Abstract
Background
Addressing the long upper lip has been a complex problem for some time. Methods such as the subnasal skin excision and the vermillion advancement technique have been described, but both leave a visible scar. A no-scar lip-lift technique is necessary for a subset of patients who have a long upper lip and will not accept a visible scar.
Methods
The upper lip is shortened via an intranasal incision and suspension suture that elevates the upper lip and anchors it to the anterior nasal spine. A retrospective review of 92 patients who had undergone upper lip-lift with the no-scar suspension technique was performed. Three plastic surgeons assessed the pre- and postoperative results and determined the presence of improvement in four categories: lip shortening, lip projection, incisor show, and vermillion show.
Results
The lip parameters improved, with 85% of the patients showing noticeable lip shortening, 79% showing increased sagittal projection, 74% exhibiting increased incisor show, and 25% exhibiting increased vermillion show. All the patients had improvement in at least one of the four categories. Complications were experienced by two patients with a suture abscess and one patient with an unraveled suture.
Conclusion
The overall lip contours improved after the lip suspension technique, most noticeably in terms of lip height and sagittal projection, and the scar was hidden intranasally.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The lips are the central feature in the lower third of facial aesthetics and play an important role in expression, communication, and seduction. This fact is clearly depicted in the media, with many actresses and models specifically known for their lips. This in turn has pushed the public demand for improved lip aesthetics, which has helped to drive the soft tissue filler market in recent years, creating a multimillion-dollar industry. Fillers allow patients to increase the fullness of their lips with minimal downtime, yet increasing the lip’s volume is only one portion of the puzzle. The often overlooked sequela of adding an excessive amount of volume to the upper lip is a long ptotic appearance from the tissue expansion effect, which can be difficult to correct. Multiple other causes exist for a long upper lip, for which people seek improvement.
The previous methods for addressing a long upper lip were based on direct surgical excision of the nasal base skin [1–3] or a vermillion advancement [4–6]. However, the problem with these techniques is the visible scar. Whereas the subnasal skin excision technique is preferred for an older, thin-skinned patient, this technique usually is not tolerated by a young, healthy cosmetic patient [7].
Through the use of an intranasal incision, we have been able to lift and shorten the upper lip with a suspension suture secured to the anterior nasal spine, leaving no signs of a visible scar. The scars are hidden intranasally, which should be more amenable to a young patient. The goal of this technique is to prevent a visible scar while shortening and improving the contour of the upper lip. We have applied this technique successfully to a variety of patients with a long, ptotic upper lip, and we present our results.
Materials and Methods
Surgical Technique
Local anesthetic (1% lidocaine with 1:100,000 epinephrine) is injected into the upper lip, nasal mucosa, and nasal skin. The mucosa between the caudal septum and the lower lateral cartilages is marked (Fig. 1). A transfixion incision is made through the nasal septum, separating the lower lateral cartilages from the septal cartilage. This incision then is carried inferiorly onto the bilateral nasal floors and superiorly as an intercartilaginous incision, separating lateral crura of the lower lateral cartilages from the upper lateral cartilages (Fig. 2). Through the inferior aspect of the incision, tenotomy scissors then are used to identify the anterior nasal spine and dissect in the subcutaneous plane just above the orbicularis oris muscle in the upper lip (Fig. 3). The area of dissection is limited to the width of the nasal base and only half the distance to the white roll of the lip.
a The mucoperichondrium is incised between the lower lateral cartilage and the caudal septum. b The same incision is repeated on the contralateral side, creating a complete transfixion incision. Bilaterally, this incision continues superiorly as an intracartilaginous incision between the upper lateral cartilages and the lateral crura
a The nasal mucoperichondrium is elevated from the nasal septum to identify the caudal septum and the anterior nasal spine (black arrow). b Through the intranasal incision, the upper lip skin is elevated from the orbicularis oris muscle. This dissection is limited to the upper half of the upper lip, indicated by the dashed black line
A limited dissection of the nasal tip and dorsum is approached through the intercartilaginous portion of the same incision. The columella and lower lateral cartilages should now move independently as a subunit. At this point, it is important to assess the external nasal valve, particularly the cartilaginous footplates of the medial crura. If there appears to be flaring of the footplates, they should be excised to prevent airway obstruction with the advancement of the columellar subunit (Fig. 4).
a After elevation of the upper lip skin and subcutaneous tissue from the orbicularis oris, the columellar subunit is freely mobile, and the footplates (black arrows) of the medial crura are evaluated. b The footplates are excised to prevent external nasal valve obstruction once the columellar subunit is advanced
A 3-0 supramid suture (S. Jackson, Inc., Alexandria, VA, USA) loaded on a large-diameter French eye needle is passed through the orbicularis oris muscle at a level approximately one-half the distance from the columella-labial junction to the white roll of the upper lip. This allows the surgeon to elevate the lip adequately without tethering or inhibiting the function of the orbicularis oris muscle. The suture then is passed through the soft tissue surrounding the anterior nasal spine or the septal cartilage depending on the optimal direction of suspension (Fig. 5). The suture then is tightened carefully to apply the desired amount of lift to the upper lip (Fig. 6).
