Abstract
Selection of the most appropriate treatment to obtain the best results with the lowest rate of recurrence and minimal morbidity and mortality is mandatory for the management of hepatic hydatid disease. The surgical approach is the mainstay of treatment, and there has been a tendency toward laparoscopic surgery and, more recently, percutaneous treatment (PT), which has become increasingly popular with revolutions in techniques. We aimed to evaluate the results of current therapeutic methods in the context of a 10-year single-institution experience. Between 1992 and 2003, 355 patients with 510 hydatid cysts of the liver were treated by open operation, laparoscopic surgery, or PT. The series included 128 females and 227 males ranging in age from 10 years to 73 years. Preferred treatment modalities, perioperative complications, interventions, recurrences, and length of hospital stay were retrospectively analyzed. There were two postoperative deaths (1.08%) in the open surgery group. Biliary leakage was observed in 28 patients treated with open surgery, in 10 patients after PT, and in 2 after laparoscopic treatment. Recurrence rates were 16.2%, 3.3%, and 3.5% after open surgery, laparoscopic surgery, and percutaneous treatment, respectively. Characteristics of the cyst, presence of cystobiliary communications, and the availability of a multidisciplinary team are the factors that we believe directly affect the results. Radical surgery can be done safely for suitable cases; conventional procedures are associated with greater morbidity. Laparoscopic surgery seems effective and safe, with low morbidity and recurrence rates for type I–III cysts in accessible localizations. Our experience with PAIR (puncture, aspiration, injection, and reaspiration) and catheterization provides evidence that the procedure is an effective and safe option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hydatid disease is still frequent in endemic areas. Approximately 50%–70% percent of the cysts are localized in the liver.1 The right lobe is affected in 85% of patients, and in one quarter to one third of cases the cysts are multiple. The second most frequent site is the lungs, accounting 20%–30% percent of all cysts; less frequently, the spleen, kidneys, heart, bones, central nervous system, and other organ systems are affected.2 Despite its benign outcome, management of the disease presents a dilemma for surgical clinics because of the high complication and recurrence rates, which lead to prolonged hospitalization.3 Because of the limited efficacy of systemic chemotherapy, the surgical approach to treatment has been accepted as the gold standard for the management of hydatid disease, and radical surgical resection has been proposed as a safe and very effective technique with an almost nil recurrence rate.4 Parallel to the progress in laparoscopic techniques during the last decade, laparoscopic treatment of hepatic hydatid disease has been increasingly popular since 1992.5,6 Furthermore, a perforator-grinder-aspirator (PGA) apparatus specifically designed for the evacuation of hydatid cysts has been developed and is used in many centers.7,8 Improvements in interventional or radiological techniques have also permitted percutaneous treatment (PT), which is especially useful in patients who cannot or do not want to undergo surgery. Prospective randomized studies have shown that combining PT with administration of albendazole is an effective and safe alternative to surgery for the treatment of uncomplicated hydatid cysts of the liver.9–11 With all kind of approaches, the primary goals are to avoid spillage of the cyst contents into the peritoneum and thus prevent anaphylaxis and dissemination and to neutralize and evacuate the entire germinal lining and thus prevent recurrence.
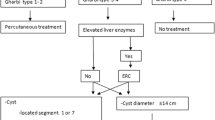
Even with the greatest care in the management of hepatic hydatid disease, recurrence issue has been one of the main problem, and it is mainly related to the spillage of cyst content.12 The morphological appearance of liver hydatid disease has been classified into five types by Gharbi et al.,13 based on the sonographic analysis of the morphology and structure of the cyst by ultrasonography (US). This classification is also recommended for planning treatment and evaluating therapeutic efficiency.14 Type I and II (pure fluid collection and fluid collection with a split wall), some subtypes of the type III (fluid collection with septa) that do not involve nondrainable solid material, and infected hydatid cysts were accepted as candidates for percutaneous treatment. Type III, type IV (hydatid cysts with heterogeneous echo pattern), and liver cysts that ruptured into the biliary system or peritoneum were widely accepted for surgical approaches. It is generally accepted that type V hydatid cysts (those with reflecting thick walls) do not need any intervention.15
Our institution has a patient population that consists primarily of young male soldiers and their relatives who come from many endemic areas of the country. Surgical approaches with various techniques have typically been the recommended treatment in the department up until 1992, when the PT and laparoscopic approaches began to be used as the preferred treatment in many selected cases. In this study, we retrospectively evaluated the results of the different treatment modalities with regard to postoperative morbidity, management of complications, and recurrence during the last 10 years. Safety and effectiveness of noninvasive techniques in uncomplicated cysts is also discussed, and the relation between cyst content and postoperative outcomes such as biliary leakage, biliary fistula, cavity infections, and postoperative hospitalization is examined for the patient population treated during the 10 years ending in 2003.
