Abstract
Background
Contemporary guidelines for managing PTC advise an approach wherein primary tumor and regional metastases (RM) are completely resected at first surgery and radioiodine remnant ablation (RRA) is restricted to high-risk patients, policies our group has long endorsed. To assess our therapeutic efficacy, we studied 190 children and 4242 adults consecutively treated during 1936–2015.
Subjects and methods
Mean follow-up durations for children and adults were 26.9 and 15.2 years, respectively. Bilateral lobar resection was performed in 86% of children and 88% of adults, followed by RRA in 30% of children and 29% of adults; neck nodes were excised in 86% of children and 66% of adults. Tumor recurrence (TR) and cause-specific mortality (CSM) details were taken from a computerized database.
Results
Children, when compared to adults, had larger primary tumors which more often were grossly invasive and incompletely resected. At presentation, children, as compared to adults, had more RM and distant metastases (DM). Thirty-year TR rates were no different in children than adults at any site. Thirty-year CSM rates were lower in children than adults (1.1 vs. 4.9%; p = 0.01). Comparing 1936–1975 (THEN) with 1976–2015 (NOW), 30-year CSM rates were similar in MACIS <6 children (p = 0.67) and adults (p = 0.08). However, MACIS <6 children and adults in 1976–2015 had significantly higher recurrence at local and regional, but not at distant, sites. MACIS 6+ adults, NOW, compared to THEN, had lower 30-year CSM rates (30 vs. 47%; p < 0.001), unassociated with decreased TR at any site.
Conclusions
Children, despite presenting with more extensive PTC when compared to adults, have postoperative recurrences at similar frequency, typically coexist with DM and die of PTC less often. Since 1976, both children and adults with MACIS <6 PTC have a <1% chance at 30 years of CSM; adults with higher MACIS scores (6 or more) have a 30-year CSM rate of 30%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In these changing times [1] of over-diagnosis [2, 3] and probable over-treatment [4] of the commonest endocrine malignancy, i.e., papillary thyroid carcinoma (PTC), institutional databases, with large numbers of patients being carefully followed for long postoperative periods, become valuable resources [5, 6] to determine whether increasing sophistication in diagnosis [7] and early treatment of both primary [8] and recurrent [9] diseases are actually leading to improved rates of cause-specific mortality (CSM) and tumor recurrence (TR) in children [10, 11] and in adults [12,13,14], whether in the majority with low-risk MACIS [15, 16] prognostic scores <6 or in the small minority with MACIS scores of 6 or more, who have a significant risk of dying from PTC.
The 2015 American Thyroid Association guidelines for PTC management in children [17] and adults [18] have recommended an individualized approach, where primary tumor and regional metastases (RM) are completely resected at first surgery and radioiodine remnant ablation (RRA) is selectively restricted to higher risk patients [19], as defined by either AJCC staging [20] or possibly MACIS prognostic scores [5, 15, 16, 19]. These principles have been endorsed by our multi-disciplinary group for more than 40 years [10,11,12,13,14,15,16, 19].
To assess the efficacy of our contemporary PTC management approach, we have studied 190 children and 4242 adults, consecutively treated at the Mayo Clinic in Rochester, Minnesota during the eight decades of 1936 through 2015, and have compared outcomes in a THEN cohort, treated during 1936–1975, with a NOW cohort, treated during the more recent four decades of 1976–2015. We had previously studied outcome using our Mayo Rochester Computerized Thyroid Cancer Database (MRCTCD) for the 1039 patients treated during the three decades of 1946–1975 [10], the 1500 patients treated during the four decades of 1945–1984 [13], the 1779 patients treated during the five decades of 1940–1989 [15], the 2444 patients treated during the six decades of 1940–1999 [14], as well as the 3595 patients [21] treated during the seven decades of 1940–2009.
Patients and methods
Records of all PTC patients undergoing definitive primary surgery at the Mayo Clinic in Rochester, Minnesota, during an 80-year period between January 1, 1936 and December 31, 2015 were reviewed. All relevant histologic slides were reviewed and classified according to current criteria of the World Health Organization [22] by Mayo staff pathologists and problematic cases were re-reviewed by specialist endocrine pathologists, principally, Professors Woolner, Goellner and Sebo [5, 10, 12,13,14,15].There were 4432 patients (2893 women, 142 girls, 1349 men and 48 boys) who had histologic confirmation of PTC and were treated within 60 days of the initial cytological or histologic diagnosis. The study protocol was approved by the Mayo Institutional Review Board; each patient (or parent in the case of the children) provided consent to participate in the follow-up study. Details of patients’ presentations, operative and pathologic findings, as well as adjunctive treatments, were obtained from the MRCTCD [5, 10,11,12,13,14,15, 21] maintained since 1984 by one of us (I.D.H.).