A second suture may need to be placed to refine the lip’s position further. Any signs of notching on the lip skin after placement of the suspension suture are addressed by additional subcutaneous undermining lateral to the notching until there is a smoother transition.
The columella now is advanced upward and outward, taking up the excess skin. This step has the added benefit of increasing the nasal tip projection, which many patients lack to some degree. For patients with excessive nasal tip projection before the lip suspension, a tip rhinoplasty will need to be performed to decrease the tip’s projection. For patients with a hanging columella, the caudal septum may be shortened to correct this deformity. Any excess skin from the lip-lift within the nasal vestibule should be excised. The columella is reattached to the caudal septum with 4-0 PDS sutures, and the mucosal incisions are closed with 4-0 plain gut suture.
Results
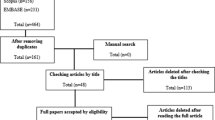
A retrospective review identified 92 patients (89 females and 3 males) who had undergone the no-scar lip-lift procedure (Fig. 7) between July 2005 and July 2009 by the senior author (E.Y.). The majority of the procedures were performed in conjunction with other facial rejuvenation procedures in the operating room with the patient under general anesthesia. Only 34 patients had undergone the procedure in the office setting under local anesthesia. The age range was 18–59 years (mean, 34 years). The mean follow-up period was 10 months (range, 2–26 months). All the patients were thought to have a long upper lip in relation to their facial aesthetics preoperatively. In our patient population, we found four main categories of a long upper lip: phenotypic variation (Fig. 8), postrhinoplasty (Fig. 9), post-lip fillers (Fig. 10), and senescent/ptotic condition (Fig. 11).
a The intranasal incision in the right nostril is demonstrated starting from the nasal floor (solid black line), proceeding up the nasal septum as a transfixion incision, and continuing as an intercartilaginous incision (dashed black line). This incision is continued on the contralateral nasal floor and between the upper and lower lateral cartilages (not shown). The nasal tip is approached through this incision and undermined in the subcutaneous plane (light blue). The soft tissues of the upper lip are elevated in the subcutaneous plane above the orbicularis oris muscle fascia in an area defined by one-half the height of the upper lip and the width of the nasal base (light blue). b A 3-0 supramid (S. Jackson, Inc., Alexandria, VA, USA) suspension suture (black line) is passed via the intranasal incision into the previously dissected subcutaneous plane and grabs the superficial orbicularis oris muscle and fascia at approximately one-half the height of the upper lip. The width of the orbicularis oris grabbed is approximately 1–1.5 cm. The suture then is anchored to the anterior nasal spine and tightened to shorten the central upper lip. c The excess upper lip skin then is redistributed upward into the nasal vestibule, where any excess tissue can be excised. The columellar subunit is lifted upward and outward (black arrows), then secured to the nasal septum or anterior nasal spine. This adds projection to the nasal tip and slight tip rotation
A 21-year-old woman who has a phenotypic variation of a long upper lip with poor sagittal projection. Top Preoperative views. Bottom Postoperative views 10 months later. Note the shortened upper lip with improved incisor show in the anteroposterior view and improved sagittal projection in the lateral view
A 36-year-old woman who has a postrhinoplasty long upper lip with moderate sagittal projection and poor vermillion show. Top Preoperative views. Bottom Postoperative views 12 months later. Note the shortened upper lip with improved incisor and vermillion show in the anteroposterior view and improved sagittal projection in the lateral view
A 59-year-old woman who has a senescent/ptotic long upper lip with poor sagittal projection. Top Preoperative views. Bottom Postoperative views 9 months later. Note the shortened upper lip with improved incisor and vermillion show in the anteroposterior view and improved sagittal projection in the lateral view
Pre- and postoperative photographs were analyzed by three plastic surgeons in terms of the following categories: lip height, sagittal lip projection (“pout”), incisor show, and vermillion show. In each category, the surgeon was asked to classify the lip as showing improvement versus no change. Where the result presented a discrepancy, it was recorded with the vote of a two-thirds majority for the purpose of the study.
