Abstract
Measurement is the essence of science. The BIS™ brain monitor provides direct propofol response measurement. Measuring transformed the propofol ketamine technique from a qualitative approach to a quantitatively reproducible one. Propofol was originally titrated with an IV bag and a micro-drip IV set. Propofol response was titrated to clinical signs. An infusion pump later replaced the IV bag, enabling the propofol dose enumeration. The propofol effect was measured with a BIS.™ A statistically significant 30% propofol reduction was achieved with BIS™ monitoring. Patient movement occurred during propofol sedation. Secondary EMG trending to BIS™ enabled the differentiation of cortically based movement (i.e., deeper sedation indicated) from spinal cord-based movement (i.e., more local indicated). Outcomes were improved when surgeons re-injected vasoconstricted field with patient movement.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ambulatory cosmetic surgery patients are expected to be discharged to home following their surgery. The problems facing their anesthesiologists and surgeons are (1) delayed emergence, (2) pain, and (3) postoperative nausea and vomiting (PONV). These problems are causes for unintended hospital admission after day surgery. Ambulatory discharge is predicated on discharge-ready emergence in about an hour after surgery. When patients take longer to emerge, discharge is delayed, resulting in increased nursing hours and decreased cost-effectiveness. Discharge delays secondary to patients’ rides are a different issue but not in the purview of the anesthesiologist.
A patient’s brain cannot respond to information it does not receive. Failure to saturate N-methyl-d-aspartate (NMDA) receptors prior to local anesthetic (LA) injection is a major cause of postoperative pain [1]. From March 26, 1992, to December 26, 1998, after a qualitative, incremental propofol induction, a 50 mg IV ketamine dose was given 2–5′ before the surgeon’s LA. The 2–5′ delay allows the ketamine to saturate the NMDA receptors. The saturation provides 10–20′ immobility for LA injections. After the initial LA injections, patient movement during the case was challenging. The ‘too light’ versus ‘more local’ discussion resulted in more IV drugs, instead of more local, being given to the patient. Discharge delays resulted.
Glycopyrrolate 0.2 mg IV was given prior to induction to eliminate laryngospasm potential by minimizing oropharyngeal secretions. The propofol initial drip rate was set to approximate the patient’s baseline heart rate and then adjusted based on response. Patient variation in propofol sensitivity made it difficult to enumerate the effective dose that was administered. Variable propofol drip rates with the technique made it artful but challenging to reproduce.
Propofol sedation was defined by the clinical signs of loss of lid reflex and loss of verbal response. Propofol sedation blocks ketamine hallucinations [2]. The degree of airway intervention was dictated by patient response. The incremental propofol induction preserved the muscles responsible for maintaining a patent airway, i.e., genioglossus, orbicularis oris, temporalis masseter. Spontaneous ventilation was preserved by avoiding an initial propofol bolus. Approximately 30% of the patients required only the rhytidectomy position to keep a patent airway. With the chin extended and head rotated laterally, two vectors of temporalis masseter were exerted on the genioglossus kept the tongue off the back of the throat. In another 30% of patients, the rhytidectomy position proved inadequate. To open the airway, an IV bag was placed under the patients’ shoulders. The IV bag added additional force to the genioglossus muscle. If neither of the first two airway maneuvers were adequate to keep the airway open, a nasal airway was used for another 30% of patients. Less than 10% of patients required laryngeal mask airway (LMA) to support their airway. No patients required bag and mask ventilation or endotracheal intubation. More than half the patients required no airway instrumentation, an advantage for avoiding postoperative sore throat complaints.
Typical induction times were between 2 and 3.’ Propofol was deliberately titrated to produce an SpO2 92–95% with spontaneous ventilation on room air. The oxygen concentration in room air is insufficient to support combustion during facial electrocautery [3]. Respiratory depression to this SpO2 level was thought to prevent ketamine hallucinations. None were reported. Oxygen was available but rarely needed. Continuous EKG and NIABP were also monitored. Suction, Ambu® bags, crash carts and defibrillators were available. Only suction for persistent oropharyngeal secretions was used.
