Abstract
Introduction
Several recent studies have reported accurate and reliable use of patient-specific cutting guides (PSCG) for medial opening-wedge high tibial osteotomy (OW-HTO); however, a majority of these are small cases series or ex-vivo reports. The hypothesis of this study was that performing an OW-HTO with PSCG results in a reliable and accurate correction with good or satisfactory patient-reported functional outcomes at a mean of two years. We also hypothesized that the use of PSCG would not increase the rate of specific or non-specific complications.
Methods
In this single-centre, observational study, a prospective cohort of a hundred patients (age < 60 years with isolated medial knee osteoarthritis and significant metaphyseal tibial vara) were included between February 2014 and November 2017 to investigate the safety and accuracy of OW-HTO using PSCG. The accuracy of post-operative alignment was defined by the difference between the desired correction defined pre-operatively and the correction obtained post-operatively measured on CT scan (ΔHKA, ΔMPTA, ΔPPTA). Functional outcomes were evaluated by the difference between the value obtained in the pre-operative questionnaire and that obtained at the last follow-up (mean 2 years) using the KOOS and UCLA activity scale. Intra-operative and post-operative complications were recorded.
Results
The mean patient age was 44.17 ± 6.77 years; no patient was lost to follow-up at a mean of two years. The mean ΔHKA was 1 ± 0.95°, the mean ΔMPTA was 0.54 ± 0.63°, and the mean ΔPPTA was 0.43 ± 0.8°. No significant differences (all p values > 0.05) were observed between the desired correction defined pre-operatively and the correction obtained post-operatively (ΔHKA, ΔMPTA, ΔPPTA). An improvement of 27 ± 25 for the KOOS Pain, 28 ± 26 for the KOOS symptoms, 27 ± 28 for the KOOS ADL, 26 ± 33 for the KOOS sport/rec, 28 ± 38 for the KOOS QOL, and 2.6 ± 2.4 for the UCLA was obtained as compared with the pre-operative values (all p < 0.0001). No procedures observed were abandoned, and the PSCG was well positioned in all cases. The overall complication rate was 32% up to two years post-operatively, most of them being classed as minor events (28%).
Conclusion
Performing an OW-HTO with PSCG produces an accurate correction with good functional outcomes at a mean of two years. Furthermore, there is no increase in the rate of specific or non-specific complications. A study to assess the reproducibility of this technique, regardless of the surgical level, is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of medial opening-wedge and lateral closing tibial osteotomies is to correct varus alignment in the lower limb in order to treat overload in the medial compartment of the knee joint [1].
In the last decade, medial opening-wedge high tibial osteotomy (OW-HTO) has gained increasing popularity, as more and more studies continue to report respectable post-operative outcomes with fewer complications [2, 3]. Accurate correction in all three spatial planes is a pivotal factor to obtain good clinical outcomes [4]. To achieve the ideal planned correction, various planning methods, surgical techniques, and differing instrumentations have been developed: examples of this would include conventional methods (with various intra-operative techniques to assess lower-limb alignment), computer-assisted surgery, and recently the use of patient-specific cutting guides (PSCG) [5, 6]. Several recent studies have reported reliable and accurate correction with the use of PSCG for OW-HTO, but the reports are either small case series [7,8,9] or ex vivo studies [10]. The objectives of this study were (1) to evaluate the accuracy of post-operative lower limb alignment, by comparing the achieved correction to the planned correction, (2) to evaluate the functional outcomes through the KOOS and UCLA activity scale, and (3) to evaluate the number of specific and non-specific complications found in the first 100 patients treated using PSCG in a single surgical centre. The hypothesis of this study was that performing an OW-HTO with PSCG results in a reliable and accurate correction with good or satisfactory patient-reported functional outcomes at a mean of two years. We also hypothesized that the use of PSCG would not increase the rate of specific or non-specific complications.
Methods
Patients
In this single-centre, prospective, observational study, 100 patients undergoing OW-HTO using PSCG, by three senior surgeons, from February 2014 to November 2017 were assessed. Inclusion criteria were patients < 60 years with isolated medial knee osteoarthritis (Ahlbäck ≤ 2//Kellgren and Lawrence < 4) [11] and significant metaphyseal tibial vara (medial plateau tibial angle (MPTA) < 85°). Exclusion criteria were patients with advanced osteoarthritis (Ahlbäck > 2), evidence of symptomatic patellofemoral or lateral knee osteoarthritis, previous surgery, and hardware or bony abnormalities that would interfere with obtaining a high-quality CT scan. Patient consent was collected pre-operatively after they were informed of the procedure in accordance with the principles of the Helsinki declaration. A local ethics committee approved our study protocol prior to the investigation.