Follow-up information regarding the 2992 (68%) living patients was obtained either by Mayo Clinic re-examination or through correspondence with the home physician, patient, or family members. TR events at regional, local or distant sites were identified as per earlier publications [5, 12, 13, 23], and, like the recently published [24] National Thyroid Cancer Treatment Cooperative Study Group (NTCTCS) Registry Analysis [24], were characterized by “structural evidence of disease determined either radiologically or by pathology.” Since 1986 [5], we have recognized three types of TR with “differing prognostic implications” [12, 13]. These were (1) postoperative metastatic nodes, (2) local recurrences and (3) postoperative distant metastases. Only patients with metastatic nodes discovered in the neck or superior mediastinum more than 180 days after initial surgical treatment were considered to have postoperative metastatic nodes [12, 13]. A local recurrence [12] was diagnosed “if biopsy-proven tumor was discovered in the anterior aspect of the neck, other than in the lymph nodes, at any time after apparently complete surgical removal of the original tumor.” Distant metastatic lesions diagnosed no later than 30 days after operation were considered to be present at the time of the initial examination; those diagnosed more than 30 days postoperatively were considered new distant metastatic lesions. None of our recurrent events were based solely on persistently elevated levels of serum thyroglobulin. All recurrent events reported in earlier reports [10, 13,14,15, 21] were re-analyzed before consideration of inclusion in the present study. The MRCTCD has been funded annually since the time of our first publication on the 859 PTC patients treated during 1946–1970 [12] and, as the cohort of patients has expanded and is being continuously updated, all new TR events were added to the present database.
Death certificates were requested and examined for the patients who died as a result of PTC, as well as those who died from other causes of death; details of autopsy findings, if performed, were recorded in the database. All 4432 patients were followed in the database to death or last follow-up examination. The mean duration of follow-up for the 190 children (aged 18 or less) was 26.9 years (range 0.1–69.7 years) and for the 4242 adults was 15.2 years (range 0.1–69.2 years); total experience amounted to 69,699 patient-years of observation, as of August 21, 2017. Median follow-up for the 190 children was 24.5 years and for the 4242 adults was 10.9 years.
Survival rates from the date of initial surgery until death (all causes or cause-specific) or TR were estimated by the Kaplan–Meier method. Studies of mortality involved all 4432 patients, whereas studies of TR were confined to those 4245 patients (96%), who did not have distant metastases at presentation and underwent potentially curative complete tumor resection without postoperative gross residual disease. Comparisons of risk characteristics and trends across the decades were performed with Chi-squared test of proportion or the Fisher’s exact test, when necessary. The log-rank test was used to determine group differences in survival curves. All tests were two sided, with an alpha level of 0.05. All calculations were performed using SAS software. SAS and all other SAS Institute Inc product or service names are registered trademarks of SAS Institute Inc, Cary, NC, USA.
Results
Patient and tumor characteristics at presentation in children and adults
There were 190 children (aged 18 years or less at time of initial surgery) who were definitively treated for PTC at the Mayo Clinic in Rochester, Minnesota, during 1936–2015. The median age at diagnosis was 14 years (range 3–18 years). There were 142 girls (75%) and 48 boys, female: male ratio of 3:1. Mean tumor size was 2.56 cm in maximum diameter (median = 2.15 cm; range of 0.15–9.5 cm); 32 tumors (17%) were micro-cancers (maximum diameter of 1 cm or less). The histologic grade was 1 in 177 (93%) and 2 (of 4) in 13 (7%). DNA ploidy by flow cytometry was diploid in 44 (88%), tetraploid in 4 (8%) and aneuploid in 2 (4%) of 50 cases examined. Tumors were demonstrated to be multi-centric in 70 (37%) of 190 examined specimens. Altogether, 32 (17%) of the primary tumors at presentation were found at surgery to be locally invasive to extrathyroidal soft tissues and 9 (5%) had distant metastases found no later than 30 days after the date of the initial surgical procedure. In total, 143 children (75%) had metastatic involvement of regional lymph nodes at the time of initial surgery; in 120 specimens, where an accurate nodal number was available, there were 5 or less nodal metastases in 41 (34%) and 6–61 in 79 (66%). By Mayo risk-group classifications, the 190 children with PTC were classified as “low-risk” in 186 (98%) by the AGES [25] scoring system and in 172 (91%) by the MACIS [15] prognostic scoring system. Mean and median MACIS scores were 4.24 and 3.87, respectively (range of 3.16–9.32).
There were 4242 adults (aged more than 18 years at time of initial surgery) who were treated during 1936–2015. The median age at diagnosis was 48 years (range of 19–95 years).There were 2893 women (68%) and 1349 men (32%), female: male ratio of 2.1:1. Mean tumor size was 1.94 cm in maximum diameter (median = 1.5 cm; range of 0.08–15.0 cm); 1376 (32%) of tumors were micro-cancers (maximum diameter of 1 cm or less). The histologic grade was 1 in 3994 (94.1%), 2 (of 4) in 232 (5.5%) and 3 in 16 (0.4%). DNA ploidy by flow cytometry was diploid in 319 (77%), tetraploid in 48 (11%) and aneuploid in 49 (12%) of 416 cases examined. Tumors were demonstrated to be multi-centric in 1424 (34%) of 4242 examined specimens. Altogether, 396 (9%) of the primary tumors at presentation were found at surgery to have gross (macroscopic) extrathyroid invasion and 81 (2%) had distant metastases found no later than 30 days after the date of the initial surgical procedure. Totally, 1693 adults (40%) had metastatic involvement of regional lymph nodes at the time of initial surgery; in 4140 specimens, where an accurate nodal number was available, there were 5 or less nodal metastases in 1038 (25%) and 6–64 in 3102 (75%). By Mayo risk-group classifications, the 4242 adults with PTC were classified as “low-risk” in 3670 (86%) by the AGES [25] scoring system and in 3573 (84%) by the MACIS [15] prognostic scoring system. Mean and median MACIS scores were 4.81 and 4.45, respectively (range of 3.15–15.34).
