Abstract
Purpose
The purpose of this study is to discuss the mechanical function of subchondral bone cysts and its relationship with Wolff’s law.
Methods
One hundred forty symptomatic knees (120 patients) with osteoarthritis were subjected to MRI before high tibial osteotomy (HTO). Subchondral bone cysts (SBCs) were detected on 72 knees of these 140 knees. SBCs, bone marrow lesion (BML), and hip-knee-ankle (HKA) axis were measured by using validated methods. After HTO, the evolution of cysts was evaluated on MRI performed with a five year follow-up on the 72 knees with pre-operative cysts.
Results
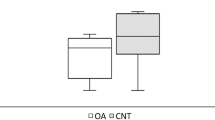
At baseline, 70 (97%) of these 72 knees had a BML surrounding the SBCs; the maximum cyst volume was 874 mm3 and the average cyst volume 9. 6 ± 4.1 mm3. In the subregions where cysts were present, adjacent cartilage was still present without full thickness defects. The mean pre-operative hip-knee-ankle angle was 7.3 ± 3 degrees (0° to 14°) of varus and differed significantly (p = 0.01) between the 68 knees without cysts (average 3 ± 2 degrees) and the 72 knees with cysts (average 9.2 ± 4 degrees). Five years after HTO, the number of cysts had decreased, the maximum cyst volume was 532 mm3, and the average cyst volume was 6.3 ± 2.8 mm3.
Conclusion
Regression of subchondral bone cysts may be related to restoration of an appropriate load at the subchondral bone. With applying poroelasticity to bone mechaincs, this finding may suggest that SBCs and BMLs may be a physiological adaptation to mechanic overload. More basic research is needed to prove this matter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subchondral bone cyst (SBC) formation [1] is frequently present on radiographs in knee osteoarthritis (OA). When the knee is visualized by using magnetic resonance imaging (MRI), SBCs appear more frequently [2] than on radiographs, and SBCs are detected in 50% of subjects with symptomatic knee OA.
Most of the studies about SBCs have been descriptive and related to their prevalence in OA. Among the different theories that are proposed to explain cyst formation, two theories are frequently discussed: for the synovial fluid intrusion theory, a subchondral cyst should develop only in regions with full-thickness cartilage loss where breaches of the articular surface allow synovial fluid and/or synovial tissue to intrude into the subchondral bone; According to the bony contusion theory, a subchondral bone cyst (SBC) forms independently of the adjacent cartilage status and occurs in bone marrow lesions (BMLs); the SBC formation is secondary to subchondral increased loading.
Wolff’s law [3] theorizes that the bone could do adaptive response to load changes. Therefore, the question is: are SBCs and BMLs an adaptive response to increased load in varus knees? If yes, they should decrease when knee malalignment is corrected by high tibia osteotomy (HTO) indicated to treat knee OA in young patients. In neutrally aligned knees, the medial compartment absorbs 60–70% of the compressive force during weight bearing [4]. Since even greater forces are found in the medial compartment in subjects with varus malalignment, consequently high tibia osteotomy that transfers the mechanical axis of the knee from medial to slightly lateral to decrease the load may influence subchondral cysts and bone marrow lesions.
We hypothesized that SBC and BML would decrease after HTO. The aim of this study was therefore to examine if SBCs and BMLs can regress when load is decreased by HTO.
Material and methods
Study patients and data collection
The study included 120 adults (140 knees) with knee osteoarthritis (Table 1). Patients were considered for inclusion if they had knee pain related to medial knee osteoarthritis (OA) with a Kellgren-Lawrence (K-L) grading from 1 to 3 despite conventional treatments such as activity modification, weight loss, physical therapy, analgesics, non-steroidal anti-inflammatory drugs, or injection therapy for at least six months. Inclusion needed that the patient accepted to have HTO as treatment, was less than 65 years old, absence of prior surgery in the knee, and accepted to have MRI pre-operatively and at follow up. Exclusion criteria were severe OA (K-L grade 4) or multi-compartmental OA, and the patients who could not have MRI. All patients were required to wait three months from any prior intra-articular injection before participating. The cohort of the 120 adults was selected (Fig. 1) among the 218 adults younger than 65 years; 70 patients were excluded pre-operatively and eight were excluded post-operatively since they did not accept a second MRI; among those who were excluded pre-operatively, 48 patients had OA with K-L grade 4, or multifocal OA; 22 patients did not accept MRI.
