Abstract
Background
Accurate acetabular component placement may reduce the risk of complication after total hip arthroplasty (THA). While surgeon experience and volume may reduce outliers, little is known how cup positioning accuracy and consistency relates to level of training (resident, fellow, attending) and whether trainee level impacts the magnitude and direction of cup placement errors.
Methods
Ninety patients undergoing posterolateral computer-assisted navigation THA were included for analysis. All surgery was performed by two fellowship-trained orthopaedic surgeons and assisted by a trainee (orthopedic resident (PGY 1–5) or fellow in adult reconstruction). In order to determine accuracy of cup placement in trainees and attendings, we used computer navigation to determine freehand cup placement by the trainee, then by the attending surgeon. Final cup inclination and version were determined and recorded by computer-assisted surgical navigation. Comparison of consistency in cup inclination and anteversion was made on values obtained by residents, fellows, and attendings and final values provided by the navigation system. In addition, to assess the role of training and repetition, acetabular cup inclination and version were compared between fellows during the first half and the second half of their training year. All comparisons were performed with the Student t-test except for comparison of rate of deviation from the safe zone, which were performed with the chi-square test. The level of significance was defined as p values ≤ 0.05 with 95% confidence interval, and trend toward significance was defined as p values ≤ 0.1.
Results
Inclination deviation from the final position and cup version deviation from the final position were statistically significant between resident vs attendings (p < 0.001 (inclination), p < 0.001 (version)), fellow vs attendings (p < 0.001 (inclination), p < 0.001 (version)), and all trainee vs attendings (p < 0.001 (inclination), p < 0.001 (version)). In all comparisons, the attending surgeons placed the cup closer to the final cup position than both resident and fellows. Proportion of inclination deviation from the safe zone of residents was significantly higher than of attendings (p < 0.001) but no significant difference was observed between fellows and attending (p = 1.00). Compared to residents, fellows demonstrated lower proportion of inclination deviation from the safe zone of 3.3% vs 23.3% for fellows vs residents (p = 0.002) and tended to implant the cups in a more horizontal position (45.6 ± 6.6° [SD] and 42.7 ± 4.3°, respectively, p = 0.04). Compared to fellow, residents tended to implant the cup in a more anteverted position than the final cup version (9.6 ± 6.7° and 6.74 ± 5.6° [SD], p = 0.034). There was no statistically significant difference in cup position between attendings’ free-hand and final (computer assisted) cup placement.
Conclusion
Accurate and consistent acetabular cup placement improves with level of training. Accurate and consistent acetabular cup version is harder to master as compared to acetabular cup inclination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate cup positioning during total hip arthroplasty (THA) is important in order to maximize range of motion, and minimize impingement, instability, and wear [1,2,3,4]. Malposition of acetabular component is an important cause of hip instability, which is the most common cause for THA revision in the USA [5]. The most commonly referenced acetabular component “safe zone” for acetabular component orientation was introduced by Lewinneck et al., who described safe range of acetabular cup placement as 5–25° of anteversion and 30–50° of abduction, with a 1.5% dislocation rate within the safe range compared to 6.1% when outside the safe range [6]. Achieving accurate and consistent acetabular cup positioning is difficult and subject to error because most acetabular cups are currently implanted with freehand technique that relies on the surgeon’s ability to accurately assess patients’ pelvic position and intra-operative identification of anatomic landmarks to guide accurate cup placement [7]. Consistency in freehand cup positioning requires repetition and experience [7]. Prior studies showed that risk of acetabular cup malpositioning correlates with number of cases performed by the surgeon, with lower-volume attending surgeons having a greater risk of cup malpositioning as compared to higher-volume attending surgeons [8,9,10].
While new technologies, such as imageless computer-assisted navigation [11, 12] and CT-based navigation [13], have been shown to greatly improve accuracy of cup placement irrespective of the surgeon’s level of experience, most acetabular components worldwide are implanted with freehand technique [7]. Therefore, ability to place acetabular cup with freehand technique remains a crucial skill for orthopaedic residents and fellows. To our knowledge, the effect of residency and fellowship training on the accuracy of cup positioning is unknown.