MATERIALS AND METHODS
This study consisted of 355 patients with 510 hydatid cysts of the liver treated by conventional open or laparoscopic surgery and percutaneous treatment in the Departments of Surgery and Radiology between 1992 and 2003. There were 128 females and 227 males ranging in age from 10 to 73 years (mean: 35.2 ± 13.3 years). Medical records of the patients were analyzed according to the following parameters: age, sex, location and the type of cysts diagnosed by radiographic imaging, preferred treatment modalities, perioperative complications, interventions, recurrences, and length of hospital stay. Patients were given a detailed explanation about the procedures and written informed consent was taken prior to procedures. Patients were classified into three groups according to treatment modalities as open, laparoscopic, and percutaneous approach, respectively. The baseline characteristics of the patients in all treatment groups are shown in Table 1.
After completing the perioperative treatment, patients were followed periodically in the third, sixth, and twelfth postoperative months in the first year and at least once a year thereafter. The follow-up procedure included physical examination, serologic tests, ultrasonography of the abdomen, and computerized tomography (CT) in particular cases. Manifestations such as reappearance of live cysts at the site of a previously treated cyst or the appearance of new extrahepatic disease resulting from procedure-related spillage were considered as local recurrence.16
Surgical Procedure for Open Approach
With open surgery the abdomen was exposed through a right subcostal incision, and the abdominal viscera were examined for potential sites of dissemination. The area around the cysts was packed with swabs soaked with hypertonic sodium chloride solution as a scolecidal agent. The cyst was punctured and the cyst content was aspirated with a 16-gauge needle connected to a 50-ml syringe through a three-way stopcock; the aspirate was replaced with the scolecidal agent. Then the protruding dome was incised and the hydatic fragments, including the laminated membrane, were removed with a sponge-holding forceps. The residual cavity of the cyst was scrubbed with swabs soaked with povidone-iodine and carefully inspected for biliary communication. Any visible fistulas were sutured with nonabsorbable sutures. Cavities were drained with tubes and an additional subhepatic drain was placed in all cases to control biliary leakage. Drains were removed on the fifth to seventh postoperative days, and a cavogram was usually obtained before the removal of the tube in order to rule out biliary communication. Patients with prolonged drainage were considered to have biliary fistulas.
Open surgical procedures were classified as radical for any type of liver resection and cystectomy. Partial cystectomy with either tube drainage, capitonnage, or omentoplasty were considered conservative approaches as described elsewhere.17,18 Cholecystectomy and intraoperative cholangiography was performed and choledochotomy with T-tube drainage was preferred in patients with obstructed common bile duct (CBD). Roux-en-Y cystojejunostomy was preferred in two patients with cysts so large that obliteration of the remaining cavity was considered impossible.
Surgical Procedure for Laparoscopic Approach
The laparoscopic procedure was begun with the establishment of pneumoperitoneum with carbon dioxide, after which the abdominal cavity was carefully explored and cysts were identified. Three to four trocars were required for each operation according to cyst locations. A long, 10/12-mm trocar (ENDOPATH, Ethicon Endo-Surgery) was introduced from a point as close as possible to the cyst, and two long strip of gauze soaked with hypertonic sodium chloride solution as a scolecidal agent were placed around the cyst. The cyst was then punctured with a 14-gauge 120-mm insufflation needle and the cyst content was rapidly aspirated. At that moment, an additional aspirator tip was placed close to the puncture point to avoid spillage of cyst contents. The cyst cavity was then nearly filled with hypertonic sodium chloride solution for irrigation, which was left in the cavity for 5–10 minutes. In the next step, the cyst wall was opened and the endocyst was evacuated into a specimen-retrieval bag with careful observation of the separation from pericyst. The cystic cavity was re-irrigated with hypertonic saline and the telescope was introduced into the cavity to explore for potential biliary openings and retained daughter cysts. The procedure was completed with partial unroofing, and closed-suction drains were placed into the cysts with subhepatic or perihepatic drains.