The categories demonstrated the following improvements: shortened lip height (n = 78, 85%), increased sagittal projection (n = 73, 79%), increased incisor show (n = 68, 74%), and increased vermillion show (n = 23, 25%) (Table 1). None of the patients demonstrated worsening of symptoms in any category. The majority of the patients (88%) demonstrated improvement in two or three categories (Table 2).
None of the patients requested removal of the suture, and the complications were minimal. Two patients experienced a small suture abscess requiring an incision in the office, and one patient had loosening of the suture 2 days postoperatively, requiring replacement in the office with the patient under local anesthesia. Most patients experienced some mild paresthesias and hypokinesis of the upper lip after the surgery, likely due to the dissection and the postoperative edema. However, all spontaneously resolved within a few weeks. None of the patients experienced synechia or external valve airway problems.
Discussion
The long upper lip is a difficult problem to address in a large portion of the population without significant facial rhytids, and a visible scar often is unacceptable in a younger cosmetic patient [8]. The previously described techniques of nasal base excision and vermillion advancement have limited applications and cannot be used universally. The nasal base excision is a reliable technique for older patients with significant rhytids, where the scar is better camouflaged. This technique is shown to be effective and has a low revision rate [9].
Recently, Santanché and Bonarrigo [10] described their nasal base excision technique, limiting the excision immediately below each nostril and preserving a columella skin bridge to better camouflage the scar. They deal with the columella skin by elevating it from the lower lateral cartilages and advancing it upward. Moveover, the vermillion advancement disrupts the central aesthetic components of the upper lip and risks an amorphous transition from the vermillion to the upper lip skin.
The complications associated with the vermillion advancement are asymmetry, hypertrophic scarring, and suture spitting [4]. Whereas some have encouraged the abandonment of this procedure due to the unsatisfactory outcome [11], others think this technique may be of some use for the lateral aspects of the lips [9].
Our lip suspension technique helps to address the long upper lip without a visible scar, which may be of some benefit for the younger cosmetic patient. The central premise of the lip suspension is enhancement of the overall upper lip aesthetics by shortening of the upper lip’s central portion. The initial frontal assessment of an aesthetically pleasing lip demonstrates well-defined landmarks, including the bilateral philtral columns, Cupid’s bow, white roll, and the dry vermillion [12]. The relationship of the upper lip to the surrounding structures can be appreciated in a sagittal view, which shows the nasolabial angle and upper lip projection. On a perpendicular line drawn from the Frankfort horizontal, the upper lip should be 2 mm anterior to the lower lip and 4 mm anterior to the chin. By making the incision intranasally, the central lip landmarks are not violated or significantly distorted.
From our earlier attempts with the suspension suture, we discovered that by limiting the dissection to half the vertical height of the lip and placing the suture at the end of this dissection plane, tethering of the lip and interruption of oral competence did not occur as with a suture placed near the white roll. This compromise allows an elevation of the lip and retained oral competence while the shape of the upper lip in the lateral view is changed from a convex or straight appearance to a more youthful concave appearance. An added benefit seen is the slightly opened position of the oral aperture, allowing a slight incisor show with the lips in their new relaxed position. This sensual appearance does not affect the lip’s dynamic function. Moreover, a significant change is seen in the lateral view of each patient, namely, a change in the lip contour from a straight line or convexity to a concavity, thus creating the appearance of fullness and pout. Most importantly, all the patients who underwent the lip suspension procedure were happy with their results.
We found four major categories of patients who presented with a long upper lip. The first group has what we consider a phenotypical long upper lip. These patients tend to be younger, have had no prior facial surgery, and have good facial proportions. The second group has the senescent, long upper lip. These patients have a loss of skin tone, fat atrophy, and facial rhytids. The upper lip tends to elongate and flatten, leading to a lack of incisor show [1, 5, 6]. The third group consists of the postrhinoplasty patients who may have had disruption of the columella’s relationship to the surrounding structures, thus elongating the upper lip. The fourth group comprises the post-lip filler patients, for whom the addition of volume not only increases the vermillion show but also increases the lip length. Some patients are seen with an excessive amount of filler, which causes a loss of the key upper lip landmarks, resulting in an amorphous “sausage-like” lip. Each of these categories benefited from the lip-lift.
Our review had its limitation with patients who at presentation had a long upper lip and facial skeletal discrepancies. Patients with a horizontal or vertical maxillary deficiency have a comparatively longer upper lip in relation to their dentition. This subset of patients is best served with a maxillary advancement or lengthening to correct the primary deformity. However, we believe a lip-shortening procedure could be used as an adjunct of a more invasive maxillary surgery or in lieu of it [13].