In the pre-operative planning stage, the planned correction was first calculated by the surgeon using conventional radiographs (weight-bearing long-leg, A/P, and lateral views). Subsequently, all patients underwent a CT scan. The surgeon took measurements and filled out an order form for the engineer which specified the correction objectives in the frontal and sagittal planes through variations in the hip-knee-ankle (HKA) angle, medial proximal tibia angle (MPTA), and posterior proximal tibia angle (PPTA).
The CT scan protocol consisted of acquiring images centered on the femoral head, the knee (allowing the distal femur and 15 cm of the proximal tibia to be captured), and one centered over the ankle. The slice thickness was 0.625 mm for the knee and 2 mm for the hip and ankle (GE Light Speed VCT 64).
An OW-HTO model was used to virtually position the Activmotion HTO plate (Newclip Technics®, Haute-Goulaine, France) on the tibia following the manufacturer’s recommendations for “ideal” positioning. The PSCG design takes into account the resection plane and the position of the screw tunnels relative to the virtual positioning of the plate. The objective behind the PSCG is to define the optimal plate position after tibial osteotomy correction, and then to report this anatomical position to the pre-osteotomy guide position. When the plate’s position fits the drill holes using the PSCG, the osteotomy is created, and subsequent opening wedge of the tibia allows optimal correction of the MPTA and PPTA.
The PSCG was secured to the bone with two pins, and then fluoroscopy was used to confirm the orientation of the osteotomy cut. The eight holes needed for the plate were pre-drilled prior to performing the osteotomy. The osteotomy was then performed with the PSCG in place. The saw blade was guided by a specific slotted capture of the PSCG, after which the proximal portion of the modular cutting guide was removed to finish the osteotomy in a single plane or two planes. This step was dependent on the planned correction and the position of the patellar tendon.
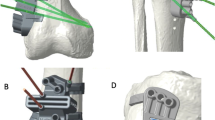
The osteotomy was then gradually opened/distracted with a lamina-spreader until the pre-drilled screw holes were aligned with the holes in the plate. The plate was secured using eight screws, the sizes of which were pre-determined during the pre-operative planning (Fig. 1a–f). The bone defect was left empty or filled with a femoral head wedge allograft or injectable phosphocalcic cement (QuickSet, Graftys®, Aix-en-Provence, France).
Pre-operative 3D templating illustrating the operative technique of patient-specific cutting guides. a, b Optimal positioning of the cutting guide with two pins (one to protect the lateral hinge during the osteotomy and one to guide the saw). c Pre-drilling the 8 holes of the plate with the guide. d Illustration of lateral hinge protection by pin. e, f Opening of the osteotomy with definitive positioning of the plate and screws on the pre-drilled holes
Grafted material was decided upon the surgeon’s preference. Post-operative management included partial to full-weight bearing as tolerated at day 1 aided if needed with the use of crutches.
All patients were reviewed one month post operatively to evaluate potential early complications and to undergo a CT scan in order to evaluate the accuracy of post-operative alignment and hinge evaluation (fractures were classified according to Takeuchi [12]. The patients were then re-reviewed every three months for regular follow-up with radiographs (long-leg standing, A/P, and lateral). Bone union and hinge stability were systematically assessed.
Patients were reviewed at one, three, 12, 18, and 24 months then every year to ensure there were no delayed complications.
At each appointment, an independent observer assessed the following:
Accuracy of the correction (post-operative alignment) is defined as the difference between the desired correction (defined pre-operatively) and the correction obtained post-operatively measured on CT scan (ΔHKA, ΔMPTA, ΔPPTA) at one month.
KOOS scoring system [13] and the UCLA activity scale [14] were recorded before the surgery and at one and two years.
Changes in the KOOS sub-scores were estimated comparing pre-operative to final follow-up assessment: ΔKOOS Pain, ΔKOOS Symptoms, ΔKOOS ADL, ΔKOOS Sport/Rec, and ΔKOOS QOL were defined this way.
The UCLA activity scale evaluates the patient physical activity. The scale has ten descriptive activity levels ranging from wholly inactive and dependent on others (level 1) to regular participation in impact sports such as running, skiing, or playing tennis (level 10).
UCLA scores were recorded both pre-operatively (Po) and before the onset of symptoms (BS) as estimated by patients. Subsequently, two values compared to their last follow-up assessment of sport activities, ΔUCLA-Po and ΔUCLA-BS, were defined this way.