These 120 patients (68 females; mean age 58; range 50–65 years) had a mean BMI of 27.2 kg/cm2 (range 23.8 to 36.5) and had planned to have high tibial osteotomy (HTO). The clinical symptoms were graded according to the Knee Society score [5] and according to the visual analog scale (VAS) pain score before surgery. At the most recent follow up (average of 10 years), the clinical results were graded according to the Knee Society score. Details of any revision surgery were also recorded from hospital charts and clinic records.
Radiograph and magnetic resonance imaging
At baseline, each subject had a weight-bearing anteroposterior tibiofemoral radiograph of the symptomatic knee. Where both knees had OA and were symptomatic, both knees were used. These were independently scored according to the K-L grade [6]. The radiologic features of tibiofemoral OA were graded in each compartment, on a 4-point scale (0 to 3) for individual features of osteophytes and joint space narrowing. Radiographic OA severity of K-L grade 3 was observed in 23% of the patients; 57% had K-L grade 2 OA and the remaining 20% grade 1 OA (Table 1). HKA axis was measured as previously described [7] before performing the osteotomy.
Each subject had an MRI performed on the symptomatic knee at baseline before the osteotomy and five years later after HTO. Knees were imaged in the sagittal plane on the same 2.5-T whole-body magnetic resonance unit (Siemens) by using a commercial extremity coil. The following sequence and parameters were used: a T1-weighted fat-suppressed 3D gradient recall and T2-weighted MRI sequences; field of view, 15 cm; 60 partitions; 512 × 192 matrix; one acquisition time, 9 min 36 s; partition thickness of 1.5 mm. The assessments of SBCs and BMLs were performed on the MRI slice that yielded the greatest lesion size.
SBCs (Fig. 2) were considered as an elliptical or spherical volume of lower (lower as grayscale) bone marrow density (BMD) surrounded entirely by an area of higher BMD (higher grayscale) with a cyst-specific threshold value defining the 50% midpoint intensity values between cyst interior and adjacent bone. We measured the following cyst parameters across the subchondral region: number of cysts, cyst number per total volume (number/cm3), cyst volume per total volume (%), maximum cyst volume (mm3), and average cyst volume (mm3). To assess the reproducibility and the precision of the cyst measurements, a study was performed whereby MRIs were randomized, and cysts were re-identified and re-measured. A cyst was classified as “persistent” if it was present in the same location on both the baseline and follow-up MRIs. The reproducibility for determination of the BMLs was assessed with kappa coefficient (κ value 0.81, p = 0.004). The precision errors (root mean square coefficients of variation) ranged from 0.7 to 3.6%.
The adjacent cartilage morphology and the presence of BMLs were assessed in subregions where SBCs were detected. BMLs were defined as ill-defined areas of increased signal intensity on T2-weighted MRI sequences. Knee cartilage volume was determined by means of image processing on an independent workstation by using the software program Osiris.
These knees with osteoarthritis (OA) were subjected to MRI 5 years after HTO; the same parameters were evaluated with a five year follow-up after plate and screws were removed to allow analysis of subchondral bone with MRI.
Statistical analysis
Demographic variables were determined by the mean, standard deviation, range, and percent. Outcome variables (cysts) were initially assessed for normality and were found to approximate normal distribution to explore the relationship between subchondral bone cysts and alignment or cartilage score. In consideration of a two time-point evaluation (baseline, 5 years follow-up), a repeated-measures ANOVA was used. Differences in cysts and BML status (persistence, regression, volume) by alignment status (HKA angle) were assessed for categorical variables by chi-square tests. A correlation analysis between the characteristics of cysts (volume; number…) and correction of malalignment was conducted by Spearman’s correlation coefficient.
Finally, to determine if the presence or regression of cysts is an independent (adjusted) predictor of a poor or good result after HTO, a multivariate Cox proportional-hazards model was created. All risks factors as demographic and radiographic factors presented in this study were included and particularly age, sex, weight, and osteoarthritis severity.