This study seeks to determine if surgeons under training (trainees) can position the acetabular component as accurately as attending-level surgeons. The study also seeks to evaluate to what extent fellowship and residency training improves the ability to accurately position the acetabular component.
Materials and methods
Patients and demographics
Between September 2017 and April 2018, 90 patients (41 males and 52 females) who underwent primary THA at a single center were included in this study (Table 1). All surgery was performed by two fellowship-trained orthopaedic surgeons through a posterolateral approach, utilizing surgical navigation and assisted by a trainee (resident (PGY 1–5) or fellow). Sixty surgeries (68%) were assisted by an adult reconstruction fellow and 30 (32%) by an orthopaedic resident. Institutional review board approval were obtained prior to the initiation of the study.
Data acquisition
Imageless computer navigation system was used for the placement of the components. Prior to exposure of the hip, patient’s horizontal and frontal planes are established through registration steps of the navigation system [12].
Data was collected in the following sequence: after acetabular reaming, the trainee manually positioned the acetabular component or a slightly undersized trial to the best of his/her abilities within the safe zone [6] (inclination of 40 ± 10° and anteversion of 15 ± 10°). Navigation was used to record cup position information, which remained blinded to the surgical team. The attending surgeon then manually positioned the acetabular component to the best of his/her abilities and real-time cup position information was again recorded. Finally, computer navigation live feedback was used to determine the final position of the acetabular component, and adjustments to the position were achieved by the attending surgeon if necessary. For each of the cases, we therefore obtained freehand inclination and anteversion values for the trainee and the attending surgeon, as well as final “unblinded” navigated values.
Statistical analysis
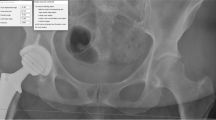
In order to assess precision of cup placement by trainees and attending surgeons, the following parameters were analyzed (Fig. 1). First, cup inclination and anteversion values were expressed as means and standard deviations as a parameter reflecting dispersion from the mean value. Second, inclination and version deviation from the final position were calculated by subtracting the final cup inclination and version values from the ones obtained blindly. For inclination, a positive value indicated that freehand cup placement was more vertical than the final one; a negative value indicated that freehand cup placement was more horizontal than the final one. For version, a positive value indicated that freehand cup placement was more anteverted than the final one; a negative value indicated that the freehand cup placement was less anteverted than the final one. Third, the proportion of patients in which freehand placement is outside the ranges of the safe zone was reported. Cup inclination is deemed to be outside the safe zone range if the inclination is < 30° or > 50°. Cup version is deemed to be outside the safe zone range if the version is > 25° or < 5°.
Schematic of acetabular cup position (inclination and version) as read by the navigation system. After acetabular reaming, the trainee (resident or fellow) manually positioned the acetabular component or a slightly undersized trial to the best of his/her abilities within the safe zone (inclination (Inc(fellow,res)) and version (Vers(fellow,res))). Navigation was used to record cup position information, which remained blinded to the surgical team. The attending surgeon then manually positioned the acetabular component to the best of his/her abilities and real-time cup position information was again recorded (Inc(att) and Vers(att)). Finally, computer navigation live feedback was used to determine the final position of the acetabular component (Inc(final) and Vers(final))
Cup inclination and version, and inclination and version deviation from the final position, as well as proportion of inclination and version deviation from the safe zone, were compared between (a) attendings and trainees, (b) attending and arthroplasty fellows, (c) attendings and residents, (d) residents and fellows, (e) fellows during the first half and the second half of their training year, and (f) attending’s initial vs final position. All comparisons were performed with the Student t-test except for comparison of rate of deviation from the safe zone, which were performed with the chi-square test. The level of significance was defined as p values ≤ 0.05 with 95% confidence interval, and trend toward significance was defined as p values ≤ 0.1.
