Abstract
Background
In ophthalmic artery occlusion by hyaluronic acid injection, the globe may get worse by direct intravitreal administration of hyaluronidase. Retrograde cannulation of the ophthalmic artery may have the potential for restoration of retinal perfusion and minimizing the risk of phthisis bulbi. The study investigated the feasibility of cannulation of the ophthalmic artery for retrograde injection.
Methods
In 10 right orbits of 10 cadavers, cannulation and ink injection of the supraorbital artery in the supraorbital approach were performed under surgical loupe magnification. In 10 left orbits, the medial upper lid was curvedly incised to retrieve the retroseptal ophthalmic artery for cannulation by a transorbital approach. Procedural times were recorded. Diameters of related arteries were bilaterally measured for comparison. Dissections to verify dye distribution were performed.
Results
Cannulation was successfully performed in 100 % and 90 % of the transorbital and the supraorbital approaches, respectively. The transorbital approach was more practical to perform compared with the supraorbital approach due to a trend toward a short procedure time (18.4 ± 3.8 vs. 21.9 ± 5.0 min, p = 0.74). The postseptal ophthalmic artery exhibited a tortious course, easily retrieved and cannulated, with a larger diameter compared to the supraorbital artery (1.25 ± 0.23 vs. 0.84 ± 0.16 mm, p = 0.000).
Conclusions
The transorbital approach is more practical than the supraorbital approach for retrograde cannulation of the ophthalmic artery. This study provides a reliable access route implication for hyaluronidase injection into the ophthalmic artery to salvage central retinal occlusion following hyaluronic acid injection.
No Level Assigned
This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern Basic Science, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors http://www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central retinal artery occlusion is strongly associated with poor visual and ocular outcomes [1–3]. Complete obstruction of the central retinal artery results in permanent visual impairment. Several studies have indicated that thrombolysis and fibrinolysis aimed at early restoration of blood flow have the potential to improve clinical outcomes in central retinal artery occlusion caused by thrombosis [4]. The risk of vitreous hemorrhage is a major problem associated with intraarterial administration. Moreover, catheter placement within the artery during anterograde selective intraarterial thrombolysis may inadvertently cause ocular symptoms. The ideal approach is delivery of the drug at a low dose [4]. This leads to the concept of retrograde injection of the drug into the ophthalmic artery. This method of drug administration, using a catheter placed percutaneously in one of the terminal cutaneous branches of the ophthalmic artery, is a safer and interesting alternative.
Percutaneous hyaluronidase injection has a beneficial effect in cutaneous arterial occlusion caused by cosmetic facial injection with hyaluronic acid. In this case, it is administrated instantly at the initial phase of complications. This suggests that hyaluronidase injection should have a beneficial effect in retinal vessel occlusion caused by hyaluronic acid injection as well. However, a practical route of administration is important. Percutaneous injection directly into the orbit or the globe performed by an inexperienced physician may be harmful to the globe and the structures within the cranial cavity. Retrograde cannulation of the ophthalmic arteries or one of its branches may have the potential to achieve visual improvement and minimize the risk of ocular injury when it is performed by a well-trained esthetic physician. This method may be a reliable access route implication for hyaluronidase injection into the ophthalmic artery to salvage central retinal occlusion following cosmetic hyaluronic acid injection. Retrograde intraarterial hyaluronidase injection may have its full beneficial effect in retinal artery occlusion when it is administrated correctly during the critical time period. Cannulation of the ophthalmic arteries may allow the enzyme to degrade most hyaluronic acid and minimize the risk of ocular injury. Size, position, and variation of the ophthalmic artery as well as a sizable terminal branch, such as the supraorbital artery, may imply the effectiveness and success of the treatment. This study was conducted to investigate the feasibility of cannulation targeting specifically at the ophthalmic artery. It included investigation of sizes and locations of both the supraorbital artery and the terminal part of the ophthalmic artery, and the development of a safe and reliable technique to facilitate the preparation and cannulation of these vessels. This study aimed to provide a reliable access route implication for hyaluronidase injection into the ophthalmic artery to salvage central retinal occlusion following hyaluronic acid injection.
