Abstract
Purpose
To define a new parameter in CT that could make imaging of the contralateral ankle dispensable evaluating the position of the fibula after syndesmotic injury.
Methods
Thirty bilateral CTs of 30 patients were included. Five parameters were defined in axial CT for the injured (_inju) and uninjured (_unin) ankle. Reproducibility was examined for inter-observer and intra-observer reliability. Comparisons for all parameters were performed between the CT scans of both ankles.
Results
All measurements had a high agreement for the inter-observer and intra-observer correlation coefficients. A large interindividual variance could be found between all parameters. If the difference of the anterior tibiofibular distance antTFD_unin and antTFD_inju was less than 2 mm, there was a strong significant pairwise correlation between all parameters between both sides.
Conclusion
Bilateral CT is still to be recommended, as it is the only way to exactly assess anterior posterior reduction of the fibula.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Syndesmotic injuries are commonly associated with ankle fractures ranging between 10 and 45% [1, 2]. The correct reduction of the fibula in the incisura fibularis tibiae is the key criterion for long-term results in ankle fractures with syndesmotic injuries, making this a question of high clinical importance [3,4,5,6]. As conventional radiography has been proven to be unreliable to rule out malpositioning of the fibula, post- or intra-operative computed tomography (CT) is the only way to evaluate the position of the fibula in the incisura fibularis [5, 7,8,9,10]. Thus, bilateral CT control after implantation of a syndesmotic screw or a suture-button device has become a highly recommended procedure in ankle fracture treatment [3, 7,8,9, 11, 12]. Rotation, anterior-posterior translation, and shortening can be exactly assessed by bilateral CT with diastases of 2 to 3 mm [3,4,5, 9]. Alternatively to post-operative scanning, intra-operative CT scans have been established in recent years. Usually, only the injured side is scanned intra-operatively, while most studies on distal tibiofibular measurements involve the uninjured side as well [12,13,14,15]. Thus, despite a high rate of studies conducted in this field, it yet remains unclear whether CT of the uninjured ankle is necessary for exact evaluation. We hypothesized that a newly defined parameter in CT imaging could make the CT of the contralateral ankle dispensable.
Materials and methods
Approval of the local institutional review board for study had been given beforehand (AZ 131/18-ek), and the study was conducted in accordance with the Declaration of Helsinki and the guidelines for Good Clinical Practice. Informed consent was available from all individuals. In a retrospective single-centre (Level I Trauma Center) case series, 30 consecutive bilateral CTs of 30 patients with a syndesmotic injury as part of an ankle fracture and an unsuspicious contralateral ankle were included in this analysis. All fibulae were anatomically reduced in the CT controls. Thus, incorrect length could be excluded as a reason for tibiofibular malreduction. Patients with a plate osteosynthesis through a posterolateral approach were excluded to avoid implant artifacts in the CT for best measurement accuracy. Demographic data of interest were age, gender, and injured side. All CTs were performed bilaterally after the implantation of a syndesmotic screw (3.2 mm, DePuy Synthes) or a suture-button device (TightRope®, Arthrex, Naples, FL, USA). All CT scans were performed within three days after surgery without administration of intravenous contrast medium. Patients were positioned supine and feet-first with the ankles in neutral position. Images were acquired using a multidetector CT scanner (iCT 256, Philips, Netherlands). Routine scan parameters included a tube current of 150 mA, a tube voltage of 100 kv with a collimation of 64 × 0.625 mm. Pitch was 0.329 with a rotation time of 0.5 s. Multiplanar reformations were reconstructed in slice thickness of 1–2 mm in axial, sagittal, and coronal orientation. All patients had given informed consent before surgery and were treated with a similar operative procedure. The surgical treatment of the lateral and medial malleolus as well as of the posterior fragment was performed according to the AO (Arbeitsgemeinschaft Osteosynthese): lateral approach to the fibula, open reduction, and osteosynthesis with a lag screw and neutralization plate. For medial malleolar fractures, a standard medial approach was chosen following open reduction and two lag screws. In case of a posterior tibial fragment (Volkmann’s triangle), indirect reduction and sagittal lag screws were used. Following fracture stabilization, syndesmotic instability was tested by performing the hook test as described previously [16, 17]. After documentation of instability by fluoroscopy, reduction, and retention with a pointed clamp, the surgeon has chosen between a transsyndesmotic screw and a suture-button device (TightRope®) as preferred. The syndesmosis was not reduced completely open but only as far as visible via the lateral approach. Standard fluoroscopy (lateral and mortise view) was applied to control the reduction. All patients received a CT of both ankles as part of the hospital’s standard post-operative procedure.