Results
Trainee vs. attending surgeon’s comparison
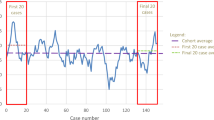
There was no statistically significant difference between attending’s initial cup inclination and final cup inclination (43.7 ± 3.3° [SD] and 43.1 ± 3.10°, p = 0.21). There was no statistically significant difference between the attending’s and trainee’s overall cup inclination (43.7 ± 5.3° [SD] and 43.7 ± 3.3°, for trainees and attendings, respectively, p = 0.92) (Table 2). However, when comparing the inclination deviation from the final position, trainees tended to place cups more vertically than attendings (4.7 ± 4.1° [SD] and 1.1 ± 1.7°, for trainees and attendings, respectively, p = < 0.001 (Table 2)). Furthermore, trainees deviated more frequently from the safe zone than attendings (10% vs 1.11%, for trainees and attendings, respectively, p = 0.03) (Table 2; Fig. 2).
There was no statistically significant difference between attending’s initial cup version and final cup version (23.2 ± 5.3° [SD] and 23.6 ± 5.14°, p = 0.58). There was no statistically significant difference between the attending’s and trainee’s overall cup version (22.1 ± 7.5° [SD] and 23.2 ± 5.3°, for trainees and attendings, respectively, p = 0.28) (Table 2). When comparing the version deviation from the final position, trainees tended to place the cup more anteverted than attendings (7.7 ± 6.1° [SD] and 1.1 ± 1.7°, for trainees and attendings, respectively, p < 0.001) (Table 2). There was no statistically significant difference in the proportion of version deviation from the safe zone between trainee and attending (36.7% vs 34.4%, for trainees and attendings, respectively, p = 0.76) (Table 2; Fig. 2).
Fellow vs attending comparison
There was no statistically significant difference between the attending’s and fellow’s cup inclination (42.7 ± 4.3° [SD] and 43.7 ± 3.4°, for fellows and attendings, respectively, p = 0.2) (Table 3). When comparing the inclination deviation from the final position, fellows tended to place the cup more vertically than attendings (4.3 ± 3.2° [SD] and 1.0 ± 1.6°, for fellows and attendings, respectively, p < 0.001) (Table 3). There was no statistically significant difference in the proportion of inclination deviation from the safe zone between fellows and attending (3.3% vs 1.7%, for fellows and attendings, respectively, p = 1.00) (Table 3).
There was no statistically significant difference between the attending’s and fellow’s cup version (21.6 ± 6.9° [SD] and 23.6 ± 4.9°, for fellows and attendings, respectively, p = 0.06). When comparing the version deviation from the final position, fellows tended to place the cup more anteverted than attendings (6.7 ± 5.6° [SD] and 1.0 ± 1.5°, for fellows and attendings, respectively, p < 0.001) (Table 3). There was no statistically significant difference in the proportion of version deviation from the safe zone between fellows and attendings (35% vs 36.7%, for fellows and attendings, respectively, p = 0.85) (Table 3).
Resident vs attending comparison
There was no statistically significant difference between the attending’s and resident’s cup inclination (45.6 ± 6.6° [SD] and 43.9 ± 3.1°, for attendings and residents, respectively, p = 0.23) (Table 4). When comparing the inclination deviation from the final position, residents tended to place the cup more vertically than attendings (5.5 ± 5.4° [SD] and 1.3 ± 2.0°, for attendings and residents, respectively, p < 0.001) (Table 4). Residents demonstrated higher proportion of inclination deviation from the safe zone than attendings (23.3% vs 0%, for residents and attendings, respectively, p < 0.001) (Table 4).
There was no statistically significant difference between the attending’s and resident’s cup version (23.3 ± 8.4° [SD] and 22.3 ± 6.1°, for residents and attendings, respectively, p = 0.6) (Table 4). However, when comparing the version deviation from the final position, residents tended to place the cup more anteverted than attendings (9.6 ± 6.8° [SD] and 1.4 ± 2.0°, for residents and attendings, respectively, p < 0.001) (Table 4). There was no statistically significant difference in the proportion of version deviation from the safe zone between residents and attendings (40.0% vs 30.0%, for residents and attendings, respectively, p = 0.42) (Table 4).
