Abstract
Background
Phthisis bulbi may follow cosmetic filler injections. Early attempts to inject hyaluronidase into the orbit after detection of devastating signs and symptoms may potentially mitigate the complications.
Methods
Cannula routes along the orbital walls were studied. Depths of injections were determined in 30 dry skulls. Deep cannula insertions were carefully performed while avoiding exiting the orbit. Forty-six cadaveric orbits with intravascular latex injection were dissected to determine injection techniques, to verify structures at risk along the routes, and to evaluate substance dispersion.
Results
The limited depths of the superior, lateral, medial, and inferior injection routes were 4.2, 3.8, 3.6, and 2.5 cm respectively, while the orbital width was 3.9 cm. The superior parasagittal injection was effective and rarely tears the superior ophthalmic vein, artery, and the optic nerve. The medial injection should be avoided because it may injure the lacrimal sac, the ophthalmic artery, and the optic nerve. Without limited depth, the lateral injection may damage the lacrimal gland and artery and proceeds to damage the optic nerve. The inferior parasagittal injection tends to exit into the infratemporal fossa but the inferior oblique injection may be safer and effective but more complicate with the depth of 4.2 cm.
Conclusion
The superior parasagittal injection is a recommended simple technique with a minimal chance of vascular injury. The inferior oblique injection requires more skill but it may be safer because of the lower position. For safety reasons, depth of each cannula insertion should not exceed the orbital width.
No Level Assigned
This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern BasicScience, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors http://www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Various injection techniques for fillers are available for restoration of the aging process [1, 2]. These can be utilized for facial augmentations and lifting to modernize the appearance and for correction of facial defects and contour asymmetry. Hyaluronic acid is the appropriate material because of its degradability using hyaluronidase [3]. Even if the material can be degraded, a few serious complications still occur [4–8]. Ocular complications occur from accidental injections into the branches of the facial or the superficial temporal arteries. Moreover inadvertent cannulation of the distal branches of the ophthalmic artery is the worst scenario because the material travels directly to the eye via the retrograde route [9–11]. Unbearable pain in the eye during the injection followed by sudden loss of vision and ophthalmoplegia is signs of ophthalmic artery occlusion [12, 13]. Early treatment by the esthetic physician at the clinic before referral to the salvage team of specialists may mitigate the tragedy. The initial treatments, which are usually ineffective, are mainly aimed to promote vasodilatation. Direct injection of hyaluronidase to the orbit may add another chance for recovery.
Retrobulbar injection has previously been associated with retrobulbar hemorrhage and globe perforation [14, 15]. This technique requires a curved trajectory estimated by the injector without bony guidance to enter into the muscle cone. This explains the increasing popularity of the sub-Tenon injection technique as an alternative. Sub-Tenon injection is effective and fast in achieving infiltration of the extraocular muscles and the ciliary nerves with the use of a confined space [16]. The curved needle follows the globe surface in the sub-bulbar fascial space toward the optic nerve. Because the procedure is technically demanding and a curved needle is required, the use of a sub-Tenon route requires specific training to correctly perform the technique without globe perforation [16]. All techniques mentioned previously emphasize the nerves for ocular anesthesia and akinesia, but a simple technique of hyaluronidase injection similar to peribulbar injection with emphasis on vascular structures is required for esthetic physicians instead [17, 18]. A facial plastic surgeon in our salvage team has used direct orbit injections in a patient with full ocular and cutaneous symptoms of ophthalmic artery occlusion. The result was so impressive except for blindness which was not reversible. In this case, total ophthalmoplegia and all the threatening skin and globe infractions completely resolved with multiple passes of a needle at the inferior temporal corner of the orbit. These initial direct injections should be standardized for obtaining an optimum result.
An understanding of the orbital wall architecture is essential. Knowledge of the courses of nerves is important for anesthetic injections but for hyaluronidase injection awareness of the orbital blood vessels should be emphasized instead to place to the drug around the vessels and to avoid retrobulbar hemorrhage [15, 16]. This study provides the simple techniques to inject hyaluronidase to the orbit for esthetic or emergency physicians. These techniques are different from the previous anesthetic injection techniques and emphasize cannula gliding along the orbital walls to minimize blind estimation of the cannula routes.