Figure 1 compares six presenting features of PTC in the 190 children and the 4242 adults treated during 1936–2015. Tumors in children were larger (p < 0.0001), more often were grossly invasive (p < 0.001), and were more likely to be incompletely resected (p = 0.003). Moreover, at diagnosis, the children were much more likely to have metastasized to both regional (p < 0.001) and distant (p = 0.002) sites. Despite these adverse prognostic features, the MACIS scores were <6 (“low-risk”) in 91%, as opposed to 81% of adults (p = 0.02), likely explained by the much higher average age of the adults, contributing to a significantly higher A (for age) component of the MACIS [15] prognostic scores.
Comparisons of six presenting features (tumor size, extrathyroid invasion, incomplete resection, nodal metastases, distant metastases and MACIS scores <6) between the 190 children and the 4242 adults consecutively undergoing definitive treatment for PTC at the Mayo Clinic in Rochester, Minnesota during 1936–2015
Primary surgery, remnant ablation and last follow-up status
Bilateral lobar resection (BLR) was performed in 164 (86%) of the children and in 3725 (88%) of the adults; near-total or total thyroidectomy accounting for 154 (81%) in children and for 3140 (74%) in adults. Unilateral lobectomy with isthmusectomy was performed as a primary procedure in 23 (12%) of the children and 481 (11%) of the adults. Neck nodes were removed at initial surgery in 163 children (86%) and in 2801 adults (66%); compartmental dissection was carried out in 107 (66%) of the 163 children and in 1637 (58%) of the 2801 adults having neck nodes removed. Incomplete tumor resection with gross residual disease was reported after primary surgery in 12 (6%) of children and 113 (3%) of adults. There were 171 (90%) of the children and 4074 (96%) of the adults who underwent complete surgical resection and had no distant metastases on initial examination or within 30 days of the primary operation. Of these 4245 potentially curable patients, 57 (33%) of the children and 1221 (30%) of the adults had radioiodine remnant ablation within 6 postoperative months.
At last follow-up, 166 (87%) of the children and 2826 (67%) of the adults were alive. Overall survival rates (to all causes of death) at 20 and 30 postoperative years were 97 and 89%, respectively, for the 190 children, and 70 and 50%, respectively, for the 4242 adults. Disease-specific survival rates at 30 years for children and adults were 98.9 and 95.1%. At study conclusion, one child (0.5%) and 127 adults (2.9%) had died from papillary cancer, accounting for 4% of all causes of death in the childhood cohort and 9% of all deaths in the adult cohort treated during 1936–2015.
Tumor recurrence (TR) and cause-specific mortality (CSM) in children and adults
Figure 2 illustrates the TR rates through 30 postoperative years at local, regional and distant sites in the 171 children and the 4074 adults who had complete surgical resection and did not have initial distant spread. The majority of recurrences in both children and adults were in regional (neck) lymph nodes (middle panel); in both children and adults, the 30-year regional TR rates were identical at 16%. (p = 0.23). Despite children having more extensive disease at initial presentation, at none of the three sites (local, regional and distant) did the TR rates in children exceed those seen in comparably managed adults and 30-year TR rates were not significantly different at local (p = 0.69), regional (p = 0.23) or distant (p = 0.46) sites, when children and adults were compared.
Cumulative recurrence rates through 30 years after primary surgery at local (left panel), regional (middle panel) and distant (right panel) sites in the 171 children and 4074 adults, who were considered “potentially curable” (with complete surgical resection of primary tumor and without initial distant spread), i.e., were operated with “curative intent” for localized (intra-cervical) PTC
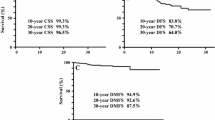
By contrast, there were significantly more deaths from PTC in adults than in children. Figure 3 (left panel) illustrates cumulative percent of children and adults dying from PTC through 30 postoperative years. At 20 years, there had been no cause-specific deaths in the children, but the 20-year CSM rate for adults was 2.9%; at 30 years, CSM rates for children and adults were 1.1 and 4.9%, respectively (p = 0.015). The difference in CSM rate was even more impressive between the 9 children and the 81 adults who had distant spread at initial presentation (Fig. 3, right panel). By 30 postoperative years, none of these 9 children had died. However, by 30 years, 41(51%) of adults with initial distant spread had died and the 20- and 30-year CSM rates were 63 and 72%, very significantly different from the observed outcome (0% CSM) observed in the 9 children (p = 0.002).
Comparisons of cumulative percent death rates from PTC during 30 postoperative years between the 190 children and 4242 adults treated for PTC during 1936–2015 (left panel) and also comparative cause-specific mortality (CSM) rates for those 81 adults and 9 children (right panel), who had distant spread at diagnosis and would be considered by current AJCC criteria [20] to be pTNM stage IV and II at presentation, respectively
Outcome in children and adults with MACIS low-risk (scores < 6) PTC tumors
We were interested in a comparison of outcome in MACIS <6 patients (representing 91% of children and 84% of adults), between the first four decades of the study (1936–1975) and the more recent four decades (1976–2015). We wished to determine whether either CSM or TR rates were significantly improved by the many “advances” introduced during the more sophisticated four decades of 1976–2015. For convenience, we chose to define the patients treated during 1936–1975 as the THEN cohort and those treated during 1976–2015 as the NOW cohort. Within the THEN cohort there were 72 children and 885 adults whose MACIS prognostic scores were <6 at presentation; within the NOW cohort there were 100 children and 2688 adults who had MACIS <6 (low-risk) scores [15]. Figure 4 compares CSM rates THEN and NOW over 30 postoperative years in these 172 children (left panel) and 3573 adults (right panel). Our 20-year CSM rate for MACIS low-risk patients at Mayo has historically been less than 1% [5, 13,14,15,16].For the NOW cohort, the 30-year CSM rate in 100 children (left panel) was 0% and in 2688 adults (right panel) was 0.7%. In neither children (p = 0.67) nor adults (p = 0.08) were the CSM rates significantly improved, when comparing the NOW (treated during 1976–2015) to the THEN cohort (treated during 1936–1975).