Resident vs. fellow comparison
When compared to fellows, residents tended to implant the cup in a more vertical position (42.7 ± 4.3° and 45.6 ± 6.6° for fellows and residents, respectively, p = 0.04). Fellows demonstrated significantly lower proportion of inclination deviation from the safe position (3.3% vs 23.3% for fellows vs residents, p = 0.002. Two out of 60 cups implanted by fellows and seven of 30 cups implanted by residents had a measured inclination greater than 50 degrees (p = 0.035).
There was no statistically significant difference between the fellows’ and residents’ cup version (21.6 ± 6.9° and 23.3 ± 8.4° for fellows and residents, respectively, p = 0.33). When compared to the final cup version, residents tended to place the cup in a more anteverted position than fellows (6.7 ± 5.6° and 9.6 ± 6.8° for fellows and residents, respectively, p = 0.035). There was no statistically significant difference in the proportion of version deviation from the safe zone between residents and fellows (35 vs 40%, for fellows and residents, respectively, p = 0.63).
Beginner vs. advanced training comparison
Compared to fellows in the first half of their training, fellows in the second halves of their training had lower proportion of cup version deviation from the safe zone (45% vs 17%, for fellows in the first vs second halves of their training, respectively, p = 0.04) (Table 5). No other statistically significant changes in cup placement accuracy were noted for fellows between the first and second halves of their training periods. Compared to attendings, fellows in the second half of the training still placed the cups more anteverted and more vertical from the cups’ final position (inclination deviation from the final position: 4.2 ± 2.5° vs 1.0 ± 1.6°, p = 1.7E − 6; version deviation from the final position: 6.6 ± 4.4° vs 1.0 ± 1.6°, p < 0.001 for fellows in the second halves of their training vs attendings).
Discussion
Malposition of acetabular cup placement during total hip arthroplasty (THA) is one of the most important factors for decreased range of motion, impingement, instability, wear, and dislocation [1,2,3,4,5]. While recent advancement of the technology of imageless navigation and CT-based navigation have been shown to greatly improve accuracy of cup placement irrespective of the surgeon’s level of experience [12], most acetabular components in the USA are implanted with freehand technique. Inaccuracy and inconsistencies associated with freehand techniques have been described by various authors, with only 25–70% of the cups placed within the safe zone [14, 15]. Accuracy of cup placement using freehand technique relies on achieving a stable, strict lateral decubitus of the pelvis, intra-operative identification of anatomic landmarks to guide cup placement, and consistency that comes from training and repetition [15, 16]. Lee et al. showed that attending surgeons reached competency of optimal cup positioning within 50 cases [17]. In the study, Lee et al. also showed that most of the failure of freehand cup placement was due to deviation of cup version from the safe zone [17].
In this study, we found that accuracy of cup placement positively correlates with level of training, with number of years in training correlating with higher accuracy of cup placement. Accuracy in cup anteversion is harder to achieve than that of cup inclination, as shown by the absence of statistically significant difference in proportion of inclination deviation from the safe zone between fellow vs attending but the presence of statistically significant difference in the rate of version deviation from the safe zone between both resident vs attending and fellow vs attending. This finding suggests that the learning curve for cup version is steeper for all levels of trainings as compared to cup version. Moreover, less-experienced trainees tended to place the acetabular cup with higher inclination, which has been shown to correlate with higher risk of dislocation [6, 18, 19].
We also found that fellows were able to place the cup more accurately than residents, highlighting the value of fellowship training in arthroplasty. In this study, we also observed that the fellows in the second half of training were able to place the cup more accurately from version standpoint than fellows in the first half of the training. This finding complements and is in line with the prior study by Mahure et al. who showed that TKA and THA performed by fellowship-trained surgeons had significantly shorter surgical times and achieved higher Activity Measures for Post-Acute-Care scores and patients were discharged home more often than those whom TKA(Total knee arthroplasty) and THA are performed by non-fellowship-trained surgeons [20].