Materials and Methods
Determination of the Possible Cannula Route of Each Injection Technique
Orbital dissections were performed in 20 orbits of 10 soft embalmed cadavers to determine safe and simple techniques for cannula insertions into the orbit. By collapsing the globe dissections progressed layer by layer both from the superior and the anterior views to identify all the relationships of the orbital contents and the neurovascular distributions. Dissection emphasizes the courses of the superior ophthalmic vein and the ophthalmic artery to identify hazardous cannula routes. The thickness of the orbital fat around the globe and the muscle cone were observed. Criteria for the suitable technique were cannula insertion should.
-
1.
Be simple to perform and be a lifelong skill.
-
2.
Not be needed to fully recognize the anatomical basis of the orbital contents and walls.
-
3.
Be safe with a minimal chance to endanger the essential orbital contents: the optic nerve, the ophthalmic artery, the superior ophthalmic vein and the extraocular muscles.
-
4.
Retain the injection within the orbit, not exit into the cranial cavity.
-
5.
Cease safely at the orbital wall.
-
6.
Be placed near the orbital apex to facilitate dispersion toward the ciliary arteries in the retrobulbar space.
Verification of Efficacy of the Injection Technique
The efficacy of the techniques was determined in 20 orbits in 10 soft embalmed cadavers in the supine position. Green dye was injected into the globe via a corneal puncture to monitor cannula injury to the globe. Intraocular pressure was estimated by palpation as in clinical practices. Red and blue latexes were injected into the common carotid artery and the internal jugular vein, respectively, for revealing evidence of vascular injuries. Fragments or interrupted columns of latex near each cannula retained within the orbit were evidence of vascular injury. Another criterion of potential vascular injury was witness of a vascular structure that lied very close or even touched the cannula without an interposing muscle. The safe cannula route was that in which no vascular structure lied close to or came into contact with the cannula or had an interposing structure such as a muscle between them. To simulate the clinical scenario, a long blunt 25G 50-mm cannula was inserted at each of four orbital margins, and the cannula was glided along the corresponding orbital wall (Fig. 1). The superior parasagittal midpupillary injection was at the middle of the superior orbital margin. The medial injection was just above the medial canthal tendon. The inferior parasagittal injection was at the middle of the inferior orbital margin. The inferior oblique injection was on the vertical line just lateral to the lacrimal caruncle. The lateral injection was at the area just inferior to the lateral canthal ligament. The superior and the inferior parasagittal injections were performed by keeping the cannula routes along the sagittal plane. If the cannula touched the lateral wall or obviously deviated from the sagittal plane more than 10° when it glided along the slope of the lateral orbital wall, cannula insertion must stop, otherwise it leads to the muscle cone and the optic nerve. The medial and the lateral injections were performed by keeping the cannula routes along the transverse plane. Only in the inferior oblique injection, the cannula route intentionally was deviated 10° laterally from the sagittal plane by gliding along the orbital floor. A compass application in a mobile phone could provide accurate guidance. Observations for injuries to the orbital contents were performed from the superior view in five cadavers and from the inferior view in the other five. The calvarium and the orbital roofs were removed using a vibrating saw and a chisel in five cadavers for superior inspections. The inferior orbital rims were removed together with the orbital floors and parts of the maxillar and the malar bones bilaterally in the other five cadavers to evaluate in the same manner from below.
For substance dispersion, six orbits in three cadavers were injected with 3 ml of red liquid dye using the superior parasagittal midpupillary technique with a 25G cannula, one fast injection, and five slow injections through a skin hole made by a 27G needle to limit dye reflux. Then the orbital contents were removed through a circular periorbital incision for dissections to evaluate the effectiveness of the injections in two cadavers. Two orbits of the last cadaver were dissected 24 h later.
Results
Forty-six cadaveric orbits, from 23 cadavers aged ranging between 35 and 62 years with intravascular latex injection, were separately dissected to determine injection techniques, to verify structures at risk along the routes and to evaluate substance dispersion. The bony configuration of each orbital wall including the positions of the orbital fissures is the most important factor influencing the route of the injection techniques (Figs. 2, 3). The course of the superior ophthalmic vein and the ophthalmic artery at the superior nasal corner of the orbit and the exit of the optic nerve at the optic foramen define the risk of complications (Figs. 4, 5, 6, 7, 8).