Materials and Methods
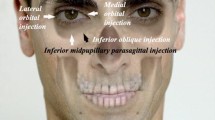
Body donors were obtained in accordance with the Declaration of Helsinki. This cadaver experiment study was performed on 20 orbits of 10 soft embalmed human cadaveric specimens. In 10 right orbits, the supraorbital region was dissected unilaterally with a linear incision just inferior to the medial end of the brow to identify the supraorbital and/or the supratrochlear arteries (Fig. 1). This was followed by cannulation of the supraorbital or the supratrochlear arteries using a 27-gage needle and the injection of dye to demonstrate vascular territories and anastomoses under operating loupe magnification. The 27-gage needle was chosen to minimize arterial wall damage and dye leakage. In 10 left orbits, a curved incision along the medial orbital margin at the medial side of the upper lid was performed to retrieve the retroseptal part of the ophthalmic artery, emerging from the orbital septum, with a sling suture for cannulation. Dye was injected to demonstrate vascular territories and anastomoses. Dissections to verify dye distribution in the orbits were performed (Fig. 2). Suture ligation might be performed to control dye leakage. The procedural times of both methods were recorded in minutes for comparison. Nonparametric statistics were used as appropriate.
Two approaches at the left eye for cannulation and retrograde injection of hyaluronidase into the retinal arterial system. The supraorbital incision just below the medial eyebrow (white ellipse) for cannulation of the supraorbital and the supratrochlear arteries. The transorbital incision (black ellipse) for cannulation of the terminal (retroseptal) ophthalmic artery. In this case the dorsal nasal artery arises as a common trunk with the supratrochlear artery from the terminal segment of the ophthalmic artery. Latex injection enhances the ophthalmic artery for illustration
In each specimen, the exit points of the supratrochlear and the supraorbital arteries were located. Diameters of the relevant arteries were bilaterally measured for comparison using a paired-samples t test. The distances between the supraorbital arteries and the midline at the level of the eyebrow and location of the terminal portion of the ophthalmic artery above the medial canthal tendon were measured with a caliper. Dissection of each orbit allowed the distribution of the injected dye to be investigated. In each right eye, after cannulation of the supraorbital artery, the ophthalmic artery was traced and located through the orbital septum. After the removal of the lens and the vitreous tissue using a pericorneal incision to collapse the globe, dissection was continued to the orbital apex allowing the orbital fat and the extraocular muscles to be inspected for dye staining.
Results
Cannulation was successfully performed in 100 and 90 % of the transorbital and the supraorbital approaches, respectively. The transorbital approach was more practical to perform compared with the supraorbital approach with a trend toward a shorter procedure time (18.4 ± 3.8 vs. 21.9 ± 5.0 min, p = 0.74). The terminal segment of the ophthalmic artery, before emerging from the orbital septum (postseptal ophthalmic artery), exhibited a tortious course (Fig. 3) easily retrieved from the orbit for cannulation with a larger diameter than the supraorbital artery (1.25 ± 0.23 vs. 0.84 ± 0.16 mm, p = 0.000).
The tortuous retroseptal segment of the ophthalmic artery can be stretched beyond the orbital septum for secured cannulation and controllable injection. Latex injection enhances the ophthalmic artery for illustration. A black hole in the middle of the lower photograph is an opening in the orbital fat from which the terminal segment of the ophthalmic artery emerges
Anatomical Findings
In the orbit, the ophthalmic artery coursed toward the superior part of the medial orbital wall. Before leaving the orbit, the artery gave rise to the supraorbital artery in 8 of 20 hemifaces (40 %) and the medial palpebral artery in 20 hemifaces (100 %) (Table 1). The supraorbital artery branched off in the middle of the orbit, passed anteriorly along the medial border of the superior rectus, and left the orbit through the supraorbital notch or foramen in 5 hemifaces, and medial to the notch in 3 hemifaces to supply the frontalis muscles from the underside. The ophthalmic artery terminated behind the orbital septum 13.1 ± 0.4 mm above the medial canthal tendon just beneath the trochlea. After emerging from the orbital septum, the ophthalmic artery gave rise to the extraorbital origin of the supraorbital artery in 12 hemifaces and then terminated into two branches in all 20 hemifaces, the supratrochlear artery and the dorsal nasal artery. In these cases, the ophthalmic artery terminated by continuation as the supratrochlear artery in 12 and the dorsal nasal artery in 8 hemifaces (Fig. 4), the smaller one arose from the artery as a branch. The supraorbital artery, which has an extraorbital origin, traveled obliquely from the epicanthal region to the supraorbital notch where it accompanied the supraorbital nerve to the forehead.