Procedure for Percutaneous Treatment
According to the sonographic type of the cyst or cysts as described by Gharbi et al.,13 patients with type I hydatid cysts (pure fluid collection), type II hydatid cysts (fluid collection with a split wall), and type III hydatid cysts (fluid collection with daughter cyst) with drainable matrices were included for the procedure. Patients with type III cysts containing nondrainable degenerated matrices due to solid components (fluid collections with septa), type IV cysts (heterogeneous echo pattern), or type V cysts (reflecting calcified wall) were excluded. Patients with ruptured (into the biliary tract, peritoneum, or pleural cavity) or secondarily infected cysts and 7 patients who had not attended to follow-up sonographic examinations were also excluded.
Every patient received prophylactic oral albendazole (Andazol; Biofarma, IST, Turkey), 15–20 mg/kg twice a day starting one week before the procedure and continued for 4 weeks. The technique of the procedure was chosen mainly according to the size of the cyst. Cysts smaller than 6 cm (n = 164) were treated with puncture, aspiration, injection, and reaspiration (PAIR), a technique developed and described by Ben Amor et al. 19 Cysts larger than 6 cm (n = 69) were treated with the catheterization technique described by Akhan et al. 20 The PAIR technique initiated with the puncture of the cyst with a 19-gauge sheathed needle under sonographic guidance and approximately half of the cyst volume aspirated; this was followed by injection of hypertonic saline solution (20%) amounting to one third of the initial estimated cyst volume. The cyst fluid was reaspirated after a 20-minute waiting period. The catheterization technique differs from the PAIR technique. After injection of the hypertonic saline solution, a 6- to 9-French pigtail catheter is placed into the cavity for 24 hours of gravity drainage. If cystographic study through the pigtail catheter shows no communication between the cyst cavity and the biliary tract, a volume of absolute alcohol half the initially estimated volume of the cyst is applied for 20 minutes to produce protoscolecidal and sclerosing effects. If, however, cystographic study through the pigtail catheter shows communication with the biliary tract, alcohol should not be used because secondary sclerosing cholangitis may result.
To avoid spillage of cyst fluid at the time of the initial puncture since the pressure is high inside of hydatid cysts, a one-way valve system was adapted to the top of a 19-gauge sheathed needle, and this type of needle was used in all patients.
Data Analysis
Results are reported as median and percent. Differences between groups were tested for significance by the Kruskal-Wallis test and the chi-squared test. The results were analyzed with a Bonferroni adjusted Mann-Whitney U-test for comparison of subgroups. Differences were considered significant at P < 0.05. The SPSS (version 10.0-Windows; SPSS Inc; Chicago, IL) software program was used for statistical analysis.
RESULTS
There were two postoperative deaths in the open surgery group (mortality 1.08%), of patients who underwent operation to treat spontaneous cyst ruptures. The first patient, a 71-year-old woman with chronic obstructive lung disease and positive serology for hepatitis C virus, died of pulmonary failure on postoperative day (POD) 12. The second patient who died, a 21-year-old man with cryptogenic cirrhosis diagnosed with perioperative liver biopsy, occurred on POD 25 as a result of fulminant hepatic failure. There were no deaths in the laparoscopic and percutaneous treatment groups. Types of operations and postoperative morbidity results are summarized in Table 2, and morbidity results with reference to cyst type and locations are given in Table 3. Mortality rates, length of postoperative hospital stay, and recurrence rates are presented in Table 4.
Fifty-eight patients (32 in the open surgery group and 26 in the PT group) had previously undergone operation for hydatid disease, 49 for cysts in the liver, 6 for pulmonary disease, and 3 for synchronous liver and pulmonary disease. Fourteen patients previously treated with PT had open surgery for recurrence (5 patients) and post-residual cavity that was misconstrued as recurrence (9 patients).
Preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed in 16 patients in the open surgery group, all of whom presented with jaundice, acute cholangitis, and possible cystobiliary communication. Combined ERCP and sphincterotomy successfully relieved the symptoms in 10 patients, and no further interventions were required during surgery. For the remaining 6 patients, cholecystectomy and intraoperative cholangiography were performed and choledochotomy with T-tube drainage was preferred in 4 out of 6 patients. These 4 patients had obstructed common bile duct (CBD). Biliary communications with visible fistulas were sutured intraoperatively with nonabsorbable sutures in 36 patients. Sutures were placed on sclerotic tissues in most cases and on healthy biliary tissue after a perifistulary pericystectomy in limited number of cases. Postoperative biliary leakage was observed in 28 patients (15.1%) treated with open surgery. In most cases leakage resulted from partial cystectomy ± drainage procedure (20 patients).