The Superior Parasagittal Midpupillary Injection
The superior ophthalmic vein, the frontal nerve, and the ophthalmic artery usually travel longitudinally spanning from the middle of the orbital roof to the medial corner (Figs. 4, 5). While the frontal nerve is fixed to the roof by the supraorbital foramen or notch, fortunately, the superior ophthalmic vein the largest vein in the orbit is covered and protected completely along its course from the cannula route in all 20 orbits by the levator palpebrae superioris and its fatty tissue envelope (Figs. 6, 7). A blunt 25G cannula is suitable for this superior parasagittal injection. After insertion through the skin and the orbital septum via a hole made by a 23G needle, the 25G cannula should follow the orbital roof until it reaches and stops at the greater wing of the sphenoid at the posterior part of the lateral wall (Fig. 2a). Care should be taken to keep the cannula trajectory on the sagittal plane otherwise it will deviate medially, penetrate the muscle cone and tear the superior ophthalmic vein and then the optic nerve at the optic canal (Fig. 2b). Midpupillary cannula insertion along the sagittal plane traveled between the frontal nerve at the roof and the levator palpebrae superioris muscle and ended near the orbital apex lateral to the common ring tendon (Fig. 8). The risk of injury to the optic nerve will increase when the injection point is close to the medial wall. The maximum depth allowed in the cannula insertion was 4.2 ± 0.3 cm (Table 1). This is the suitable technique recommended among all in this study.
The Lateral Orbital Injection Below the Lateral Canthus
Although cannula insertion along the lateral wall is safe from injury of the important neurovascular structures such as the ophthalmic artery and veins (Fig. 2c), the lacrimal gland at the superior temporal corner is susceptible to damage at its lower part. The steep slope of the lateral wall cannot accommodate the cannula inserted along the sagittal plane. Inclined insertion along the lateral orbital wall toward the midline led to the ophthalmic artery, the superior ophthalmic vein, and the optic nerve at the orbital apex in all 20 orbits (Fig. 2d). These included direct injuries to eight optic nerves and two superior ophthalmic veins, respectively. The maximum depth allowed in the cannula insertion was 3.8 ± 0.4 cm. In this injection technique, a 30-mm hypodermic needle can be safely used.
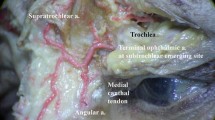
The Medial Orbital Injection Above the Medial Canthus
The lamina papyracea is a convex bone plate of the ethmoid. A tortious route of the ophthalmic artery courses along the upper half and ends at the superior nasal corner under the trochlea of the superior oblique muscle (Figs. 4, 5). The ethmoid branches anchor the ophthalmic artery and the superior ophthalmic vein to the superior nasal corner making this corner “the danger zone.” The lacrimal sac, attached and enveloped by the muscle fibers, bulges and occupies the lower half of the medial wall in the lacrimal fossa behind the medial canthal tendon. Based on the sagittal alignment of the medial orbital wall, the cannula inserted anywhere along the medial wall led to the optic canal or the superior orbital fissure at the orbital apex in all 20 orbits (Fig. 3a, b). Moreover the endangered ophthalmic artery lied very close to the cannula in 6 of 20 orbits. The maximum depth allowed in the cannula insertion was 3.6 ± 0.4 cm. A sharp needle is prohibited in this area.
Two Inferior Orbital Injections
The midpupillary line crossing the inferior orbital margin was a site for cannula insertion along the sagittal plane. This cannula route went between the inferior surface of the globe and the inferior orbital margin until it touched the sphenoid greater wing at the lateral orbital wall at a depth of 3.2 ± 0.3 cm. The orbital floor leads to the inferior orbital fissure on the lateral half because the orbital surface of the zygoma is depressed below the lateral orbital wall. The cannula should not glide along the orbital floor otherwise it could exit the orbit through the inferior orbital fissure to the infratemporal fossa. This was observed in 6 out of 20 orbits when the cannula followed the orbital floor. Although it was not a serious complication, injection outside the orbit had certainly lost the hyaluronidase with no added benefits. The maximum depth allowed in the cannula insertion was 2.5 ± 0.3 cm before it reached the inferior orbital fissure (Fig. 3d). If the cannula followed the orbital fat layer above the floor and managed to cross the inferior orbital fissure without exit the orbit, it touched the sphenoid greater wing. Because of the steep slope of the lateral wall related to the sagittal plane, the flexible cannula will deviate at the lateral wall and go toward the muscle cone. No globe perforation was evidenced in this study.