The Supraorbital Approach: Cannulation of the Supraorbital Artery
The supraorbital artery was detected running through the frowning muscles in all cadaver specimens examined. It had a superficial branch between the depressor supercilli and the corrugator supercilli muscles. The deep branch ran across the bony superciliary arch to the periosteal side of the frontal galea aponeurotica. It was distinct from the supratrochlear artery which took a subcutaneous course on the surface of the depressor supercilli and the procerus muscle. In only 5 of 20 hemifaces, the supraorbital arteries emerged from the supraorbital notch. In 3 hemifaces, the supraorbital artery emerged from the orbit medial to the notch and nerve, and its size was approximately equal to the supratrochlear artery. In 12 hemifaces, the artery branched from the extraorbital terminal part of the ophthalmic artery as a single branch before the supratrochlear artery branched off and traveled to the notch from the medial eye corner to accompany the supraorbital nerve. Both arteries, the supratrochlear and the supraorbital arteries, usually communicated and formed a subcutaneous arterial plexus rather than orientated as individual branches.
At the supraorbital region just below the brow, the supratrochlear artery was located at the medial eyebrow and medial to the vertical line drawn from the eye corner. Typically, it exhibited a more superficial course than the supraorbital artery. It bifurcated into terminal branches on the surface of the depressor supercilli. The average exit point of the supratrochlear artery was at 13.3 ± 2.4 mm (range 9–16) temporal to the midline. The average distance between the midline and the point where the supratrochlear artery crosses the supraorbital rim was 11.3 ± 1.9 mm (range 9–19). The outer diameter of the supratrochlear artery at the supraorbital rim was found to be 0.74 ± 0.17 mm (range 0.5–1.4). The supraorbital artery was located just above the supraorbital rim at an average of 24.6 ± 4.8 mm (range 21–35) temporal to the midline. Typically, we observed multiple smaller terminal branches of the supraorbital artery that made anastomoses with the superficial temporal artery over the medial two-third of brow. These anastomoses demonstrated the strong association between the vascular territories of the internal and external carotid arteries in the area of the supraorbital rim. The course of the supraorbital artery deviated more laterally than that of the supratrochlear artery which usually deviated medially. The distance between the midline and the supraorbital artery was 24.4 ± 2.6 mm (range 21–31) at the supercilliary arch. The outer diameter of the supraorbital artery (0.84 ± 0.16 mm; range 0.6–1.1) was slightly larger than the outer diameter of the supratrochlear artery. Of 20 specimens, five supraorbital arteries exhibited smaller diameters than the supratrochlear artery. Because of the sizable artery and its superficial course, in this case, the supratrochlear artery is an alternative option for cannulation using the supraorbital approach.
In all specimens, anastomoses of the terminal branch of the ophthalmic artery, the dorsal nasal artery, with the angular artery were below the brow along the side of the radix and the nasal bone medial to anastomoses between the supraorbital artery and the superficial temporal artery.
Cannulation of the supraorbital artery was achieved in 9 out of 10 right orbits (90 %). A small supraorbital artery could not be cannulated successfully because of the failure to access the arterial lumen leading to wall tearing, dye leakage and no dye-stained orbital contents.