Without anti-emetics, the opioid-free, propofol-then-ketamine-then-LA paradigm achieved the lowest published PONV rate (0.6%) in an Apfel-defined high-risk patient population (i.e., non-smoking, female, PONV/motion sickness history, emetogenic cosmetic surgery) [4]. A 50 mg ketamine dose produced immobility (i.e., dissociative effect) for approximately 10–20′ in patients between 35 and 145 kg. Opioid postoperative rescue was also absent.
A brain is not required to produce movement. A headless chicken still moves. Non-purposeful movement was generated in the spinal cord, not the brain. Prior to BIS™ brain monitoring, all propofol sedation movement was treated as if patient awareness was a possible cause. Surgeons regard any non-purposeful patient movement during sedation as ‘too light.’ Based on the surgeons’ belief that vasoconstriction equals adequate analgesia, the request for ‘deeper’ anesthesia was made when patients moved. When ‘deeper’ anesthesia was requested, this author responded with ‘more local.’ Prior to BIS™ monitoring, the author was unable to persuade the surgeons; the non-purposeful movement was generated from the spinal cord, not the brain. The author was unable to convince the surgeons to re-inject vasoconstricted fields in the immediate area of dissection. Adding additional drugs (i.e., more propofol or ketamine) failed to accurately address the issue of inadequate analgesia. Prolonged emergence and discharge followed.
“If you cannot measure it, you cannot improve it.” Lord Kelvin’s temperature quote also provides the rationale for direct brain measurement of propofol response. Measuring prevents too much or too little propofol. On December 26, 1998, bispectral (BIS™) index monitoring was added to the technique along with real-time electromyogram (EMG) secondary trending (Fig. 1). Induction began with a baseline rate of 25 mcg kg−1 min−1 propofol with successive 50 mcg kg−1 propofol boluses (i.e., shorturl.at/bsFP9 s). Induction times remained between 2 and 3 min. Propofol hypnosis was defined by BIS < 75 with baseline EMG. After induction, a 50 mg IV ketamine dose was administered followed by a 2–5′ wait, and then, subcutaneous LA was injected by the surgeon.
The BIS™ values are delayed from real time by 15–30 s. Relying on BIS™ numbers alone for propofol titration is akin to driving an automobile with rearview mirror information alone. BIS™ values alone are not useful to predict changing patient requirements during surgery. The EMG is the electrical activity of the facial frontalis muscle and is as real time as the EKG. Trended EMG spikes persist even when patients have forehead Botox.® EMG spikes signal incipient arousal of the brain [5]. More propofol is indicated to maintain sedation. Arousal precedes pain (nociception) [6]. Pre-LA injection saturation of NMDA receptors is the basis of opioid-free, preemptive analgesia [1]. In addition to patient immobility, the absence of EMG spikes with LA injection provides a reproducible basis with which to diagnose NMDA receptor saturation and opioid-free preemptive analgesia. See Fig. 1.
Numb patients rarely move during surgery. Non-purposeful patient movement under sedation has been a vexing problem for both the surgeon and the anesthesiologist. Is the movement purposeful or brain-originating with possible awareness. More sedation would be indicated? Or is the movement non-purposeful, meaning spinal cord-originating without possible awareness? More LA is indicated. Lidocaine–epinephrine is injected. Surgeons believe the epinephrine produced vasoconstriction equals adequate analgesia. Therefore, they believe patient movement means ‘too light,’ awareness risk and ‘deeper’ sedation indicated.
BIS™ < 75 with baseline EMG provides objective evidence the patient is asleep and will not remember the surgery. Patient movement with propofol @ BIS < 75 without EMG spike equals spinal cord movement and is without awareness risk. Re-injection in the immediate area of surgical dissection eliminates non-purposeful patient movement in 98–99% of cases [1]. The use of objective evidence of the origin of patient movement was an effective; dispassionate means of helping surgeons understand vasoconstriction may not equal adequate analgesia. Improved emergence and discharge followed.
During surgery, propofol was maintained 60 < BIS < 75 with baseline EMG at 25–50 mcg. kg−1. min−1 with a range between 2 and 200 mcg. kg−1. min,−1 a 100-fold variation to achieve the same numerical level of sedation. The use of body weight, vital signs variation, body mass index (BMI), target-controlled infusion (TCI) or pharmacokinetic/pharmacodynamic (PK/PD) as the basis for propofol dosing is unlikely to account for this 100-fold variation. The effect of directly measuring with real-time EMG/BIS™ brain monitoring yielded a statistically significant 30% reduction in propofol [7]. Delayed emergence secondary to excess propofol or ketamine was eliminated [1].