Figure 5 illustrates differences between the THEN and NOW cohorts with regard to the TR rates at regional (two left panels) and distant (two right panels) sites in 169 children (top two panels) and 3561 adults (bottom two panels) with potentially curative MACIS <6 PTC. With regards to postoperative distant metastases (right panels), there were no significant differences in cumulative TR rates, either in children (p = 0.07) or adults (p = 0.12), between the THEN and NOW cohorts over 30 postoperative years. By contrast, regional recurrence rates (left panels) were significantly higher, both in children (p < 0.001) and adults (p < 0.001) in the NOW cohort managed at Mayo since 1976. Indeed, in the NOW cohort, by 30 years regional recurrence rates approached 30% in adults and exceeded 50% in children.
Comparisons of cumulative recurrence rates during 30 postoperative years between the THEN and NOW cohorts of low-risk MACIS <6 PTC patients, with regards to recurrent events at regional (two left panels) and distant sites (two right panels), in 169 children (top two panels) and 3561 adults (bottom two panels) treated consecutively during 1936–2015 at the Mayo Clinic, Rochester, Minnesota with potentially curative intent
Figure 6 compares age, size, nodal metastases, gross invasion, incomplete resection and MACIS scores between the 884 adults in the THEN cohort and the 2690 adults in the NOW cohort with MACIS <6 PTC. Patients in the more recent (NOW) period of 1976–2015 are older, have smaller tumors and present with more nodal metastases at diagnosis, but their tumors are less often invasive and they are more often completely resected. However, the mean MACIS score in the THEN and NOW cohorts is identical (p = 0.32), probably refuting the notion of an alteration in tumor biology.
Comparisons of six presenting features (patient age, tumor size, nodal metastases, gross invasion, incomplete resection and mean MACIS score) between the 884 adults in the THEN cohort (treated during 1936–1975), who had low-risk MACIS <6 PTC, and the 2690 comparable adults treated more recently in the NOW cohort (1976–2015)
Figure 7 illustrates the timing of discovery of recurrences (at all sites) over 50 postoperative years in both the 169 children (upper panel) and the 3561 adults (lower panel), who had MACIS <6 PTC and had undergone potentially curative surgery (complete tumor resection and disease localized to neck). It is striking that recurrence rates, both in children and adults within the THEN cohort, are almost flat for the first 20 postoperative years, but rise steeply at 30, 40 and 50 postoperative years, perhaps related to being exposed to more intense tumor surveillance.
Comparisons of the cumulative recurrence rates (any site), during 50 postoperative years, between the THEN and NOW cohorts in either 169 low-risk MACIS <6 children (upper panel) or the 3561 low-risk MACIS <6 adults (lower panel) who had initial complete tumor resection for disease localized to the neck
Outcome THEN and NOW in adults with MACIS high-risk (scores 6+) PTC tumors
Similar to the format of Fig. 6 for MACIS <6 adults THEN and NOW, Fig. 8 compares age, size, nodal metastases, gross invasion, incomplete resection and MACIS scores between the 174 patients in the THEN cohort and the 494 patients in the NOW cohort with MACIS 6+ PTC. Patients in the more recent (NOW) period of 1976–2015 are older, have smaller tumors, present with fewer nodal metastases, are less often grossly invasive, and are more often completely resected. This may explain the significant (p = 0.02) lower mean MACIS score of 7.3 (median 6.8) seen in the 1976–2015 NOW cohort, as against the mean of 7.6 (median 7.1) observed in the THEN cohort.
Comparisons of six presenting features (patient age, tumor size, nodal metastases, gross invasion, incomplete resection and mean MACIS score) between the 174 adults in the THEN cohort (treated during 1936–1975), who had high-risk MACIS 6+ PTC, and the 494 comparable adults treated more recently in the NOW cohort (1976–2015)
Figure 9 compares the cumulative CSM rates during 30 postoperative years between the MACIS 6+ adult PTC patients treated during 1936–1975 (n = 174) and those 494 comparable patients treated in the more recent period of 1976–2015. In the 668 adult patients, representing the 16% minority with high-risk MACIS scores, the CSM rate at 30 years was 30% in the NOW cohort, significantly less (p < 0.001) than the comparable 47% rate seen with the THEN cohort. Figure 10 illustrates that this reduction in CSM is not reflected in a significant lowering of postoperative recurrence rates at local (p = 0.28), regional (p = 0.38) or distant (p = 0.62) sites in the 513 patients who had complete resection for localized disease. However, Fig. 11 demonstrates that, both for the 54 patients with distant spread at diagnosis and also for the 440 patients with localized disease treated during 1976–2015, there was an approximately 15% reduction in CSM (85 vs. 70% with distant spread: p = 0.011, and 41 vs. 25% with localized: p = 0.0004), when compared to the similar 25 and 149 MACIS 6+ patients in the THEN cohort.