Our findings in this study are in line with prior studies by Callanan et al. [8] and Bosker et al. [15]. Callanan et al. showed that surgeon experience is an independent factor for malpositioning in inclination only and combined inclination and version [8]. Bosker et al. showed that when orthopedic attending surgeons and residents were asked to hit goal targets for abduction and version angles, mean inaccuracies for inclination were 4.1° and 6.3° and mean inaccuracies for version were 5.2° and 5.7° for attending surgeon and residents respectively [15].
There are several limitations to our study. One limitation is the accuracy of computer navigation system to obtain the true inclination and version of implanted acetabular cup. In a prospective cohort study of 356 primary THA patients comparing computer navigation system measurements to post-operative EOS imaging, the mean absolute difference between navigation and EOS imaging was 2.17° ± 2.5° for inclination and 2.97° ± 4.05° for anteversion [21]. A cadaveric study of 12 hips usingcomputer navigation system evaluated by computed tomography found inclination was within 4.2° ± 3.2° and anteversion within 4.0° ± 4.0° [22]. While CT scan has been deemed as the gold standard for acetabular cup inclination and version measurement, increased health care cost and ill effect of radiation exposure have deemed CT as an impractical way to measure inclination and version of a large number of patients [23]. Second, we used Lewinneck safe zone as the target for acetabular cup placement. Several studies showed that significant amounts of hip dislocations are within the Lewinneck safe zone [24, 25] and the true safe zone might be patient dependent and based on each patient’s sagittal changes of the spine-pelvis-hip during postural changes [26, 27], combined anteversion of the acetabular and femoral components [2, 28], and femur motion [29]. Lastly, only 30 of 90 cases in this study were assisted by residents PGY 1–5 (3 cases by PGY 1, six cases by PGY 3, five cases by PGY 4, and 16 cases by PGY 5), thus limiting our ability to perform sub-analysis of accuracy of cup placement within the residents’ sub-group.
Conclusion
Accurate and consistent acetabular cup placement improves with level of training. Both fellows and residents tend to place the cup more vertically and anteverted than attendings. Fellows were able to place the cup with more accurate version and inclination than residents. Fellows in the second half of training were able to place the cup with more accurate version than fellows in the first half of the training. Attendings were able to place the cup with more accurate version and inclination than fellows on the second half of training, fellows on the first half of training, and residents. Accurate and consistent acetabular cup version is harder to master compared to acetabular cup inclination.
Availability of data and material
Data supporting the findings of the study are available from the corresponding author upon request.
References
McCollum D, Gray W (1990) Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res 261:159–176
Jolles B, Zangger P, Leyvraz P (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 17(3):282–288
Del Schutte HJ, Lipman AJ, Bannar SM, Livermore JT, Ilstrup D, Morrey BF (1998) Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty 13(6):621–626
D’Lima D, Urquhart AG, Buehler KO, Walker RH, Colwell CW (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am 82(3):316–321
Sculco P, Austin MS, Lavernia CJ, Rosenberg AG, Sierra RJ (2016) Preventing leg length discrepancy and instability after total hip arthroplasty. Instr Course Lect 65:225–241
Lewinnek G, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2):217–220
Sarin V, Pratt W, Bradley G (2005) Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplasty 20(7):887–891
Callanan M, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H (2011) The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res 469(2):319–329
Kim S,Lim YW, Kwon SY, Jo WL, Ju SH, Park CJ,Lee CW, Kim YS (2017) Level of surgical experience is associated with change in hip center of rotation following cementless total hip arthroplasty: a radiographic assessment. Plos One 12(5): e0178300