Results
Descriptive demographic data, cyst characteristics, and alignment at baseline before HTO
Descriptive demographic data
Two hundred-eighteen patients with OA (Fig. 1) were screened for including 120 patients (140 knees) in this study. Demographic data of patients are summarized in Table 1. Patients (68 females) were average 58 years old (range, 50–65 years) with a median body mass index of 29.3 kg/m2 (range, 20.8–34.5 kg/m2). Of the 140 knees, 28 (20%) were radiographically graded K-L 1, 80 (57%) knees were radiographically graded K-L 2, and 32 (23%) were graded K-L 3. Ten patients had died after a mean follow up of six years (range 5 to 9 years), and 110 living patients (130 knees) were evaluated at ten years (range 8 to 12) follow-up.
Cyst characteristics (MRI analysis)
Seventy-two (51%) knees had at least one subchondral bone cyst at baseline on MRI. For patients whose knees had cysts, no significant difference was found in age, weight, height, or BMI (p > 0.24 for all). For the entire sample (140 knees), at baseline before HTO, the total cyst number in the medial compartment varied from none to 55 over the medial proximal tibia and up to 50 in the medial condyle compartment, with a total of 105 cysts in 72 knees. After intravenous contrast administration, 65 knees with cyst (90%) showed contrast enhancement of cysts. BMLs were detected in the subregions containing cysts; cysts were adjacent to or in the middle of BMLs. Of the 72 knees with cyst at baseline, 70 (97%) also had a BML. Knees with several subchondral bone cysts were more likely to have large BMLs. In contrast, those with a BML but no cyst at baseline tended to have small BMLs.
According to the K-L grade, there was no significant difference (p = 0.34) in the severity of OA between the two groups of knees, those without cysts and those with cysts (Table 1). We found no relation between presence of cysts and volume of cartilage in the medial compartment: the mean cartilage volume (1.845 ± 0.347 cm3) was not significantly (p > 0.24) different in medial compartment of those knees with cysts, compared with those with BMLs (1.739 ± 0.435 cm3) only or neither cyst nor BML present (1.823 ± 0. 539 cm3). In the subregions where cysts were present, adjacent cartilage was still present without full-thickness defects.
Before surgery (Table 2), for a total number of 105 cysts, cyst number was 0.4 per cm3 of bone, the cyst volume percentage per total volume was 8.3 ± 2.6% for the medial proximal tibia, the cyst volume percentage per total volume was 12.4 ± 3.5% for the medial condyle, the maximum cyst volume was 874 mm3, and the average cyst volume 9. 6 ± 4.1 mm3.
We found significant positive relationships between alignment and total cyst number: The mean pre-operative hip-knee-ankle angle was 7.3 ± 3 degrees (0° to 14°) of varus and differed significantly (p = 0.01) between the 68 knees without cysts (average 3 ± 2 degrees) and the 72 knees with cysts (average 9.2 ± 4 degrees).
Cyst evolution on MRI 5 years after changes in alignment with HTO
We analyzed the effect of HTO on cyst evolution with MRI at 5-year follow-up.
After surgery, the HKA angle was 4.2 ± 2 degrees of valgus. Five years after HTO, among the 72 knees with cyst at baseline, only 22 knees had no cyst regression. The total cyst number in the medial compartment had decreased from 105 to 52 cysts (Table 2); for a total number of 52 cysts, the cyst number was 0.21 per cm3 of bone, the cyst volume percentage per total volume was 5.2 ± 1.8% for the medial proximal tibia, the cyst volume percentage per total volume was 8.4 ± 2.8% for the medial condyle, the maximum cyst volume was 532 mm3, and the average cyst volume 6.3 ± 2.8 mm3; with a significant decrease as compared with the pre-operative values (p < 0.006 for all). Association was observed between the importance of cyst regression and correction of malalignment (r2 = 0.65). On the most recent MRI, no new cyst was detected on the medial compartment; however, ten new cysts appeared on the lateral compartment.
Among the 68 knees without cyst at baseline, no cyst was detected on the medial compartment, while one cyst occurred on the lateral compartment of eight knees.
Cyst regression is an independent predictor of a good outcome at ten year follow-up
Since regression of cysts was observed, we extended our observation by examining at ten year follow-up the cohort of knees. We analyzed the effect of cyst regression on the risk of another surgery (knee arthroplasty) and on poor or good results after HTO.