Management with prolonged tube drainage was successful in 16 patients with spontaneous closure of the fistulas. Postoperative sphincterotomy with or without nasobiliary drainage catheter was required in the remaining 12 patients who had high-output (> 300 ml bile/day) bile fistulas. A nasobiliary drainage catheter was kept in place until the drainage ceased.
There were only 2 patients with biliary fistula after laparoscopic treatment, and the fistula resolved spontaneously after prolonged drainage for 24 and 27 days, respectively. Biliary fistula occurred in 10 patients after the PT procedure. Combined ERCP and endoscopic papillotomy with prolonged percutaneous catheterization (longest 39 days) was successful in 6 of 10 patients with cystobiliary fistula. Four patients eventually required surgery for the management of biliary fistula. Postoperative infection and abscess in the cyst cavity occurred in 8, 2, and 3 patients from the open, laparoscopic, and percutaneous treatment groups, respectively. Percutaneous drainage was effective in 3 patients in whom abscesses occurred after removal of the drains placed during open surgery. Treatment with antibiotics was satisfactory in 5 patients from the open surgery group and in 2 patients from the laparoscopic group, who already had a drain in the cyst cavity. Two patients who had partial cystectomy + drainage procedure developed liver abscess after discharge from the hospital. Both patients required re-operation for management of the abscess. The cyst cavity became infected in three patients treated by the PAIR technique 9, 11, and 12 days after the procedure; all required percutaneous catheter drainage for 5–8 days plus antibiotics. Re-operation was needed in one patient who had postoperative bleeding following a radical procedure for the cyst. Thirty-two patients from the open surgery group and 2 patients from the laparoscopic surgery group had concomitant cholecystectomy because of cholelithiasis, location of the cysts, or a need for intraoperative cholangiography screening. Two patients who had cysts in the spleen required splenectomy as part of the surgical intervention.
The mean follow-up period was 57.4 months (median: 35, range: 13–62 months), 14.7 months (median: 11, range: 8–22 months), and 51.1 months (median: 32, range: 5–58 months) in the open, laparoscopic, and percutaneous treatment groups, respectively. The hospitalization period was 12.5 ± 5.4 days (median: 12, range: 5–43 days) for the open surgery group, 9.9 ± 6.2 days (median: 8, range: 4–30 days) for laparoscopic surgical treatment, and 2.3 ± 7.5 days (median: 1, range: 1–73 days) for percutaneous treatment.
Biliary fistula was the most important factor leading to long hospital stay in our study. The appearance of new active cysts after primary intervention in the liver or in extrahepatic locations, defined as “recurrent disease,” was seen in 30 patients (16.2%) from the open surgery group, 1 patient (3.3%) from the laparoscopy group, and 5 patients (3.5%) from the PT group. Recurrences were most frequently seen after the partial cystectomy + drainage procedure (22 patients) and particularly after partial cystectomy + omentoplasty (4 patients) or partial cystectomy + capitonnage (4 patients).
DISCUSSION
Hydatid cyst is a parasitic disease caused by the tapeworm Echinococcus granulosus; accidental ingestion of tapeworm eggs causes infestation in humans. The disease is frequently encountered in endemic areas of Mediterranean countries, New Zealand, Australia, North America, South America, Central America, and Asia .21 A large series of retrospective multicenter studies for hydatid cyst of the liver indicated that the most frequent clinical patterns were uncomplicated cysts (82%), cysts that had ruptured into the biliary tract with a large biliocystic fistula of more than 5 mm (12%), and cysts involving the thorax (2.2%); the remaining patients had other, rare complications.22
The desired goals in the treatment of hepatic hydatid disease include complete elimination of the parasite and prevention of recurrent disease with minimum morbidity and mortality. Selection of the most appropriate treatment to achieve those goals depends on the condition of the patient, the nature of the cyst(s) considering number, size, location, and presence of cystobiliary communications, and the availability of an experienced surgeon and interventional radiologist. The patient-related factors include age, pregnancy, patient preference, and associated diseases that preclude surgical intervention. Before any therapeutic intervention, the nature of the cyst(s) should be classified based on ultrasound (US) images, and CT screening must be done to provide necessary information. The size, number, and location of the cyst(s) and the nature of the cyst contents, as well as any associated complicating factors will then guide the therapeutic decision-making process.
