg HM, Melmed S, Polonsky KS (eds) Williams textbook of endocrinology, 10th edn. Saunders, Philadelphia, pp 457–490
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1057
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Yamashita S, Saenko V (2007) Mechanisms of disease: molecular genetics of childhood thyroid cancers. Nat Clin Pract Endocrinol Metab 3:422–429
Lima J, Trovisco V, Soares P et al (2004) BRAF mutations are not a major event in post-Chernobyl childhood thyroid carcinomas. J Clin Endocrinol Metab 89:4267–4271
Penko K, Livezey J, Fenton C et al (2005) BRAF mutations are uncommon in papillary thyroid cancer of young patients. Thyroid 15:320–325
Robinson DW, Orr TG (1955) Carcinoma of the thyroid and other diseases of the thyroid in identical twins. AMA Arch Surg 70:923–928
Ron E, Kleinerman RA, Boice JD Jr et al (1987) Population-based case-control study of thyroid cancer. J Natl Cancer Inst 79:1–12
Hemminki K, Vaittinen P (1999) Familial cancers in a nationwide family cancer database: age distribution and prevalence. Eur J Cancer 35:1109–1117
Goldgar DE, Easton DF, Cannon-Albright LA et al (1994) Systematic population-based assessment of cancer risk in first-degree relatives of cancer probands. J Natl Cancer Inst 86:1600–1608
Stoffer SS, Van Dyke DL, Bach JV et al (1986) Familial papillary carcinoma of the thyroid. Am J Med Genet 25:775–782
Kraimps JL, Bouin-Pineau MH, Amati P et al (1997) Familial papillary carcinoma of the thyroid. Surgery 121:715–718
Lupoli G, Vitale G, Caraglia M et al (1999) Familial papillary thyroid microcarcinoma: a new clinical entity. Lancet 353:637–639
Hrafnkelsson J, Tulinius H, Jonasson JG et al (1989) Papillary thyroid carcinoma in Iceland. A study of the occurrence in families and the coexistence of other primary tumours. Acta Oncol 28:785–788
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enomoto, Y., Enomoto, K., Uchino, S. et al. Clinical Features, Treatment, and Long-Term Outcome of Papillary Thyroid Cancer in Children and Adolescents Without Radiation Exposure. World J Surg 36, 1241–1246 (2012). https://doi.org/10.1007/s00268-012-1558-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1558-4