Eighty percent of patients required one or two 50 mg ketamine doses to satisfactorily complete the cases, many of which were 5 h. Aggregate ketamine doses exceeding 200 mg were not incompatible with one-hour discharge times. The brain size of a 100 kg male is not twice that of a 50 kg female, yet both remain immobile for LA injection with the same 50 mg ketamine dose. The heaviest patient to remain immobile from the 50 mg ketamine dose was this 145 kg liposuction patient. See Fig. 2. Therefore, the number of NMDA receptors does not vary with body weight.
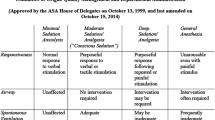
LA was administered in volumes not to exceed 5000 ccs of tumescent solution or less than 55 mg kg−1 [8]. Postoperative bupivacaine was sprayed, not injected, on the surgical field not to exceed 50 ccs of 0.25%. Cases included liposuction, sub-pectoral breast augmentation, body implants, reduction mammoplasty, abdominoplasty and all facial cosmetic cases, i.e., rhytidectomy, browlift, facial implants and laser facial resurfacing. N.B., Small volumes of 2% lidocaine with epinephrine were used for rhinoplasty and blepharoplasty cases (Table 1).
Conclusion
Over 26 years, more than 5000 patients received propofol then 50 mg ketamine then LA for ambulatory cosmetic surgery. All were discharged to home without requiring professional aftercare givers. No patients were admitted to the hospital for either pain, PONV or prolonged emergence. There were no opioid addicts or opioid overdose deaths. The transition from qualitative to quantitative propofol ketamine sedation allowed the paradigm to evolve from an art to a science-based technique. Real-time EMG/BIS™ monitoring helped surgeons understand vasoconstriction may not guarantee adequate analgesia.
References
Friedberg BL (2017) Can Friedberg’s triad solve persistent anesthesia problems? Over-medication, pain management, postoperative nausea and vomiting. Plast Reconstr Surg Glob Open 5(10):1527. https://doi.org/10.1097/GOX.0000000000001527
Friedberg BL (1993) Hypnotic doses of propofol block ketamine induced hallucinations. Plast Reconstr Surg 91:196–197. https://doi.org/10.1097/00006534-199301000-00047
Friedberg BL (1999) Facial laser resurfacing with propofol-ketamine technique: room air, spontaneous ventilation (RASV) anesthesia. Dermatol Surg 25:569–572. https://doi.org/10.1046/j.1524-4725.1999.99077
Friedberg BL (1999) Propofol-ketamine technique, dissociative anesthesia for office surgery: a five-year review of 1,264 cases. Aesth Plast Surg 23:70–74. https://doi.org/10.1007/s002669900245
Practice Advisory for Intraoperative Awareness and Brain Function Monitoring (2006) Anesthesiol 104:847–864
Lichtner G, Auksztulewicz R, Velten H et al (2018) Nociceptive activation in the spinal cord & brain persists during deep general anesthesia. Br J Anaesth 121:291–302. https://doi.org/10.1016/j.bja.2018.03.031
Friedberg BL, Sigl JC (2000) Clonidine premedication decreases propofol consumption during bispectral (BIS) index monitored propofol-ketamine technique for office-based surgery. Dermatol Surg 26:848–852. https://doi.org/10.1046/j.1524-4725.2000.00074.x
Ostad A, Kageyama N, Moy RL (1996) Tumescent anesthesia with a lidocaine dose of 55 mg/kg is safe for liposuction. Dermatol Surg 22:921–927. https://doi.org/10.1213/ANE.0000000000001119
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflicts of interest to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
informed consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Friedberg, B.L. BIS Monitoring Transformed Opioid-Free Propofol Ketamine Anesthesia From Art to Science for Ambulatory Cosmetic Surgery. Aesth Plast Surg 44, 2308–2311 (2020). https://doi.org/10.1007/s00266-020-01987-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-020-01987-6