The Transorbital Approach: Cannulation of the Terminal Part of the Ophthalmic Artery
The supratrochlear and the dorsal nasal arteries were the first two branches usually encountered in the subcutaneous tissue when the curve upper lid incision was made along the medial orbital rim in the transorbital approach. The former ran from the epicanthal area obliquely upward across the medial orbital rim toward the glabella, the later ran across the depressor supercilli obliquely downward toward the radix. The first two branches either ran in the same direction (12 in 20 hemifaces, 60 %) (Fig. 1) or on the opposite direction (8 in 20 hemifaces, 40 %) (Fig. 4). Tracing these branches backward through the orbital septum, the terminal part of the ophthalmic artery could be identified with the medial palpebral branch running to the medial canthus under the preseptal muscle of the orbicularis oculi. The ophthalmic artery was small and tortious at the 10-mm terminal segment and then gradually enlarged within the orbit. Because of the tortuosity, the terminal segment could be retracted from the orbit by a loop of the sling suture for at least 5 mm. This made it easier to perform a secure cannulation. Three locations of the terminal part of the ophthalmic artery in the globe before it existed at the epicanthal point based on the frequency of distributions were as follows: 12 arteries (60 %) were medial to the levator aponeurosis close to the superior orbital wall; 6 arteries (30 %) were just lateral to trochlea close to the superior nasal corner of the orbit; and 2 arteries (10 %) were along the medial orbital wall just above the medial canthal tendon.
Cannulation of the ophthalmic artery was successful in all 10 left orbits. The diameter at the cannulation site was 1.25 ± 0.23 mm (range 0.9–1.7). In all cadaveric specimens examined after removal of the globe contents, the typical point of entry of the ophthalmic artery into the optic canal was found laterally, underneath the optic nerve. Upon examination of all cadaveric specimens after dissection to the orbital apex, a spread of dye into the ophthalmic and the central retinal artery was evidenced by dye staining the orbital contents including the vitreous gel, the orbital fat, and the extraocular muscles (Fig. 2).
Discussion
The skin incision of the supraorbital approach is concealed by the medial eyebrow. So does that of the transorbital approach, which is also a standard incision in blepharoplasty and concealed by the natural eyelid contour. Both the supratrochlear artery and the supraorbital artery originate from or, in the minority, have direct anastomoses with the ophthalmic artery. The later type arises from the angular artery as its terminal branches. None of these arteries communicate with intracranial blood vessels [5–8]. A cadaver investigation provided evidence supporting the consideration of retrograde injection into the ophthalmic artery and that percutaneous cannulation of the supraorbital artery is feasible to deliver thrombolytic agents to the retinal vascular system [4]. This method could also be applied to the hyaluronidase injection into the ophthalmic artery. In this initial study, we are in agreement with the previous study that the supraorbital approach using the supraorbital or the supratrochlear arteries is feasible for ophthalmic artery cannulation. Because of the smaller caliber of the cannulated arteries within the Asian population, we used smaller needles compared to the previous study. Concerning the smaller arteries, we conducted another transorbital approach as an alternative with a lower incision and approximately equal incision length. We suggest that, for a rapid and reliable retrograde injection into the ophthalmic arterial system, direct access into the terminal part of the ophthalmic artery behind the orbital septum is recommended and preferable to perform over the cannulation of the supraorbital artery. Less anatomic variability of the postseptal ophthalmic artery with a sizable diameter compared with the supraorbital artery provided easier cannulation and a reliable access route. Besides, the vertical course of the ophthalmic artery along the orbital axis facilitates cannulation and provides a comfortable injection angle. Moreover, the relationships to the medial orbital wall and the medial canthal tendon of the terminal ophthalmic artery were remarkably consistent and the tortuosity allowed retrieval of the arterial segment from the opening of the orbital septum for open operating space. Wider operating space makes secured cannulation and well-controlled retrograde injections possible. Retrograde injection directly at the ophthalmic artery allows rapid access of the hyaluronidase to the central retinal artery at the origin of the ophthalmic artery. The supraorbital artery typically exhibits small terminal branches that made multiple anastomoses with the descending branches of the superficial temporal artery. These anastomoses may steal some amount of the injection material leading to ineffective clearance of the occluded retinal artery. The previous study revealed an average distance of 16.4 mm between the midline and the point where the supratrochlear artery crosses the supraorbital rim [4]. However, in our study, the exit points of the supratrochlear artery were much closer to the midline.