At the most recent follow-up (average of 10 years, range 8 to 12 years), the clinical outcome could be analyzed for 130 knees (Fig. 1). Among the 22 knees without any cyst regression, 18 knees (82%) had a subsequent surgery (total knee arthroplasty) due to recurrence of pain with a poor knee score (60 points ± 14), as compared with only two knees (4%) with revision for TKA in the group of 50 knees with cyst regression (Fig. 3); therefore, cyst regression at five years is a predictor of a good outcome at ten years (p < 0.01).
For the other 110 knees without TKA revision at the most recent follow-up, the Knee Scores had progressed significantly (p < 0.01) from a clinical pre-operative knee score of 58 points ± 15 to a ten year follow-up score of 78.2 points ± 16.
Discussion
The main finding of this study is that cysts occur more frequently in knees with malalignment and may regress after correction of malalignment by high tibial osteotomy. The current study highlights the importance of bone cyst lesions and their evolution as a determinant of OA severity, specifically regarding the risk of future knee arthroplasty after HTO. To our knowledge, this study is the first one to examine the longitudinal changes of subchondral cyst structure of the tibiofemoral joint in individuals with varus knee alignment before HTO. Changes were evaluated in combination with the functional outcome on average ten years after HTO. We have some understanding of the mechanical factors (overcorrection) that predict success of a high tibial osteotomy but a limited understanding of other factors that could predict risks of failure of high tibial osteotomy with as consequence a future total knee arthroplasty. The MRI-based findings demonstrated that cysts are a frequent picture in knee OA. As patients with absence of regression of SBCs had greater likelihood of failure of HTO and revision with total knee arthroplasty than were patients with reduction of SBCs, this may help in the discussion with a patient with persistent pain after HTO. In the patient with moderate radiographic OA who does not respond to HTO, demonstration of absence of regression of cysts on MRI may allow earlier consideration for another treatment (arthroplasty).
Wolff’s Law [3] hypothesized that the bone could do adaptive response to load changes with a way of “form follow function” and comply “mathematical law.” Whether the appearance and regression of SBCs can be considered an adaptive response to increased load would assume that they occur when pressure increases and their occurrence decreases the load on cartilage. The first part of this hypothesis (they occur when pressure increase) is confirmed by this study that demonstrates that cyst development is more frequent in knees with malalignment. As cysts regression was observed in the medial compartment after HTO, even in absence of improvement of joint space, their evolution does not appear to be related to the cartilage layer but rather to the pressure change in the subchondral bone. This is in agreement with finite element analysis study [8] supporting the theory that stress-induced bone may be the cause of the development of subchondral bone cysts in osteoarthritis. The second part of this hypothesis (their occurrence decreases the load on cartilage) supposes that occurrence may protect the cartilage from a mechanical point of view. Although we have no direct evidence, this second part is not incompatible with known data on biomechanics: According to finite element analysis [8], and according to the elasticity of the cartilage, the maximum stress after loading the cartilage (with von-Mises stress values) occurs at some distance [9] of the application of the load, i.e., in the subchondral bone below the tidemark in an area without communication with the joint (Fig. 4). The basic bone marrow pressure is generally about 30 mmHg which is approximately one fourth of the systemic blood pressure [11]. The cyst envelope provides a confined environment for the marrow, especially under impact loading. Under loading, the water in the SBCs is confined to the cysts and would bear and distribute loads evenly inside the cysts. Bone marrow pressure changes with varying degrees of loads [12], and the changes in cyst may be (roughly) compared with the inflation that increases the size of a balloon and enhances the bounce of a balloon. As the pressure increases inside the balloon, the external surface of the balloon remains at the same pressure as atmospheric pressure. In the same way when the pressure increases inside the cyst, the pressure on the outer wall of the cyst does not increase or just a little protecting the subchondral bone in contact with the under surface of the cartilage and the cartilage. However, since Wolff’s law [13] considers the bone to be a dry cellular solid and Graphic Statics is one of its theoretical basis, the credibility of Wolff’s Laws has been debated; bones, especially cancellous bones, are poroelastic media― a continuum. Poroelasticity [14, 15], to describe the fluid-solid interactions within a poroelastic media, would probably be more suitable in updating Wolff’s Law.