The reported technique requires the surgeon to evaluate the upper lip and nose as a subunit to obtain the desired changes to the lip and prevent negative changes to the nose. By avoiding a direct excision technique, adjustments to the lower third of the nose may be required in some cases to accommodate the advancement of the excess upper lip skin. In most patients, an increase in nasal tip projection is well tolerated for overall nasal aesthetics.
A subset of patients with excess nasal tip projection may need a formal nasal tip rhinoplasty to modify the lower lateral cartilages and decrease the tip projection. A hanging columella can be addressed by reducing the caudal septum if the advancement does not correct it initially. However, most patients were corrected to a normal position with slight visibility below the ala on a lateral view. It also is important to evaluate the lip from both the anterior and lateral views for a full assessment of the changes after the lip suspension technique because in the anterior view the lip may appear longer due to repositioning of the columella and nasal tip. However, in the lateral view, the lip clearly will be shorter with improved outward projection. Finally, the lower lateral cartilage footplates can be excised if they appear to be tenting skin into the nasal aperture, possibly obstructing the external nasal valve. With a basic knowledge of the nasal anatomy, this lip suspension can be performed safely.
The lip-lift is meant to provide an additional option to upper lip rejuvenation and is not intended to replace lip fillers. Many patients require addition of volume to improve lip contours via augmentation [6, 14]. However, with a lip-lift procedure, the patient may require less volume replacement to achieve an aesthetic improvement [15].
With any facial aesthetic surgical procedure, the surgeon is working in millimeters, and the slightest change in the sagittal projection or vertical height can drastically change the overall cosmetic outcome. The changes seen are subtle, but that is all most patients really need. The upper lip is shortened enough to give a slight incisor show in the anterior view. Furthermore, the upper lip’s contour changes from convex or straight to a more concave appearance with better outward projection of the vermillion. The major benefit from the lip suspension technique is the lack of a visible scar, which is crucial for a young patient whose scar cannot be adequately camouflaged in rhytids or facial creases. Although some older patients with ptotic upper lips may be candidates for this procedure, we still routinely perform the subnasal skin excision for older patients for whom the scar will not be a major issue.
The reported technique is a simple procedure that can be performed in the office with the patient under local anesthesia or in the operating room in conjunction with other facial rejuvenation procedures. The lip suspension can be reversed easily if the patient is not satisfied with the result by simply removing the suture intranasally. We believe this straightforward procedure can help improve upper lip aesthetics using a single suture and minimal operative time without a noticeable scar.
References
Austin HW (1986) The lip lift. Plast Reconstr Surg 77:990–994
Greenwald AE (1987) The lip-lift. Plast Reconstr Surg 79:147
Hinderer UT (1995) Aging of the upper lip: a new treatment technique. Aesthetic Plast Surg 19:519–526
Felman G (1993) Direct upper lip lifting: a safe procedure. Aesthet Surg J 17:291–295
Guerrissi JO, Sanchez LI (1993) An approach to the senile upper lip. Plast Reconstr Surg 92:1187
Maloney BP (1996) Cosmetic surgery of the lips. Facial Plast Surg 12:265–278
Niechajev I (2000) Lip enhancement: surgical alternatives and histological aspects. Plast Reconstr Surg 105:1173–1183
Rozner L, Isaacs GW (1981) Lip lifting. Br J Plast Surg 34:481–484
Weston GW, Poindexter BD, Sigal RK, Austin HW (2009) Lifting lips: 28 years of experience using the direct approach to rejuvenating the aging mouth. Aesthet Surg J 29:83–86
Santanché P, Bonarrigo C (2004) Lifting of the upper lip: personal technique. Plast Reconstr Surg 113:1828–1835
Wilkinson TS (1994) “Lip lift” resection. Plast Reconstr Surg 94:221
Fanous N (1984) Correction of thin lips: “lip lift”. Plast Reconstr Surg 74:33–41
Jeter TS, Nishioka GJ (1998) The lip-lift: an alternative corrective procedure for iatrogenic vertical maxillary deficiency: report of a case. J Oral Maxillofac Surg 46:323–325
Perenack J (2005) Treatment options to optimize display of anterior dental esthetics in the patient with the aged lip. J Oral Maxillofac Surg 63:1634–1641
Guyuron B (2000) Lip enhancement: surgical alternatives and histological aspects (discussion). Plast Reconstr Surg 105:1184–1187
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Echo, A., Momoh, A.O. & Yuksel, E. The No-Scar Lip-Lift: Upper Lip Suspension Technique. Aesth Plast Surg 35, 617–623 (2011). https://doi.org/10.1007/s00266-011-9655-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-011-9655-6