Comparisons of cumulative recurrence rates over 20 postoperative years at local (left panel), regional (middle panel) and distant (right panel) sites between the 113 adults with MACIS 6+ PTC operated for potentially curative localized disease THEN during 1936–1975 and the comparable patients treated NOW during 1976–2015
Comparisons of cumulative CSM rates over 20 postoperative years between the THEN and NOW cohorts (treated during 1936–75 and 1976–2015, respectively), either in those 79 adults with high-risk MACIS 6+ PTC who had distant metastases at diagnosis (left panel) or in the 589 adults with high-risk MACIS 6+ PTC, whose presenting disease was localized to the neck
As compared to our original MACIS prognostic model [15], which was initially derived from a “training set” of 764 patients from a 1940–1964 cohort, we are now observing a significantly improved CSM outcome in the MACIS 6+ adult PTC group, and it would seem reasonable to “recalibrate” the cumulative CSM rates to be expected over 20 years in a more contemporary cohort of 3184 adult patients treated during 1976–2015. To that end, Fig. 12 illustrates the prediction of PTC death over 20 postoperative years by five MACIS prognostic risk groups with scores of 0–5.99, 6–6.99, 7–7.99, 8–8.99 and 9+ and 20-year cumulative CSM rates, respectively, of 0.6, 6.7, 23.2, 55.0 and 85.4% (p < 0.0001). Figure 13 illustrates the more familiar significant (p < 0.0001) differences in CSM seen between the 494 with MACIS high-risk scores (6+) and the 2690 with low-risk scores (<6), the 20-year CSM rates being 21.5% for high-risk and 0.6% for low-risk with a 20-year CSM (high-risk to low-risk) ratio [26, 27] of 35.8.
Cumulative CSM rates over 20 postoperative years in the NOW cohort of 3184 adult PTC patients, consecutively treated at the Mayo Clinic during 1976–2015, according to five MACIS prognostic risk groups with scores of 0–5.99, 6–6.99, 7–7.99, 8–8.99 and 9+ and with 20-year cumulative CSM rates, respectively, of 0.6, 6.7, 23.2, 55.0 and 85.4% (p < 0.0001)
Discussion
Almost 90 years ago, JJ Pemberton of the Mayo Clinic [28] commented that the “prevailing belief” in 1928 was that thyroid cancer was “incurable” and that “surgical measures are of little avail and may even be discouraged, whenever malignant disease can be diagnosed clinically.” Fortunately, attitudes about the surgical management of thyroid cancer have changed substantially during the ensuing years and Mayo authors, including surgeons, pathologists, endocrinologists and statisticians, have contributed regularly to this literature [5, 8,9,10,11,12,13,14,15,16]. Some 15 years ago, our group examined temporal trends in initial therapy and long-term outcome in 2444 consecutively treated PTC patients during six decades (1940–1999) and reported [14] in this journal that the 10-year rates for both mortality and recurrence were not significantly improved during the last five decades of the study, either for the low-risk majority with MACIS scores <6 or the high-risk minority with MACIS scores of 6+. We commented that “increasing use of RRA has not apparently improved the already excellent outcome achieved before 1970, in low-risk (MACIS < 6) patients managed by near-total thyroidectomy and conservative nodal excision.” In a recent debate entitled “Well differentiated thyroid cancer (WDTC): are we over-treating our patients?”, Nixon and Shah from MSKCC commented [6] that “only reports which are clinician collected, with a standardized approach to data collection, offer the level of detail required to interrogate subtleties such as the impact of therapy on outcome.” In a study of 2797 WDTC patients (87% PTC) managed during a 73-year period of 1932–2005 at MSKCC, they, like earlier authors, concluded [4] that “already excellent outcomes are unlikely to be significantly improved with an ever more aggressive approach to treatment.” Likely, these conclusions from two such “clinician collected” reports from single institutional cohorts influenced the less aggressive policies currently advocated in the 2015 ATA management guidelines for children and adults with differentiated thyroid cancer [17, 18].
We believe that this report describing initial presentation and long-term outcome in 4432 PTC patients treated during eight decades (1936–2015) is unique. The mean follow-up periods observed in children of 27 postoperative years and in adults of 15 years are unsurpassed. The recently published NTCTCS registry analysis [24] of 4348 PTC patients “contributed by 11 North American institutions with expertise in the treatment of patients with thyroid carcinoma” studied a cohort “diagnosed and registered” during 1987–2012 and, by contrast, had a median follow-up duration of only 6 years. This is our second study where we have compared children and adults with PTC managed by the same group of Mayo endocrine surgeons and followed by the same group of endocrinologists over decades. In the earlier study [10], published almost 30 years ago, we studied 58 children and 981 adults managed during 1946–1975, at a time when radio-immunoassay of thyroglobulin (Tg) was not available, high-resolution real-time neck ultrasound was yet to be invented, prophylactic central compartment dissection never considered and prognostic scoring yet in its infancy [25, 26]. Despite this lack of sophistication, we observed [10] that “survival (all causes of death) for both adults and children (with PTC) up to 30 years after the initial surgery was no different from expected survival rates. Only adults aged more than 40 years had a significantly higher mortality from PTC than did children (p < 0.0001).”
In this report, we again find that, when compared to adults, children with PTC had larger tumors and, at initial presentation, had more often metastasized to regional nodes and distant sites. In contrast to the smaller, earlier study [10], we found that children in this study were more likely to have gross extrathyroid invasion and more often had an incomplete primary tumor resection with gross residual disease. As before [10], we found that children almost never died of PTC and, if <1% developed distant spread, they were very likely to live with it, rather than die from it. Children had insignificantly fewer local recurrences and postoperative distant metastases, but in contrast to the earlier study, performed in an era without neck ultrasound, the higher neck nodal (regional) recurrence rates seen in children in the past has now been equaled by the adults, with the more than 15% rate seen in adults during 1936–2015 being now insignificantly different (p = 0.23) from the children, and approximately twice the 30-year rate of 7.8% seen in the earlier study of 1946–1975, in an era without neck ultrasound and with infrequent radioiodine use.