To estimate socio-professional improvement, ability to return to work and sport were also recorded.
Intra-operative and post-operative complications were recorded with a specific focus on the number of cases in which the PSCG procedure was abandoned, difficulties with wound and bone healing, hinge fracture, delayed or absent graft integration, and the number of cases requiring hardware removal (Fig. 2).
Intra-operative pictures of a 54-year-old patient undergoing HTO using a PSCG. a–c The PSCG is secured onto the tibia; two k-wires help to guide the saw blade and to protect the lateral hinge. d A wedge is sculpted in a femoral head allograft. e, f Final plate and screws’ positions verified on a fluoroscopic image
Population
One hundred patients (59 men and 41 women) were included; no patients were lost to follow-up at a mean of two years. The mean patient age was 44.2 ± 6.8. Pre-operatively, the mean HKA angle was 171.6 ± 2.8°, the mean MPTA was 79.8 ± 3.1°, and the mean PPTA was 9.2 ± 3° (Table 1).
Statistical analysis
The descriptive statistic was present as mean ± standard deviation for quantitative variables. The Mann-Whitney U test for two independent samples with 95% confidence interval (95% CI) was used to evaluate the differences between two variables, one-way ANOVA between more than two variables, and multiple linear regressions for relationships. The paired Student t test was used to estimate evolution of functional outcomes during follow-up. The differences in proportions between two samples were estimated with the z test with 95% CI. Finally, a multivariate analysis evaluating factors related to accuracy, clinical outcomes, and complications rate was performed.
Results
Accuracy of post-operative alignment (Tables 2 and 3)
The mean ΔHKA was 1 ± 0.9°, the mean ΔMPTA was 0.5 ± 0.6°, and the mean ΔPPTA was 0.4 ± 0.8°. No significant differences (all p values > 0.05) were observed between the desired correction defined pre-operatively and the correction obtained post-operatively (ΔHKA, ΔMPTA, ΔPPTA). Inter-observer correlation coefficients (CCIs) were found to be 0.67, 0.88, and 0.89 regarding the capability of the PSI system to reproduce planned correction for HKA, gender, age, physical lifestyle at work (sedentary vs active), HKA pre-op, MPTA pre-op, PPTA pre-op, and graft material which did not correlate with significant accuracy differences in both univariate and multivariate analyses. A significant association was found between ΔHKA, ΔPPTA, and the occurrence of a hinge fracture (respectively p = 0.04 and p < 0.0001).
Functional outcomes (Tables 4 and 5)
At a mean of two years, an improvement of 27 ± 25 for the KOOS Pain, 28 ± 26 for the KOOS symptoms, 27 ± 28 for the KOOS ADL, 26 ± 33 for the KOOS sport/rec, 28 ± 38 for the KOOS QOL, and 1.6 ± 2.4 for the UCLA was obtained as compared to the pre-operative values (all p < 0.0001).
Gender, HKA pre-op, MPTA pre-op, PPTA pre-op, ΔHKA, ΔMPTA, and hardware removal did not correlate with significant difference in terms of functional outcomes in the univariate or multivariate analysis. A significant correlation was found between age, ΔPPTA, time to bone healing, the occurrence of a hinge fracture or post-operative complications, and KOOS sub-score improvement (all p < 0.05). The mean time to return to work and sports were 2.7 ± 2.1 and 5.4 ± 4.3 months, respectively.
Complications (Table 6)
No abandonment of the PSCG procedure was observed.
Minor complications included benign lateral hinge fractures Takeuchi type 1 (18%), postoperative haematoma (9%), graft osteolysis (2%), and persistent phosphocalcic cement graft at the last follow-up (7%). Major complications (10%) included Takeuchi type 2 and 3 fractures (6%), deep wound infections (3%), and non-union of the osteotomy (1%). Hardware removal was required (medical reason, e.g., local pain related to hardware) in three patients at the last-follow-up.
The mean time to bone healing was 4.6 ± 2.1 months.
Discussion
The main finding of this study is as follows: performing an OW-HTO with PSCG is a reliable and accurate procedure. It also allows good functional outcomes to be observed at a mean of two years without increasing the rate of specific or non-specific complications.
The first objective of this study was to analyze the reliability of this technique by comparing the accuracy of the achieved correction (measured on CT scan) relative to the planned correction (defined pre-operatively) in both the coronal and sagittal planes (HKA, MPTA, and PPTA). Importantly, varying intra-operative methods have been described to control and instrument the osteotomy; however, these techniques seem to limit the accuracy that can be obtained from osteotomy surgery and only focus on coronal plane correction. In a review of the literature by Van Den Bempt et al., they report a wide range of deviation away from the ideal coronal plane correction being attempted [15]. The mean accuracy was 5.6° (from 4° to 8°) for conventional methods, and it was 5.5° (from 4° to 7°) using the computer-assisted surgery.