Another injection that requires more skill is the inferior oblique injection, in which the cannula enters medially on the anterior lacrimal crest at the lower orbital margin between the two vertical lines of the lacrimal caruncle and the medial limbus. The medial half of the floor on the orbital surface of the maxilla is raised higher than the inferior orbital fissure. The injection route that intentionally deviated 10° from the sagittal plane to the temple engaged the apex of the lateral wall in all orbits at 4.2 ± 0.3 cm (Fig. 3c). Most of the techniques mentioned previously require limited depth for cessation before reaching the optic nerve or exiting the orbit, but the superior parasagittal and this inferior oblique injection are the two freehand techniques that do not require the limited depth. The injection depths are limited by the lateral orbital wall without endangering the optic nerve.
Natural Barriers for Hyaluronidase Spread
The orbital fat is loosely arranged into a lobulated mass, lobules are incompletely separated from each other by the natural barriers. They are the globe, the lacrimal gland, the extraocular muscles, and the recesses in the eyelids. Continuations between the retrobulbar fat in the muscle cone and the adjacent periconal fat around the muscle cone exist at the gaps between the muscles which are wider than the muscles. The orbital fat is loose and can be easily removed. No definite boundaries define the fat compartments in the orbit, and no separating fascial barriers were recognized except for the suspensory and the check ligaments which envelope the anterior part of the globe around the attachments of the extraocular muscles. The periconal fat completely envelopes the muscle cone and separates it from the orbital walls. Red dye spread along the orbital walls and dispersed into the retrobulbar fat from the injection site near the apex (Fig. 9). Rapid injection limited dye spreading only along the injection tract without entering the retrobulbar space. Injections performed as slow as possible effectively infused dye into the retrobulbar fat. The optic nerve, the ophthalmic artery, and the ciliary arteries were stained with red dye in all five orbits with slow injection. Only the anterior part of the inferior orbital fat is spared from staining. The last cadaver with delayed exploration expressed homogeneous deeper stained color within the muscle cone. Dispersion of hyaluronidase from the periconal fat to the ciliary arteries in the retrobulbar fat is possible and the process of dispersion continues as time passes. Although hyaluronidase injected into the orbit may spread toward less resistance, in a confined space such as the orbit the drug certainly flows into all directions including the retrobulbar fat and further redistribution occurs until it is neutralized with native hyaluronic acid within the orbital tissues.
Discussion
A common application of hyaluronidase is used in combination with local anesthetics in elective ophthalmic surgery to accelerate drug dispersion [19]. In the occluded vascular complications following filler injections, hyaluronidase has to come into direct contact with the hyaluronic acid molecules within the occluded lumen of the branch retinal vessels. By catalyzing the hydrolysis of hyaluronic acid, hyaluronidase lowers the viscosity, thereby reestablishing tissue perfusion. An optimal result of hyaluronidase injection should be obtained by direct cannulation and retrograde injection via the supraorbital, the supratrochlear, or the dorsal nasal arteries at the medial eye corner. This operative procedure requires a facial plastic surgeon to make an incision at the epicanthal region. Considering the hyaluronidase injection, we concluded that direct cannulation and retrograde injection of the occluded vessel by an experienced surgeon is the treatment of choice. The second choice is sub-Tenon or retrobulbar injections by an experienced ophthalmologist or an anesthesiologist. These techniques endanger the globe and the optic nerve. Vitreous hemorrhage, globe, and optic nerve perforation may complicate the clinical signs and symptoms. When a specialist in salvage procedures is not available, direct injection of the hyaluronidase into the orbit using a safe technique may be the only choice to reestablish capillary perfusion and may partially restore the retinal blood supply. The aim of the injection is to perfuse the hyaluronidase into the safe area until it reaches the retrobulbar fat which contains the ciliary vessels. Experience from various clinical trials shows that hyaluronidase seems to have no toxicity toward normal tissues and to have no other adverse effects in preclinical experiments and when used in various clinical trials [19].