The year 2017 represents the 40th anniversary of the publication of Ernie Mazzaferri’s report [29] in Medicine (Baltimore), which promoted remnant ablation after total or near-total thyroidectomy for most PTC patients, changed practice worldwide [1] and prompted one of us (IDH) in 1990 to state [13] that “it is somewhat disconcerting if indeed the outcome of only 33 patients receiving radioiodine remnant ablation (RRA) should have so influenced the postoperative management of many thousands of papillary cancer patients subsequently treated at Mayo and other American as well as European centers.” Since it was in June 1976 that Mazzaferri presented his results to the Society of Nuclear Medicine, one might consider that the four decade period of 1976 through 2015 represents the era of the “rise and fall of remnant ablation.” In our own institution, if we consider the numbers of adult patients receiving RRA within 6 months of bilateral lobar resection for localized disease, the percent having RRA rose from 12% in 1971–1975 to 40% in 1976–1980, rose further to a peak of 67% during 1981–1985 and has fallen progressively to 26% during 2011–2015 (unpublished observations). The falling rates of RRA at Mayo are likely attributable to a better understanding of the natural history of treated PTC, as supplied by McConahey’s seminal study [12] published in 1986, and the realization that a selective use [19] for RRA in PTC could be enabled by restricting the use of RRA to the minority of PTC patients [16], who have high-risk disease with MACIS prognostic scores of 6 or more [15].
Perhaps relevant to some of our findings in relation to observed differences in outcome between patients treated during 1936–1975 and those from 1976 to 2015, would be a consideration of the contrasting styles of postoperative tumor surveillance employed in PTC patients THEN and NOW. Then (before 1976), an office visit typically consisted of no more than a history, neck palpation, ordering an occasional chest X-ray, checking a free thyroxine index and providing a script for ongoing levothyroxine therapy. Now (since 1976), an endocrinologist can choose from a remarkably expensive [28] menu of serum free T4, TSH and thyroglobulin (Tg) measured with ultrasensitive precision, bedside neck ultrasound, readily available ultrasound-guided biopsy, recombinant human thyrotropin (rhTSH) for injection and Tg stimulation, CT and MR imaging, and PET-CT, sometimes also enhanced by rhTSH.
Clearly, such sophistication in the early diagnosis of either primary or recurrent PTC comes at a huge price [30]. It has been estimated that the overall societal cost of WDTC care in the USA in 2013 was $1.6 billion, of which 41% was attributed to diagnosis, surgery and adjuvant therapy, while 37% was spent on “surveillance of survivors.” The same Harvard group estimated that the projected 2030 costs (in US 2013 dollars) for WDTC care, based on current incidence rates, could exceed $3.5 billion [30]. Similar gloomy predictions have previously been made regarding the financial consequence of “hunting for nonpalpable thyroid nodules” [31] during an era when “our ultrasound units are better, our biopsy techniques are improved, cytologic interpretation is refined, and we are essentially able to perform FNA on any lesion we can visualize.” Cronan [31] has stated that, “if we refuse to accept reality with regard to nonpalpable nodules, finances may well force us to reassess our directions.” He has estimated that if 150 million Americans have a thyroid nodule with a 10% rate of PTC, 15 million would merit surgery, and the financial costs for biopsy and surgery alone would conservatively reach 30 billion dollars. His recommendation, in order to prevent the “tsunami of thyroid nodules” from overwhelming the health care system, was that “it might well be better to turn off the ultrasound machines” [31]. Similar drastic changes in “surveillance of survivors” may be necessary if finding “small volume” locoregional recurrences in MACIS <6 PTC does not, as we have suggested, impact the CSM rates in such low-risk patients. Additionally, a future time of restricted funding may hopefully promote the publication of clinical guidelines that will direct clinical endocrinologists toward more cost-effective surveillance strategies. As Cronan has also recently stated, “from the patient perspective, we have hung the psychological stigma of cancer on these patients, the dependency for daily thyroid supplementation, and the continued need for follow-up in the absence of any data suggesting what to do long term. We accept all these consequences to control a cancer with a 99% 10-year survival…..our research focus should rather be toward the discovery of the small percentage of thyroid cancers that are aggressive and alter life spans.” [31].
The significant differences (p < 0.001) in regional recurrence rates seen NOW in both children and adults (Fig. 5) might be explained either by a change in tumor biology of the patients in the NOW cohort or, more probably, by the readily available ultrasensitive serum thyroglobulin measurements and the more widespread use of neck sonography now employed in more contemporary postoperative PTC surveillance [16,17,18]. The mean MACIS score in the THEN and NOW cohorts (Fig. 6) is identical (p = 0.32), probably refuting the notion of an altered tumor biology.
Additionally, Fig. 7 probably illustrates a phenomenon that perhaps could only be identified in a longitudinal study where follow-up can be reliably observed out as far as 50 postoperative years. The more recently treated NOW cohort is immediately exposed to the recently introduced, sophisticated but expensive, surveillance methods, and recurrence rates have by 30 years exceeded 50% in children and almost 30% in adults. It would appear that if the patients in the THEN cohort survive long enough to be exposed to the NOW technology, then recurrence rates will eventually approximate the high levels seen within the first 30 postoperative years in the NOW cohort. It seems likely that we are presently identifying recurrent disease much earlier in the postoperative period, but, obviously, MACIS <6 low-risk patients still survive 99% of the time, whether managed prior to 1976 or after that date, and despite the frequent discovery of recurrent/persistent disease, whether discovered postoperatively early or late.