Therapeutic modalities range from systemic chemotherapy to conventional or laparoscopic surgical interventions to percutaneous drainage with or without medical therapy. Surgery remains the cornerstone of the treatment for hepatic hydatid cysts, whether radical or conservative. However, drug treatment with percutaneous drainage is recommended as a good alternative to surgery, especially in selected patients with non-complicated cysts and patients who have contraindications for surgery.3,11
The radical surgical procedures include hepatic resection, and more frequently pericystectomy. The most widely performed conservative surgical techniques include unroofing, simple drainage, closure of the edges (capsulorrhaphy) of the residual cavity without drainage, capitonnage, furrowing the margins of the cavity by “introflexion,” or omentoplasty in the residual cavity. Surgery may be performed by a conventional open approach or a laparoscopic approach. To date, however, there are no randomized clinical trials comparing laparoscopic treatment with conventional open treatment. Marsupialization has been abandoned by most centers because of the high complication rates of the procedure.18,21
Our retrospective study represents a 10 years of institutional experience of hydatid disease of the liver with multidisciplinary approach. Until 1992, conventional surgical techniques had been the recommended treatment in the department, whereas PT and laparoscopy have since been preferred as alternative treatments in many selected cases since then.11,23,24
Postoperative mortality in our series was 1.08% in the open surgical group. Although higher mortality rates (27%–32.5%) have been reported by Moreno et al., many studies have shown lower results, ranging between 0 and 3%.3,25–31 Zaouche et al.,22 reported a 4.5% mortality rate in a large multicenter study including 244 patients with hepatic cysts of the liver complicated with a large biliocystic fistula. They observed that all deaths occurred after conservative surgery. It has been generally accepted that performing radical surgery for a benign disease may increase the operative risk, but that conservative procedures are safer and easier to perform. However, the results reported by Zaouche et al.,22 indicate that morbidity is more prevalent after conservative surgery and that the major causes of operative complications are comorbidities related to patient age, abscess formation in the remaining cyst cavity, and presentation with perforated cysts.
The preoperative detection and the management of biliocystic communication is one of the most important issues in the treatment of hydatid cysts of the liver because such cysts are usually associated with higher morbidity and mortality. Endoscopic retrograde cholangiopancreatography can be used as a diagnostic and therapeutic approach in the management of biliocystic communication. Preoperative ERCP sometimes shows the biliocystic fistula and defines the biliary tract–related complication. It has been demonstrated as useful for revealing the symptoms in acute cholangitis and biliary obstruction in studies with a limited number of cases, so that elective surgery can be performed later. The ERCP procedure itself may also evacuate content of the obstructed common bile duct when combined with sphincterotomy, thereby avoiding common bile duct exploration during surgery; in addition, postoperative biliary fistula formation can be prevented by drainage of the cyst cavity.32–35 Controversially, it has been suggested that nonoperative perendoscopic treatment may be insufficient in treating cholangitis and in an emergency context, because the cystic cavity containing biliopurulent material is situated above the biliary convergence and cannot always be reached via a perendoscopic nasobiliary drain.22
In a recent study, preoperative ERCP was performed in 16 cases and was effective in 10 patients, thus avoiding common bile duct exploration during operation. For the remaining 6 patients, choledochotomy with T-tube drainage was required in 4 patients. Preoperative assessment with ERCP was not required in patients undergoing laparoscopic surgery and percutaneous treatment. We conclude that our results also support the usefulness of preoperative ERCP + sphincterotomy in the management of biliocystic communication in patients with acute cholangitis and biliary obstruction.
Intraoperative management of cystobiliary communication is an important matter, although the communications between the cyst and the biliary tree usually involve small cholangioles and direct extension into major bile ducts is rare.22,36,37 The primary goals of the surgery must be evacuation of the cyst content, cavity management, clearance of any choledochal obstruction, and the restoration of the normal bile drainage. Suturing visible openings of fistula, internal transfistulary drainage, directed fistulization and transcholedochal evacuation without approaching the cyst cavity from the liver surface are commonly recommended techniques for intraoperative management of cystobiliary communications.22,38–41
In their series with large cystobiliary fistulas, Zaouche et al.,22 performed 180 common bile duct (CBD) explorations in 244 cases and proposed that the presence (or not) of hydatid material in the CBD did not seem to be a determinant for the choice of surgical procedure; nor did it influence the specific complications and hospital stay rates. These investigators therefore concluded that the systematic drainage of a free CBD was not necessary. They also concluded that internal transfistulary drainage and an unroofing procedure involving suturing of healthy fistula tissue to an omentoplasty, or suture obliteration capitonnage of the remaining cavity were feasible and effective methods, but that direct fistulization was associated with greater morbidity and a longer hospital stay. If the fistula was left untouched, then drainage of the remaining cavity with or without CBD drainage was also accompanied by a high mortality and morbidity rates.