Assessment of the syndesmotic parameters
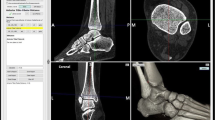
Two blinded observers reviewed all CT scans. The region of interest was selected to be 1 cm proximal from the distal tibial joint as described before [15, 18]. To focus on the same region of the ankle, we defined a standardized approach for selecting the image slices. Based on the coronary views, the axial views depicting the slice 1 cm above the distal tibial joint were chosen (Fig. 1).
Measurement of the syndesmotic parameters
All parameters were defined in axial CT slices depicted on Fig. 2. The measurement was done using MagicWeb® (Visage Imaging, San Diego, CA, USA). A tangent A was aligned to the anterior tibia. A parallel line B was drawn on the anterior margin of the fibula, another parallel C on the posterior margin of the fibula, and a further parallel D on the posterior tibia. The distance AB was defined as the anterior tibiofibular distance (antTFD), BC as the fibular diameter (D_fib), and CD as the posterior tibiofibular distance (postTFD). The tibial diameter (D_tib) was defined as the sum from these three parameters. The relative antTFD (Rel_antTFD) was defined as antTFD/D_tib. All measurements were executed both on the injured (_inju) and uninjured (_unin) side.
Measurement validity
The reproducibility of all parameters was examined with the intraclass correlation coefficient for both inter-observer reliability (measurements made by 2 different observers) and intra-observer reliability (measurements repeated at different points in time by the same observer) for repeated measurements. For all thirty patients, two independent observers, two board-certified orthopaedic surgeons (initials blinded for review), calculated the parameters on CT scans. In addition, for intraobserver reliability testing, the measurements were repeated after a three month interval, with a randomized patient order.
Statistical analysis
Statistical data analysis was performed with SPSS software, version 20.0 (SPSS, Chicago, IL, USA). Inter- and intra-observer agreements were measured with the two-way mixed single measures interclass correlation coefficient with 95% confidence intervals reported (95% CI). The parameters were normally distributed. Comparisons for all parameters were performed with the paired t test between the CT scans of the uninjured ankles and operatively treated injured ankles. The level of significance for statistical analysis was set at p < 0.05.
Results
Demographic data
Patients’ average age was 47.3 (range, 19–82) years with eight males and 22 females. Fourteen patients received a syndesmotic screw, and 16 patients received a suture-button device. According to the AO classification, there were 19 AO 44 B and 11 AO 44 C fractures. All demographic data are presented in Table 1. None of the untreated ankles showed signs of previous injury or other pathologies in the CT.
Inter-observer and intra-observer reliability
All measurements had a high agreement both for the inter-observer (range, 0.83–0.94) and intra-observer (range, 0.71–0.95) correlation coefficients with only one correlation coefficient below 0.8 (postTFD_unin, 0.72 KI [0.38–0.87]) (Table 2) [19].
Comparability
antTFD and D_fib could be measured in all CT scans. It was not possible to measure postTFD on the injured side in eight CT scans due to a displaced posterior tibial fragment. A large interindividual variance could be found between all parameters (Table 3). If the difference of antTFD_unin and antTFD_inju was 2 mm or less than 2 mm (n = 15), there was a strong significant pairwise correlation between the following parameters: antTFD (n = 15; r = 0.89; p < 0.001), D-fib (n = 15; r = 0.83; p < 0.001), and postTFD (n = 11; r = 0.84; p = 0.001) between the injured and uninjured side. With the numbers available, no significant correlation could be detected if the difference was more than 2 mm (antTFD, n = 15, r = 0.39, p = 0.16; D-fib, n = 15; r = 0.40; p = 0.14; postTFD, n = 11, r = 0.43, p = 0.19. Therefore, we defined antTFD as the main parameter of interest. No correlation of postTFD was possible in four pairs of both groups due to the insufficient reduction of the posterior tibial fragment. Relative ratios (Rel_antTFD) could not improve comparability between the injured and the uninjured side.