The lack of improvement in either recurrence or CSM rates in MACIS <6 low-risk children and adults (Figs. 5 and 7) should not come as a surprise, especially in view of our multiple earlier reports [5, 14, 19] about the lack of impact of more aggressive initial therapy in low-risk PTC. The improved CSM in adults with high-risk MACIS 6+ PTC (Fig. 9) seen in the 1976–2015 cohort is not explained by a significant reduction in recurrence at local, regional or distant sites. However, the fact that the “high-risk” tumors in the NOW cohort are smaller, and less often have metastasized to regional and distant sites, may account in part for the improved outcome seen in association with the NOW patients whose MACIS “high-risk” scores are on average slightly lower (Fig. 8). Moreover, since these more recent cases were less often grossly invasive, this likely led to the lower frequency of incomplete resection seen in the NOW cohort. However, as Grant [8, 9] has recently advised [23], “it is well to remember Blake Cady’s keen insight into tumor biology and the interplay with surgical intervention” [32]. To paraphrase, “Biology is King; patient selection is Queen. Technical details of surgical procedures are the Princes and Princesses of the realm who frequently try to overthrow the powerful forces of the King and Queen, usually to no long-term avail….technical wizardry cannot overcome biological restraints.” Thus, the improved outcome observed in the MACIS 6+ NOW cohort may well be explained because the NOW cohort is “less high risk” than those in the THEN cohort.
The improved CSM in patients with initial distant spread (Fig. 11) treated during 1976–2015 cannot be attributed to more extensive neck surgery [8, 9], but perhaps owes more to distant metastatectomies [33] and more judicious use of radioiodine, external irradiation and, where appropriate, ablation with cryotherapy or radio-frequency. Where disease is localized to the neck, perhaps a combination of head and neck surgery and selective use of irradiation have averted deaths from involvement of the aerodigestive tract by tumors showing macroscopic extrathyroid extension.
Clearly, in MACIS <6 disease the excellent prognosis seen in times past continues but, with high-risk MACIS 6+ patients enjoying an improved outlook, it would seem timely (Figs. 12 and 13) to produce new data for a revised and more contemporary MACIS prognostic scoring system. In the “changing landscape” [1, 6, 34] of PTC observed in the past four decades, it seems even more desirable, as Nixon and Shah [4] have recently said that “leaders in the field must champion the need to stratify their patients by risk of recurrence and death. This risk prediction should not only be used to counsel patients, but to tailor the approach to therapy. The era of total thyroidectomy, central neck dissection and RAI for all has ended, as the features of patients who can safely be managed with conservative therapy have been defined.” With our colleagues from MSKCC [4], we certainly would also agree when they express the hope that “the epidemic of thyroid cancer which is being experienced in the developing world will bring with it resources to manage the demand. It is vital that these resources are not squandered on the over-treatment of low-risk patients, but targeted at those patients with high-risk disease, for whom curative therapy still remains elusive.”
Conclusions
Firstly, children, despite presenting with more extensive PTC than adults, recur at no greater frequency, die less often from PTC and usually coexist with distant spread. Secondly, CSM in MACIS <6 children and adults has not substantially improved since 1976, despite more rapid detection and prompt treatment of recurrences. Some might consider the recent increase in locoregional recurrence rates seen in MACIS low-risk patients, and likely caused by increased neck ultrasound scanning [31], to be a regrettable and expensive trend. Finally, CSM in adults with MACIS high-risk PTC (with scores of 6+) is improving and one wonders whether endocrine surgeons or perhaps, even radiation oncologists, are more likely responsible for this trend, rather than diagnostic radiologists or clinical endocrinologists. Alternatively, the improved CSM observed in the more recently treated MACIS 6+ adult cohort may be explained because the NOW cohort may be biologically “less high risk” than those in the THEN cohort.
Therefore, in an era, formerly of “affordable care,” does one really expect that the USA and its insurance providers can continue to justify funding the present obsession of clinical endocrinologists with “super-sensitive” serum thyroglobulin levels and tiny neck nodal targets seen only by high-resolution sonography [35]? Perhaps only the next 4 or 8 years of ever-changing health policies [34] in the USA will provide the final answer to this relevant and timely question for patients with this most common endocrine malignancy and their physicians.