Stress distribution of a point load in continuum resembles a pressure bulb, a stress contour or a line which connects all points below the tidemark, at which the vertical pressure is the same; in fact, an isobar is a spatial curved surface and resembles a bulb in shape; this is because the vertical pressure at all points in a horizontal plane at equal radial distances from the load is the same as described in Boussinesq’s equation [10]. Pressure at points inside the bulb is greater than that at a point on the surface of the bulb
We acknowledge the limitations to our study. The regression of the cysts could be related to a trophic effect of the osteotomy and not directed related to alignment correction; however, before surgery, knees with cysts had greater malalignment than those without cysts, and association was observed between the importance of cyst regression and correction of malalignment. Another limitation to this analysis is that there were only two time-points’ measurements for cysts. Therefore, it is difficult to affirm that at ten years follow-up, there were no other changes for cyst evolution.
In conclusion, the present study has found correlation of SBCs with malalignment. With applying poroelasticity to bone mechanics, this finding may suggest that SBCs and BMLs may be a physiological adaptation to mechanic overload. Regression of SBCs after HTO may be related to restoration of an appropriate load at the subchondral bone. Wolff’s law is a valid explanation, but this analysis is not strong enough to demonstrate it. Further analysis and more studies are needed.
References
Kon E, Ronga M, Filardo G, Farr J, Madry H, Milano G, Andriolo L, Shabshin N (2016) Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg Sports Traumatol Arthrosc 24(6):1797–1814. https://doi.org/10.1007/s00167-016-4113-2
Crema MD, Roemer FW, Zhu Y, Marra MD, Niu J et al (2010) Subchondral cystlike lesions develop longitudinally in areas of bone marrow edema-like lesions in patients with or at risk for knee osteoarthritis: detection with MR imaging--the MOST study. Radiology 256(3):855–862
Brand RA (2010) Biographical sketch: Julius Wolff, 1836–1902. Clin Orthop Relat Res 468(4):1047–1049
Andriacchi TP (1994) Dynamics of knee malalignment. Orthop Clin North Am 25(3):395–403
Scuderi GR, Sikorskii A, Bourne RB, Lonner JH, Benjamin JB, Noble PC (2016) The knee society short form reduces respondent burden in the assessment of patient-reported outcomes. Clin Orthop Relat Res 474(1):134–142. https://doi.org/10.1007/s11999-015-4370-2
Kellgren J, Lawrence J (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494
Hernigou P, Giber D, Dubory A, Auregan JC (2020) Safety of simultaneous versus staged bilateral opening-wedge high tibial osteotomy with locked plate and immediate weight bearing. Int Orthop 44(1):109–117. https://doi.org/10.1007/s00264-019-04385-z
Dürr H, Martin H, Pellengahr C, Schlemmer M, Maier M, Jansson V (2004) The cause of subchondral bone cysts in osteoarthrosis a finite element analysis. Acta Orthop Scand 75(5):554–558
Arjmand H, Nazemi M, Kontulainen SA, McLennan CE, Hunter DJ, Wilson DR, Johnston JD. (2018) Mechanical metrics of the proximal tibia are precise and differentiate osteoarthritic and normal knees: a finite element study Sci Rep 31;8(1):11478. https://doi.org/10.1038/s41598-018-29880-y
Bogdanov LV, Zakharov VE (2002) The Boussinesq equation revisited. J Physica D: Nonlinear Phenomena 165(3):137–162
Wilkes CH, Visscher MB (1975) Some physiological aspects of bone marrow pressure. J Bone Joint Surg (Am Vol) 57(1):49–57
Gurkan UA, Akkus O (2008) The mechanical environment of bone marrow: a review. Ann Biomed Eng 36(12):1978–1991
Wolff J (1986) The law of bone remodeling. Berlin Heidelberg New York: Springer, (translation of the German 1892 edition)
Detournay E and Cheng AH.-D (1993) Fundamentals of poroelasticity, chapter 5 in comprehensive rock engineering: principles, practice and projects, Vol. II, Analysis and Design Method, ed. C. Fairhurst, Pergamon Press, p. 113–171
Carter DR, Hayes WC (1977) The compressive behavior of bone as a two-phase porous structure. J Bone Joint Surg Am 59:954–962
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Weiguo Wang and Ran Ding are the Co-first author
Rights and permissions
About this article
Cite this article
Wang, W., Ding, R., Zhang, N. et al. Subchondral bone cysts regress after correction of malalignment in knee osteoarthritis: comply with Wolff’s law. International Orthopaedics (SICOT) 45, 445–451 (2021). https://doi.org/10.1007/s00264-020-04809-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04809-1