In our experience, cholecystectomy and intraoperative cholangiography were performed in six of 185 patients treated with open surgery, and CBD exploration with T-tube drainage was preferred in 4 patients for restoration of normal bile drainage. Intraoperative suture placement at the openings of the fistulas was accomplished in 36 patients. We did not have any experience with regard to other cavity management options, such as internal transfistulary drainage, directed fistulization, or transcholedochal evacuation.
Among the most commonly reported postoperative complications are persistent external biliary fistulas (defined as persisting after the tenth day and excessive drainage of clear bile over hundreds of millimeters per day); remaining cavity infections (accompanied by fever and a biliopurulent discharge from the drain); purulent retention in the remaining cavity associated with ineffective drainage or early removal of a drain, necessitating evacuation by percutaneous puncture or by reoperation; residual obstacles to the CBD; and bile peritonitis and other morbidities related to surgery, with reported rates of 6% to 47%.3,21,22,25,27–31,42,43 Persistent external biliary fistulas was were the most prominent postoperative complication in our experience, resulting in 15% (28/185), 6% (2/30), and 7% (10/140) among patients treated with open, laparoscopic, and percutaneous treatment, respectively. The overall rate for biliary fistulas was 11% (40/355) in this study, which can be considered reasonable compared to reported rates. Because most of these fistulas resulted from simple drainage with open surgery, we consider revising our cavity management in favor of omentoplasty, capitonnage, and untested options such as internal transfistulary drainage.
Conservative therapy with replacement of daily electrolyte and fluid losses was reported to be effective in low-output fistulas (<300 ml bile/day), but endoscopic treatment has been advocated in high-output fistulas of more than 1 week’s duration with no signs of reduction and in low-output fistulas of more than 3 weeks’ duration without signs of reduction.32,43 Combined ERCP + sphincterotomy/nasobiliary catheter was successful in the treatment of 18 of 40 fistulas in our series. Prolonged tube drainage resulted in spontaneous closure of the fistula in 18 patients with low output rates, but 4 patients required surgical intervention after percutaneous treatment.
In the management of remaining cavity infections and purulent retention in the remaining cavity, we observed that percutaneous drainage and treatment with antibiotics should be the first modality attempted, reserving the surgical option for unsuccessful conservative medical management.
Recurrence after primary treatment of hepatic hydatid disease is an important issue, with reported rates ranging from 1.1% to 25%.3,18,22,25,28–31,42–44 Recurrent disease is usually defined as reappearance of live cysts at the site of a previously treated cyst or presentation with new extrahepatic disease. Presentation with major complications including pyogenic infection and intrabiliary rupture has also been accepted as recurrence. Because recurrence may develop many years later, longer follow-up is generally recommended if possible.16 Ultrasound and CT scanning, in addition to clinical and serological evaluation, are preferred methods for identifying recurrent disease. The radiographic appearance of postoperative cysts may vary significantly and is frequently time-dependent, but growth of the cyst appears to be the best imaging marker for significant locally recurrent disease.45,46 In the case of recurrence, because the primary treatment has failed, more radical treatment may be indicated as a therapeutic option. In patients with appropriate cyst morphology (univesicular and peripheral cysts), PAIR and catheterization might be considered a therapeutic option, especially if the surgical alternative is associated with increased risk.
As a safe procedure, cyst evacuation with or without partial cystectomy can be done with low operative mortality if required cyst wall resection does not involve major pedicles. Because recurrence is likely after parasite penetration through the pericyst; the likelihood of further recurrence is considered high unless complete cystopericystectomy or liver resection is carried out; this procedure also offers the best chance of curing recurrent hepatic hydatid disease if it can be carried out without opening the cyst.16
In a recent study, recurrent disease was diagnosed in 30 patients (16.2%) in the open surgery group, 1 patient (3.3%) in the laparoscopy group, and 5 patients (3.5%) in the group treated with the percutaneous approach. In 10 patients with univesicular recurrent cysts, PAIR and catheterization was preferred as a therapeutic option, and the results were satisfactory. The remaining 20 patients underwent reoperation, with omentoplasty in 6 patients, capitonnage in 10 patients, and cystopericystectomy in 4 patients as preferred treatment of recurrences. The single recurrence after laparoscopic surgery was due to a missed multivesicular cyst that was treated with open surgery 3 months after primary intervention. Partial cystectomy and evacuation with open surgery was the preferred treatment for recurrences after percutaneous approaches. Recurrence rates were significantly higher after the partial cystectomy + drainage procedure than with other open surgical procedures.