References
Sitges-Serra A (2014) Low-risk papillary thyroid cancer: times are changing. Expert Rev Endocrinol Metab 9(1):9–18
Davies L, Morris LG, Haymart M et al (2015) AACE and ACE disease state clinical review: the increasing incidence of thyroid cancer. Endocr Pract 21(6):686–696
Vaccarella S, Franceschi S, Bray F et al (2016) Worldwide thyroid cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med 375(7):614–617
Nixon IJ, Shah JP (2014) Well differentiated thyroid cancer: are we over treating our patients? EJSO 40:129–132
Hay ID, McConahey WM, Goellner JR (2002) Managing patients with papillary thyroid carcinoma: insights gained from the Mayo Clinic’s experience of treating 2,512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc 113:241–260
Nixon IJ, Ganly I, Patel SG et al (2012) Changing trends in well differentiated thyroid carcinoma over eight decades. Int J Surg 10(10):618–623
Kiernan CM, Whiteside MA, Solorzano CC (2017) Cancer registries: can we improve the quality of thyroid cancer data? Ann Surg Oncol 24(5):1202–1207
Grant CS, Stulak JM, Thompson GB et al (2010) Risks and adequacy of an optimized surgical approach to the primary surgical management of papillary thyroid carcinoma treated during 1999–2006. World J Surg 34(6):1239–1246. doi:10.1007/s00268-009-0307-9
Onkendi EO, McKenzie TJ, Richards ML et al (2014) Reoperative experience with papillary thyroid cancer. World J Surg 38(3):645–652. doi:10.1007/s00268-013-2379-9
Zimmerman D, Hay ID, Gough IR et al (1988) Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients treated at one institution during three decades. Surgery 104:1157–1166
Hay ID, Gonzalez-Losada T, Reinalda MS et al (2010) Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34(6):1192–2002. doi:10.1007/s00268-009-0364-0
McConahey WM, Hay ID, Woolner LB et al (1986) Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy and outcome. Mayo Clin Proc 61:978–996
Hay ID (1990) Papillary thyroid carcinoma. Endo Metab Clin N Am 19(3):545–576
Hay ID, Thompson GB, Grant CS et al (2002) Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 26:879–885. doi:10.1007/s00268-002-6612-1
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1,779 patients surgically treated at one institution during 1940 through 1990. Surgery 114:1050–1058
Hay ID (2007) Management of patients with low-risk papillary thyroid carcinoma. Endocr Pract 13(3):521–533
Francis GL, Waguespack SG, Bauer AJ et al (2015) Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroid 25(7):716–759
Haugen BR (2017) 2015 ATA management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer; what is new and what has changed? Cancer 123(3):372–381
Hay ID (2006) Selective use of radioactive iodine in the postoperative management of patients with papillary and follicular thyroid carcinoma. J Surg Oncol 94(8):692–700
Edge SB, Byrd DR, Compton CC et al (2010) AJCC cancer staging manual, 7th edn. Springer, New York, pp 67–74
Hay ID, Johnson TR, Thompson GB et al (2016) Minimal extrathyroidal extension in papillary thyroid carcinoma does not result in increased rates of either cause-specific mortality or postoperative tumor recurrence. Surgery 159(1):11–19
LiVolsi VA, Albores-Saavedra J, Asa SL (2004) Papillary thyroid carcinoma. In: DeLellis RA, Lloyd RV, Heitz PU, Eng C (eds) Pathology and genetics of tumours of endocrine organs: WHO classification of tumours. IARC Press, Lyon, pp 57–66
Grant CS (2015) Recurrence of papillary thyroid carcinoma after optimized surgery. Gland Surg 4:52–62
Carhill AA, Litofsky DR, Ross DS et al (2015) Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J Clin Endocrinol Metab 100:3270–3279
Hay ID, Grant CS, Taylor WF et al (1987) Ipsilateral lobectomy versus bilateral lobar resection in papillary thyroid carcinoma: a retrospective analysis of surgical outcome using a novel prognostic scoring system. Surgery 102:1088–1094
Cady B (1997) Our AMES is true: how an old concept still hits the mark: or, risk group assignment points the arrow to rational therapy selection in differentiated thyroid cancer. Am J Surg 197:462–468
Cady B (1998) Papillary carcinoma of the thyroid gland: treatment based on risk group definition. Surg Clin N Am 7:633–644
Pemberton JJ (1928) Malignant disease of the thyroid gland: a clinical consideration. Ann Surg 87:369–377
Mazzaferri EL, Young RL, Oertel JE et al (1977) Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore) 56:171–196
Lubitz CC, Kong CY, McMahon PM et al (2014) Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer 120:1345–1352
Cronan JJ (2008) Thyroid nodules; is it time to turn off the US machines? Radiology 247:602–604
Cady B (1978) Basic principles in surgical oncology. Presidential address. Arch Surgery 132:338–346
Porterfield JR, Cassivi SD, Wigle DA et al (2009) Thoracic metastatectomy for thyroid malignancies. Eur J Cardiothorac Surg 36:155–158
Lubitz CC, Sosa JA (2016) The changing landscape of papillary thyroid cancer: epidemiology, management, and the implications for patients. Cancer 122:3754–3759
Dominguez JM, Nilo F, Contreras T et al (2017) Neck sonography and suppressed thyroglobulin have high sensitivity for identifying persistent/recurrent disease with low-risk thyroid cancer treated with total thyroidectomy and radioactive iodine ablation, making stimulated thyroglobulin unnecessary. J Ultrasound Med. doi:10.1002/jum.14260 (Epub ahead of print)
Acknowledgements
The documentation from one institution of 70,000 patient-years of PTC experience has required the cooperation of many Mayo Clinic colleagues and the support of the lead author’s wife, Professor Eileen Hay. Dr. Hay is particularly indebted to the late Drs. McConahey, Taylor and Woolner for initiating the careful documentation of outcome in the 1946–1970 cohort of PTC patients. This present study was supported by generous financial contributions from the Dr. RF Emslander Professorship, Colin V. and Brenda Reed from Nashville, TN, and the William Stamps Farish Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hay, I.D., Johnson, T.R., Kaggal, S. et al. Papillary Thyroid Carcinoma (PTC) in Children and Adults: Comparison of Initial Presentation and Long-Term Postoperative Outcome in 4432 Patients Consecutively Treated at the Mayo Clinic During Eight Decades (1936–2015). World J Surg 42, 329–342 (2018). https://doi.org/10.1007/s00268-017-4279-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4279-x