Another interesting finding from our study was the observation that injected dye within the supraorbital or the terminal ophthalmic artery resulted in a spread into the ophthalmic branches, including the central retinal artery. Previous study on the cannulation of the supraorbital artery attempted to provide firm experimental evidence for the successful delivery of drugs to the retinal vascular system, but we also provide evidence to support the results by inspection of the orbital fat and the extraocular muscles for dye staining. The clinical observation revealed that rapidly changing intravascular pressure may result in reversal of blood flow direction within the supraorbital arteries toward the ophthalmic artery. Given a sufficient pressure of injection, it seems plausible that these vessels have the potential to provide a reliable route for the retrograde hyarulonidase injection in the clinical setting. Based on the findings that supraorbital artery mean peak systolic and end-diastolic blood flow velocities were markedly different, it may be hypothesized that ultrasonographic controlled retrograde injections would be possible. Based on the anatomical distributions and anastomoses of the ophthalmic artery and the supraorbital artery, the intraarterial administration of drugs via the terminal part of the ophthalmic artery would require relatively small injection volumes compared with administration via the supraorbital artery. There is a reasonable likelihood that, in a pathological situation such as retinal artery occlusion, blood flow within the retinal vascular system or the ophthalmic artery is significantly decreased, thereby affecting injection pressures or the dosage of drugs required for the targeted delivery of hyaluronidase via the supraorbital artery. Experiments to determine the change of blood flow in patients with retinal vessel occlusion are beyond the scope of the present study. However, a greater understanding of the detailed anatomy of the orbital arterial system will be an important component for future efforts to establish cannulation of the ophthalmic artery via the supraorbital or transorbital approach as an alternative to systemic administration in retinal artery occlusion. However, cadaver injection studies do not provide us with physiological information. Further studies are necessary to prove the effectiveness of this therapeutic option.
To the best of our knowledge direct injection of hyaluronidase into the ophthalmic artery to treat blindness following cosmetic facial injection of hyaluronic acid has not been performed. Three important issues have to be verified for patient safety and effectiveness of the treatment. The first is how to perform the injection of hyaluronidase into the ophthalmic artery, the second is how retrograde arterial injection of the hyaluronidase affects the orbital tissues including the vitreous body, and the last is how to prevent large amounts of hyaluronidase from entering the internal carotid artery after it reaches the origin of the central retinal artery. This is because the ophthalmic artery is the first branch of the internal carotid artery distal to the cavernous sinus, and the central retinal artery is the first branch of the ophthalmic artery.
This study initially explored the first issue in a cadaver model, by expressing a rapid and reliable procedure. Experimentation in the cadaver model is a limitation of this study. Two substantial factors which are difficult to control may influence the results of the retrograde injections during the in vivo study. Cyclical changes in intraluminal arterial pressure limit the injection time during the systolic phase and allow the injection materials to escape to the carotid system in the diastolic phase. Various degrees of constriction responding to wall injury may block the materials from passing further in the ophthalmic artery.
The second and the last issues determining the effectiveness and safety of the treatment are beyond the scope of this study, but some complications could be speculated. Complications of intraarterial administration of hyaluronidase into the orbit may be vitreous detachment and seizures. Hyaluronic acid is covalently linked to form a proteoglycan macromolecule of the vitreous gel. Hyaluronidase dissolutes glycosidic bonds of hyaluronic acid resulting in decreased viscosity of the vitreous body. In healthy eyes, vitreous tissue is adhered to the retina; administration of hyaluronidase has the potential to induce a posterior vitreous detachment. In diseased eyes, it has been investigated for treatment of vitreous hemorrhage in diabetic retinopathy [9, 10].