Discussion
The most important findings of this study were the excellent inter- and intra-observer reliability of the measurements for both the injured and uninjured tibiofibular parameters. However, no significant correlation between the injured and uninjured side could be found with the difference of antTFD_unin and antTFD_inju being more than 2 mm. The calculation of relative ratios did not improve comparability. Thus, the hypothesis must be rejected. Still, the measurement technique seems to be accurate.
Interestingly, in patients with differences of the antTFD_unin and antTFD_inju exceeding 2 mm, the fibular diameter did not correlate between both sides anymore. This can be caused by two separate reasons. First, fibular fracture reduction could be insufficient leading to a fibular shortening and/or malrotation. But reduction of fibular length had been controlled beforehand in the CT. Second, this might be caused by malrotation of the whole fibula. Thereby, in cases without a complete rupture of the interosseous membrane with persistent tibiofibular fixation, rotation would be the consequence of an anterior or posterior shifting of the fibular in relation to the tibia. In current literature, numerous attempts have been made to define normal tibiofibular parameters [15, 20]. Transferring these measurements into actual clinical settings has proven to be difficult. Phisitkul et al. have developed a method to define anterior-posterior reduction in a cadaveric study, which has already been used in clinical studies [20, 21]. Yet, this method depends on an intact or anatomically reduced posterior tibial tubercle. Our data is supported by Davidovitch et al., who did not scan the uninjured side and found no significant difference in the rate of malreduction comparing intra-operative and post-operative CT [13]. The threshold for malreduction was defined by 2 mm as in other studies [13, 22]. Large interindividual but small intraindividual differences including gender-specific differences in the anatomy of the incisura fibularis have been described in anatomic and clinical studies [15, 23]. Certain morphologic variations even have been found to increase the risk of malreduction [24]. This makes it even more important to know the regular anatomy of the patient’s ankle beforehand to evaluate the result of surgery.
In consequence of this data and in accordance with literature, we now use intra-operative CT of both ankles. This is technically more demanding and time-consuming but feasible (Fig. 3). Having the images of both ankles available for direct comparison makes intra-operative CT scanning more efficient. An immediate correction is possible avoiding revision surgery. Alternatively, the uninjured side can be included in a pre-operative CT. Thus, more accurate planning can be done pre-operatively to save time and effort.
In this study, no patients with ORIF of the posterior tibial fragment have been included to have more accurate measurements for first assessment of the method. In the next step, this group must be included for further evaluation, especially as posteriorlateral approaches to posterior fractures gain importance [25].
Altogether this study has several limitations which need to be discussed. The major limitation of this study is the missing standardized operative protocol such as the choice of syndesmotic screw or TightRope® which was selected by the surgeon. Besides, only the hook test was used for testing syndesmotic instability, and alternative tests like the external rotation test were not performed. Fibular length was not measured separately but assumed to be anatomic as a result of the anatomical reduction of the fibula. Additionally, patients treated by a posterior approach were excluded. Furthermore, no evaluation of bilateral fluoroscopic assessment of both sides has been performed, which might have been an alternative to intraoperative CT. We assumed that based on the available literature, intraoperative CT was superior to fluoroscopy. Next, the number of patients included is small. However, the inter- and intraclass reliabilities were mainly excellent, and significant correlations between both sides were found in those patients where antTDF difference was less than 2 mm. Finally, no clinical data were evaluated. To conclude, in order to guarantee intra-operative reduction according to the patient’s individual anatomy, a pre- or intra-operative CT of the uninjured side is recommended in patients with ankle fracture with syndesmotic injury. The antTFD between both ankles should be within 2 mm to prove sufficient fibulotibial reduction. An intra-operative CT image of both ankles has the advantage to react immediately in cases of malreduction avoiding revision surgery.