Dorr L, Malik A, Wan Z, Long WT, Harris M (2007) Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res 465:92–99
Davenport D, Kavarthapu V (2016) Computer navigation of the acetabular component in total hip arthroplasty: a narrative review. EFFORT Open Rev 1(7):279–285
Jacob I, Benson J, Shanaghan K, Gonzalez Della Valle A (2020) Acetabular positioning is more consistent with the use of a novel miniature computer-assisted device. Int Orthop 44(3):429–435
Iwana D, Nakamura N, Miki H, Kitada M, Hananouchi T, Sugano N (2013) Accuracy of angle and position of the cup using computed tomography-based navigation system in total hip arthroplasty. Comput Aided Surg 18:187–194
Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K (2004) The accuracy of free-hand cup positioning–a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop 28(4):198–201
Bosker B, Verheyen CCPM, Horstmann WG, Tulp NJA (2007) Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg 127:375–379
Sanchez-Sotelo J, Berry D (2001) Epidemiology of instability after total hip replacement. Orthop Clin North Am 32:543–552
Lee Y-K, Biau DJ, Yoon BH, Kim TY, Ha YC, Koo KH (2014) Learning curve of acetabular cup positioning in total hip arthroplasty using a cumulative summation test for learning curve (LC-CUSUM). J Arthroplasty 29(3):586–589
Kelley S, Lachiewicz P, Hickman J, Paterno S (1998) Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop Relat Res 355:163–170
Newington D, Bannister G, Fordyce M (1990) Primary total hip replacement in patients over 80 years of age. J Bone Joint Surg Br 72:450–452
Mahure S, Feng JE, Schwarzkopf RM, Long WJ (2020) The impact of arthroplasty fellowship training on total joint arthroplasty: comparison of peri-operative metrics between fellowship-trained surgeons and non-fellowship-trained surgeons. J Arthroplasty 10:2820–2824
Gross A, Safir OA, Kuzyk PRT, Sculco PK, Wolfstadt J, Girardi BL, Fichman SG, Muir JM (2018) Optimizing leg length and cup position: a surgical navigation tool. Seminars in Arthroplasty 29(3):157–160
Cross M, Schwarzkopf R, Miller TT, Bogner EA, Muir JM, Vigdorchik JM (2017) Improving registration accuracy during total hip arthroplasty: a cadaver study of a new, 3-D mini-optical navigation system. Hip Int 28(1):33–39
McArthur B, Cross M, Geatrakas C, Mayman D, Ghelman B (2012) Measuring acetabular component version after THA: CT or plain radiograph? Clin Orthop Relat Res 470(10):2810–2818
Abdel M, Roth P, Jennings MT, Hanssen AD, Pagnano MW (2016) What safe zone? The vast majority of dislocated THAs are within the Lewinneck safe zone for acetabular cup revision. Clin Orthop Relat Res 474(2):386–391
Dorr L,Callaghan J (2019) Death of the Lewinneck “safe zone”. J Arthroplasty 34: 1–2
Lazennec J-Y, Brusson A, Rousseau M (2013) Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res 99:S87–S103
Lazennec J-Y, Charlot N, Gorin M, Roger B, Arafati N, Bissery A, Saillant G (2014) Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat 26:136–144
Komeno M, Hasegawa M, Sudo A, Uchida A (2006) Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics 29:1104–1108
Esposito C, Gladnick BP, Lee YY, Lyman S, Wright TM, Mayman DJ, Padgett DE (2015) Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty 30:109–113
Acknowledgements
This study was partially funded by the generous contribution of William and Carol Browne.
Author information
Authors and Affiliations
Contributions
PKS and AGDV conceived and designed the analysis and collected the data. VJS, YC, PKS, and AGDV performed the analysis and wrote the manuscript. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Institutional review board approval and patient consent were obtained prior to the initiation of the study.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suhardi, V.J., Chiu, Yf., Sculco, P.K. et al. Accuracy of acetabular cup placement positively correlates with level of training. International Orthopaedics (SICOT) 45, 2797–2804 (2021). https://doi.org/10.1007/s00264-021-05165-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05165-4