In the sub-Tenon injection technique, physicians access the subfascial space by a cut hole at the inferonasal segment near the corneoscleral junction using a fine scissors and pass the curve cannula following the globe surface to reach the posterior pole. The periconal space is wider and easier to access than the sub-Tenon space. It allows dispersion of the hyaluronidase into the retrobulbar space containing the ciliary arteries. The 25G cannula is available in the clinic because it is commonly used for filler injections. A simple technique to indirectly access the retrobulbar space is more practical for esthetic physicians who do not routinely perform operative procedures.
The orbital apex lies medial to the sagittal plane passing through the midpupillary line. This plane passes through the sphenoid greater wing at the lateral orbital wall. A cannula inserted along the sagittal plane at the midpupillary line will go directly to the slope of the sphenoid greater wing and then deviate medially to the orbital apex and the optic nerve. During the superior parasagittal injections, the first hit is the cannula touching the sphenoid bone at 4.2 ± 0.3 mm and then, if the cannula is further advanced, the second hit is the muscle cone. This study proposes injection techniques in which the hyaluronidase is safely injected very close to the ophthalmic vascular system. Concerning individual variation, if the physician feels the loss of resistance after a pop felt with the deep cannula position, reinsertion of the cannula with carefully evaluation of the landmark is recommended otherwise intracranial injection may be encountered.
When decreased visual acuity or sudden loss of vision occurs during or after a cosmetic facial injection of hyaluronic acid, a hyaluronidase injection into the orbit instantly is recommended. Two levels of aggressive treatment should be considered based on the severity of the ocular complications, experience and knowledge of the esthetic physician who faces the ocular complication. The superior parasagittal injection of hyaluronidase within the cannula depth of 40 mm is the least aggressive treatment. This injection technique is effective, easy, and safe enough for the esthetic physician. For fully confident esthetic physicians who recognize and cope with the sudden loss of sight together with other ocular ischemic symptoms of the patient such as ophthalmoplegia and intractable pain in the eye and the glabella-forehead region, more aggressive treatment should be administration otherwise phthisis bulbi may be the result. These include aggressive injections with all injection techniques recommended and repeat the injections within 20 min based on the clinical results. Although this suggestion is based on a rare personal experience, it is founded on all available information. Multiple injections will allow complete dispersion of hyaluronidase throughout the orbit. Minute orbital vessels which are capillaries and venules within the ischemic extraocular muscles and the orbital fat are the targets for intravascular absorption of hyaluronidase. These vessels allow for the possibility of direct contact of the hyaluronidase and the hyaluronic acid. Then the patient is referred to the salvage team for further aggressive treatments such as arterial cannulation.
Although the injection techniques are safe, practicing in cadavers under the supervision of experienced trainers until essential knowledge and skill of the techniques are gained is important before the techniques are used clinically. In the office setting, most procedures are performed freehand without radiologic and ultrasound guidance. Participation in a hands-on workshop is an ethical way of medical practice for novices nowadays.
Cadaver study has many limitations due to the lack of muscle movements and tone, no vascular perfusion and also decreased intraocular pressure. Although hyaluronidase is effective in dispersion, the effectiveness of direct injection of hyaluronidase into the periconal fat for salvage of branch retinal artery occlusion is still questionable. This requires animal experiments to quantify the results [20]. The neutral position of the cornea and dense sclera facilitate simulation of injections. Although it is possible to simulate vascular injury causing retrobulbar hemorrhage in soft embalmed cadavers with latex perfusion in the carotid artery and the internal jugular vein, assessment of efficacy and complications between two compared injection techniques certainly requires many more specimens which may not be cost-effective and not practical. However, one of these injection techniques may be utilized for ocular anesthesia, a randomized control clinical trial comparing the recommended injection techniques and the standard retrobulbar injection for anesthetized ocular surgery performed by experienced ophthalmologists or anesthesiologists sounds reasonable and ethical.
Conclusion
Superior parasagittal midpupillary injection and inferior oblique injection may be safe and effective techniques for esthetic physicians because of the deep cannula positions when ocular complications occur. The superior parasagittal injection is a simple technique recommended with minimal chance of vascular injury. The inferior oblique injection requires more skill but it may be safer. For safety reasons, the depth of each cannula insertion should not exceed the orbital width.