Hyaluronic acid is a major constituent of the extracellular matrix of the adult brain. A recent animal study suggested that decreasing the hyaluronic acid in the extracellular substance in the brain tissue reduces the size of the brain’s extracellular space; some areas may be prone to epileptic seizures [11]. The seizures were most prevalent in mice which showed the greatest hyaluronic acid reduction in the hippocampus. Electrophysiology in mice brain slices demonstrated spontaneous epileptiform activity in pyramidal neurons, while histological analysis revealed an increase in cell packing in the stratum pyramidale. Further studies have to investigate the two important issues mentioned above which are possible to execute initially in cadaver models. Ultrasound and other imaging modalities may allow monitoring and controlling the injections to minimize the hyaluronidase entering the brain tissue via the carotid system.
Conclusion
Cannulation with retrograde injection of dye was successfully performed in 100 % and 90 % of the transorbital and the supraorbital approaches, respectively, evidenced by staining of the vitreous gel and orbital contents. The transorbital approach was more practical to perform compared with the supraorbital approach with a trend toward a short procedure time (18.4 ± 3.8 vs. 21.9 ± 5.0 min, p = 0.74). The postseptal terminal segment of the ophthalmic artery exhibited a tortious course easily retrieved by a sling suture with a larger diameter than the supraorbital artery (1.25 ± 0.23 vs. 0.84 ± 0.16 mm, p = 0.000).
References
Chen Y, Wang W, Li J, Yu Y, Li L, Lu N (2014) Fundus artery occlusion caused by cosmetic facial injections. Chin Med J 127:1434–1437
Kim KE, Ahn SJ, Woo SJ, Kim N, Hwang JM (2013) Central retinal artery occlusion caused by fat embolism following endoscopic sinus surgery. J Neuroophthalmol 33:149–150
Lazzeri S, Figus M, Nardi M, Lazzeri D, Agostini T, Zhang YX (2013) Iatrogenic retinal artery occlusion caused by cosmetic facial filler injections. Am J Ophthalmol 155:407–408
Schwenn OK, Wustenberg EG, Konerding MA, Hattenbach LO (2005) Experimental percutaneous cannulation of the supraorbital arteries: implication for future therapy. Invest Ophthalmol Vis Sci 46:1557–1560
Kilinc H, Bilen BT (2007) Supraorbital artery island flap for periorbital defects. J Craniofac Surg 18:1114–1119
Erdogmus S, Govsa F (2007) Anatomy of the supraorbital region and the evaluation of it for the reconstruction of facial defects. J Craniofac Surg 18:104–112
Lopez R, Lauwers F, Paoli JR, Boutault F, Guitard J (2008) The vascular system of the upper eyelid. Anatomical study and clinical interest. Surg Radiol Anat 30:265–269
Kleintjes WG (2007) Forehead anatomy: arterial variations and venous link of the midline forehead flap. J Plast Reconstr Aesthet Surg 60:593–606
Lopez-Lopez F, Rodriguez-Blanco M, Gomez-Ulla F, Marticorena J (2009) Enzymatic vitreolysis. Curr Diabetes Rev 5:57–62
Narayanan R, Kuppermann BD (2009) Hyaluronidase for pharmacologic vitreolysis. Dev Ophthalmol 44:20–25
Arranz AM, Perkins KL, Irie F, Lewis DP, Hrabe J, Xiao F, Itano N, Kimata K, Hrabetova S, Yamaguchi Y (2014) Hyaluronan deficiency due to Has3 knock-out causes altered neuronal activity and seizures via reduction in brain extracellular space. J Neurosci 34:6164–6176
Acknowledgments
Miss Hannah E Greenwood from the University of Liverpool kindly revised this manuscript.
Conflict of interest
All authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tansatit, T., Apinuntrum, P. & Phetudom, T. An Anatomic Basis for Treatment of Retinal Artery Occlusions Caused by Hyaluronic Acid Injections: A Cadaveric Study. Aesth Plast Surg 38, 1131–1137 (2014). https://doi.org/10.1007/s00266-014-0408-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-014-0408-1