In conclusion, selection of the treatment option that provides the best results with the lowest recurrence rates and minimal morbidity and mortality is the mainstay in the management of hepatic hydatid disease. The condition of the patient, characteristics of the cyst, the presence of cystobiliary communications, and the availability of a multidisciplinary team are the factors we believe directly affect the outcome. Radical interventions such as total cystectomy and hepatic resection can be done safely with minimal morbidity and mortality for suitable cases. Conventional procedures are associated with more morbidity because they are used most often for complicated and difficult case. Laparoscopic surgery seems to be effective and safe with low morbidity and recurrence rates for type I–III cysts in accessible locations, but the procedure has its own disadvantages such as limited area of surgical manipulation and difficulty with controlling the spillage during puncture.
Our experience with PAIR and catheterization provides evidence that the procedure is an effective and safe tool and a good alternative to surgery for properly selected cases.
References
Ammann RW, Eckert J. Cestodes. Echinococcus. Gastroenterol. Clin North Am 1996;25:655–689
Anonymous. Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull WHO 1996;74:231–242
Yorganci K, Sayek I. Surgical treatment of hydatid cysts of the liver in the era of percutaneous treatment. Am J Surg 2002;184:63–69
Alonso CO, Moreno GE, Loinaz SC, et al. Results of 22 years of experience in radical surgical teatment of hepatic hydatid cysts. Hepatogastroenterology 2001;48:235–243
Ertem M, Uras C, Karahasanoglu T, et al. Laparoscopic approach to hepatic hydatid disease. Dig Surg 1998;15:333–336
Lujan Mompean JA, Parrilla PP, Robles CR, et al. Laparoscopic treatment of a liver hydatid cyst. Br J Surg 1993;80:907–908
Saglam A. Laparoscopic treatment of liver hydatid cysts. Surg Laparosc Endosc 1996;6:16–21
Alper A, Emre A, Acarli K, et al. Laparoscopic treatment of hepatic hydatid disease. J Laparoendosc Surg 1996;6:29–33
Khuroo MS, Wani NA, Javid G, et al. Percutaneous drainage compared with surgery for hepatic hydatid cysts. N Engl J Med 1997;337:881–887
Odev K, Paksoy Y, Arslan A, et al. Sonographically guided percutaneous treatment of hepatic hydatid cysts: long-term results. J Clin Ultrasound 2000;28:469–478
Ustunsoz B, Akhan O, Kamiloglu MA, et al. Percutaneous treatment of hydatid cysts of the liver: long-term results. AJR Am J Roentgenol 1999;172:91–96
Kayaalp C, Sengul N, Akoglu M. Importance of cyst content in hydatid liver surgery. Arch Surg 2002;137:159–163
Gharbi HA, Hassine W, Brauner MW, et al. Ultrasound examination of the hydatic liver. Radiology 1981;139:459–463
Lewall DB, McCorkell SJ. Hepatic echinococcal cysts: sonographic appearance and classification. Radiology 1985;155:773–775
Akhan O, Ozmen MN. Percutaneous treatment of liver hydatid cysts. Eur J Radiol 1999;32:76–85
Sielaff TD, Taylor B, Langer B. Recurrence of hydatid disease. World J Surg 2001;25:83–86
Sayek I, Onat D. Diagnosis and treatment of uncomplicated hydatid cyst of the liver. World J Surg 2001;25:21–27
Cirenei A, Bertoldi I. Evolution of surgery for liver hydatidosis from 1950 to today: analysis of a personal experience. World J Surg 2001;25:87–92
Ben Amor N, Gargouri M, Gharbi HA, et al. [Trial therapy of inoperable abdominal hydatid cysts by puncture]. Ann Parasitol Hum Comp 1986;61:689–692
Akhan O, Dincer A, Gokoz A, et al. Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol. An experimental study in sheep. Invest Radiol 1993;28:121–127
Dziri C, Haouet K, Fingerhut A. Treatment of hydatid cyst of the liver: where is the evidence? World J Surg 2004;28:731–736
Zaouche A, Haouet K, Jouini M, et al. Management of liver hydatid cysts with a large biliocystic fistula: multicenter retrospective study. Tunisian Surgical Association. World J Surg 2001;25:28–39