References
Tornetta P, Axelrad TW, Sibai TA, Creevy WR (2012) Treatment of the stress positive ligamentous SE4 ankle fracture: incidence of syndesmotic injury and clinical decision making. J Orthop Trauma 26:659–661. https://doi.org/10.1097/BOT.0b013e31825cf39c
Jensen SL, Andresen BK, Mencke S, Nielsen PT (1998) Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand 69:48–50
Rammelt S, Zwipp H, Grass R (2008) Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. Foot Ankle Clin 13:611–633, vii–viii. https://doi.org/10.1016/j.fcl.2008.08.001
Sagi HC, Shah AR, Sanders RW (2012) The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma 26:439–443. https://doi.org/10.1097/BOT.0b013e31822a526a
Vasarhelyi A, Lubitz J, Gierer P et al (2006) Detection of fibular torsional deformities after surgery for ankle fractures with a novel CT method. Foot Ankle Int 27:1115–1121. https://doi.org/10.1177/107110070602701219
Weening B, Bhandari M (2005) Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 19:102–108
Gardner MJ, Demetrakopoulos D, Briggs SM et al (2006) Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int 27:788–792. https://doi.org/10.1177/107110070602701005
Marmor M, Hansen E, Han HK et al (2011) Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int 32:616–622. https://doi.org/10.3113/FAI.2011.0616
Miller AN, Carroll EA, Parker RJ et al (2009) Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int 30:419–426. https://doi.org/10.3113/FAI.2009.0419
Rammelt S, Obruba P (2015) An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg 41:601–614. https://doi.org/10.1007/s00068-014-0466-8
Franke J, von Recum J, Suda AJ et al (2012) Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am 94:1386–1390. https://doi.org/10.2106/JBJS.K.01122
Franke J, von Recum J, Suda AJ et al (2014) Predictors of a persistent dislocation after reduction of syndesmotic injuries detected with intraoperative three-dimensional imaging. Foot Ankle Int 35:1323–1328. https://doi.org/10.1177/1071100714549047
Davidovitch RI, Weil Y, Karia R et al (2013) Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg Am 95:1838–1843. https://doi.org/10.2106/JBJS.L.00382
Summers HD, Sinclair MK, Stover MD (2013) A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma 27:196–200. https://doi.org/10.1097/BOT.0b013e3182694766
Dikos GD, Heisler J, Choplin RH, Weber TG (2012) Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma 26:433–438. https://doi.org/10.1097/BOT.0b013e3182535f30
Cotton F (1910) Fractures and joint dislocations. WB Saunders, Philadelphia
Stoffel K, Wysocki D, Baddour E et al (2009) Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis. A cadaveric study. J Bone Joint Surg Am 91:2646–2652. https://doi.org/10.2106/JBJS.G.01537
Beumer A, Swierstra BA (2003) The influence of ankle positioning on the radiography of the distal tibial tubercles. Surg Radiol Anat 25:446–450. https://doi.org/10.1007/s00276-003-0147-5
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Phisitkul P, Ebinger T, Goetz J et al (2012) Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg Am 94:2256–2261. https://doi.org/10.2106/JBJS.K.01726
Kocadal O, Yucel M, Pepe M et al (2016) Evaluation of reduction accuracy of suture-button and screw fixation techniques for syndesmotic injuries. Foot Ankle Int 37:1317–1325. https://doi.org/10.1177/1071100716661221
Thordarson DB, Motamed S, Hedman T et al (1997) The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am 79:1809–1815
Mukhopadhyay S, Metcalfe A, Guha AR et al (2011) Malreduction of syndesmosis--are we considering the anatomical variation? Injury 42:1073–1076. https://doi.org/10.1016/j.injury.2011.03.019
Boszczyk A, Kwapisz S, Krümmel M et al (2018) Correlation of Incisura anatomy with syndesmotic malreduction. Foot Ankle Int 39:369–375. https://doi.org/10.1177/1071100717744332
Bartoníček J, Rammelt S, Tuček M (2017) Posterior malleolar fractures: changing concepts and recent developments. Foot Ankle Clin 22:125–145. https://doi.org/10.1016/j.fcl.2016.09.009
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Annette B. Ahrberg and Ulrich J. Spiegl. The first draft of the manuscript was written by Annette B. Ahrberg, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Approval of the local institutional review board for study had been given (Ethical Committee at the Medical Faculty, Leipzig University, AZ 131/18-ek) in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
Consent to participate
All individuals have given general consent in the use of their data, including imaging, for analysis and publication. This has been approved by the Ethical Committee.
Consent for publication
All individuals have given general consent in the use of their data, including imaging, for analysis and publication. This has been approved by the Ethical Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahrberg, A.B., Hennings, R., von Dercks, N. et al. Validation of a new method for evaluation of syndesmotic injuries of the ankle. International Orthopaedics (SICOT) 44, 2095–2100 (2020). https://doi.org/10.1007/s00264-020-04631-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04631-9