References
Shetty R (2014) Under eye infraorbital injection technique: the best value in facial rejuvenation. J Cosmet Dermatol 13:79–84
Lee SK, Kim HS (2014) Recent trend in the choice of fillers and injection techniques in Asia: a questionnaire study based on expert opinion. J Drugs Dermatol 13:24–31
Narayanan R, Kuppermann BD (2009) Hyaluronidase for pharmacologic vitreolysis. Dev Ophthalmol 44:20–25
He MS, Sheu MM, Huang ZL, Tsai CH, Tsai RK (2013) Sudden bilateral vision loss and brain infarction following cosmetic hyaluronic acid injection. JAMA Ophthalmol 131:1234–1235
Kim EG, Eom TK, Kang SJ (2014) Severe visual loss and cerebral infarction after injection of hyaluronic acid gel. J Craniofac Surg 25:684–686
Kim YJ, Kim SS, Song WK, Lee SY, Yoon JS (2011) Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthal Plast Reconstr Surg 27:e152–e155
Lazzeri S, Figus M, Nardi M, Lazzeri D, Agostini T, Zhang YX (2013) Iatrogenic retinal artery occlusion caused by cosmetic facial filler injections. Am J Ophthalmol 155:407–408
Park KH, Kim YK, Woo SJ, Kang SW, Lee WK, Choi KS, Kwak HW, Yoon IH, Huh K, Kim JW (2014) Iatrogenic occlusion of the ophthalmic artery after cosmetic facial filler injections: a national survey by the korean retina society. JAMA Ophthalmol 132:714–723
Erdogmus S, Govsa F (2007) Anatomy of the supraorbital region and the evaluation of it for the reconstruction of facial defects. J Craniofac Surg 18:104–112
Kilinc H, Bilen BT (2007) Supraorbital artery island flap for periorbital defects. J Craniofac Surg 18:1114–1119
Schwenn OK, Wustenberg EG, Konerding MA, Hattenbach LO (2005) Experimental percutaneous cannulation of the supraorbital arteries: implication for future therapy. Investig Ophthalmol Vis Sci 46:1557–1560
Kim SN, Byun DS, Park JH, Han SW, Baik JS, Kim JY, Park JH (2014) Panophthalmoplegia and vision loss after cosmetic nasal dorsum injection. J Clin Neurosci 21:678–680
Lazzeri D, Agostini T, Figus M, Nardi M, Pantaloni M, Lazzeri S (2012) Blindness following cosmetic injections of the face. Plast Reconstr Surg 129:995–1012
Adekoya BJ, Onakoya AO, Balogun BG, Oworu O (2013) Current practice of ophthalmic anesthesia in Nigeria. Middle East Afr J Ophthalmol 20:341–344
Gross A, Cestari DM (2014) Optic neuropathy following retrobulbar injection: a review. Semin Ophthalmol 29:434–439
Kumar CM, Eid H, Dodds C (2011) Sub-Tenon’s anaesthesia: complications and their prevention. Eye 25:694–703
Lessa S, Passarelli CA (2007) Peribulbar anesthesia for blepharoplasty. Aesthetic Plast Surg 31:463–466 discussion 467
ElKhamary SM, Riad W (2014) Three dimensional MRI study: safety of short versus long needle peribulbar anesthesia. Saudi J Ophthalmol 28:220–224
Hamada S, Devys JM, Xuan TH, Ganem S, Sahel JA, Heran F, Plaud B (2005) Role of hyaluronidase in diplopia after peribulbar anesthesia for cataract surgery. Ophthalmology 112:879–882
Batlle OR, Sponse WE, Swann FB, Margo CE, Groth SL, Ayyala RS (2014) Retrobulbar diversion of aqueous humor: laboratory studies. J Glaucoma. doi:10.1097/IJG.0000000000000077
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tansatit, T., Apinuntrum, P. & Phetudom, T. A Cadaveric Feasibility Study of the Intraorbital Cannula Injections of Hyaluronidase for Initial Salvation of the Ophthalmic Artery Occlusion. Aesth Plast Surg 39, 252–261 (2015). https://doi.org/10.1007/s00266-015-0456-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-015-0456-1