Tan A, Yakut M, Kaymakcioglu N, et al. The results of surgical treatment and percutaneous drainage of hepatic hydatid disease. Int Surg 1998;83:314–316
Kaymakcioglu N, Yakut M, Tan A, et al. Recurrence after surgery at the liver cyst hydatid. Turkish J Surg 1998;14:339–345
Balik AA, Basoglu M, Celebi F, et al. Surgical treatment of hydatid disease of the liver: review of 304 cases. Arch Surg 1999;134:166–169
Karavias DD, Vagianos CE, Bouboulis N, et al. Improved techniques in the surgical treatment of hepatic hydatidosis. Surg Gynecol Obstet 1992;174:176–180
Sayek I, Yalin R, Sanac Y. Surgical treatment of hydatid disease of the liver. Arch Surg 1980;115:847–850
Vagianos CE, Karavias DD, Kakkos SK, et al. Conservative surgery in the treatment of hepatic hydatidosis. Eur J Surg 1995;161:415–420
Alfieri S, Doglietto GB, Pacelli F, et al. Radical surgery for liver hydatid disease: a study of 89 consecutive patients. Hepatogastroenterology 1997;44:496–500
Dziri C, Paquet JC, Hay JM, et al. Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver: a multicenter, prospective, randomized trial. French Association for Surgical Research. J Am Coll Surg 1999;188:281–289
Magistrelli P, Masetti R, Coppola R, et al. Surgical treatment of hydatid disease of the liver. A 20-year experience. Arch Surg 1991;126:518–522
Tekant Y, Bilge O, Acarli K, et al. Endoscopic sphincterotomy in the treatment of postoperative biliary fistulas of hepatic hydatid disease. Surg Endosc 1996;10:909–911
Rodriguez AN, Sanchez del Rio AL, Alguacil LV, et al. Effectiveness of endoscopic sphincterotomy in complicated hepatic hydatid disease. Gastrointest Endosc 1998;48:593–597
Dumas R, Le Gall P, Hastier P, et al. The role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatid disease. Endoscopy 1999;31:242–247
Ozaslan E, Bayraktar Y. Endoscopic therapy in the management of hepatobiliary hydatid disease. J Clin Gastroenterol 2002;35:160–174
Marti-Bonmati L, Menor F, Ballesta A. Hydatid cyst of the liver: rupture into the biliary tree. AJR Am J Roentgenol 1988;150:1051–1053
Pedrosa I, Saiz A, Arrazola J, et al. Hydatid disease: radiologic and pathologic features and complications. Radiographics 2000;20:795–817
Lygidakis NJ. Diagnosis and treatment of intrabiliary rupture of hydatid cyst of the liver. Arch Surg 1983;118:1186–1189
Kornaros SE, Aboul-Nour TA. Frank intrabiliary rupture of hydatid hepatic cyst: diagnosis and treatment. J Am Coll Surg 1996;183:466–470
Ulualp KM, Aydemir I, Senturk H, et al. Management of intrabiliary rupture of hydatid cyst of the liver. World J Surg 1995;19:720–724
Bedirli A, Sakrak O, Sozuer EM, et al. Surgical management of spontaneous intrabiliary rupture of hydatid liver cysts. Surg Today 2002;32:594–597
Karavias DD, Tsamandas AC, Payatakes AH, et al. Simple (non-parasitic) liver cysts: clinical presentation and outcome. Hepatogastroenterology 2000;47:1439–1443
Skroubis G, Vagianos C, Polydorou A, et al. Significance of bile leaks complicating conservative surgery for liver hydatidosis. World J Surg 2002;26:704–708
Erdem E, Nessar M, Sungurtekin U, et al. The management of hepatic hydatid cysts: review of 94 cases. J Hepatobiliary Pancreat Surg 1998;5:179–183
El Tahir MI, Omojola MF, Malatani T, et al. Hydatid disease of the liver: evaluation of ultrasound and computed tomography. Br J Radiol 1992;65:390–392
Marino JM, Bueno J, Prieto C, et al. Residual cavities after surgery for hepatic hydatid cysts—an ultrasonographic evaluation. Eur J Pediatr Surg 1995;5:274–276
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yagci, G., Ustunsoz, B., Kaymakcioglu, N. et al. Results of Surgical, Laparoscopic, and Percutaneous Treatment for Hydatid Disease of the Liver: 10 Years Experience with 355 Patients. World J. Surg. 29, 1670–1679 (2005). https://doi.org/10.1007/s00268-005-0058-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0058-1