Furthermore, previous series have observed a 30 to 50% accuracy of correction after conventional OW-HTO [16]. Other groups that have published work focusing on computer-assisted surgery have also failed to demonstrate optimal correction in more than 20% of their patients undergoing OW-HTO [10]. This is contrary to the results of this study, where the post-operative correction was reproducible and accurate to the pre-planned correction using PSCG technology.
The results of this study compare favorably to those of Saragaglia et al. who reported a 96% accuracy for a planned HKA angle of 184° ± 2° using computer-assisted surgery [17].
Several recent studies have published accurate and reliable corrections in OW-HTO surgery with the use of PSCG. Victor et al. [8] reported an accuracy of 1° in the coronal plane and 2° in the sagittal plane, except that the study was performed with radiographic analysis only. Perez-Mananes et al. [9] had similar results and reported an accuracy of 2° in the coronal plane; however, in their series the tibial slope was not measured and neither was CT analysis performed. Munier et al. [7] in their pilot study observed an accuracy measured on a CT scan of less than 2° in the coronal and sagittal planes. In terms of achieving an accurate correction, the results demonstrated in this study are similar to these three published series.
It is well documented that correcting the sagittal plane is essential in preserving knee biomechanics [8, 18]. An OW-HTO is known to modify the sagittal plane by increasing the tibial slope [19,20,21]. Findings of this study suggest that changes within the tibial slope (PTTA) are predictably accurate, which in turn is essential for managing cruciate ligament balance within the knee and trying to maintain the native biomechanics.
Another objective of this study was to evaluate the functional outcomes through the KOOS and UCLA activity scale, at a mean of two years of follow-up. In contrast to this study, other series using PSCG for OW-HTO demonstrate little or no clinical follow-up of patients. All sub-scores of the KOOS in this study showed an improvement of approximately 25 points between the value obtained in the pre-operative questionnaire and that obtained at the last follow-up (mean 2 years). This study was consistent and parallel with other published studies demonstrating that functional scores improved after HTO [22,23,24]. Several studies have published results on return to sports after HTO [25,26,27] and concluded that return to sports was possible at the same or a higher functioning level; the findings in this present study reinforce these conclusions (gain of 1.6 ± 2.4 for the UCLA was obtained, at a mean of 2 years). The use of PSCG for OW-HTO allows good socio-professional outcomes with early return to work and sport (2.7 ± 2.1 months and 5.4 ± 3.3 months, respectively).
The last objective was to evaluate the occurrence of specific and non-specific complications occurring in the first 100 patients treated using PSCG for OW-HTO in this series.
Several recent studies have reported that the complication rate following medial OW-HTO ranged from 1.9 to 55% [28]. The overall complication rate was 32% up to two years post-operatively, and the majority of the complications were classed as minor (28%). Major complications requiring procedure modification or additional surgery were found in 10% of patients in this series.
Recently in 2019, Han et al. [29] reported a 29.7% complication rate after medial OW-HTO using locking plates; most of their complications were minor (21.1%). The most reported complication was an un-displaced lateral hinge fracture, while major complications requiring additional surgical treatment were found in 8.6% of their treated patient population.
In this series, the incidence of lateral hinge fractures detected on CT scan was 24%. This is similar to recent reports with incidence rates ranging from 15.6 to 25.4% [28, 30].
This study bears several limitations; firstly, this is a non-comparative study and although data exists on the safety and accuracy of conventional or computer-assisted surgeries, a control group of conventional HTO would have been valuable to draw direct comparison. The early results of this study and experience with PSCG have made the authors stop and transition from the use of conventional HTO procedure completely.
Secondly, OW-HTO using PSCG requires a pre-operative CT scan, which subsequently increases the radiation exposure and is not necessary in conventional or computer-assisted surgeries. Nevertheless, Perez-Mananes et al. [9] published that PSCG reduced the use of intraoperative fluoroscopy (average of 55 in conventional procedure) and required less surgical time. Moreover, CT scanning and 3D modeling have shown to have a number of advantages over using standard radiographs; it improves the visualization and thus understanding of the procedure, defines the required correction during pre-operative planning, and importantly improves the reliability of measuring the post-operative correction to the pre-operative planned correction and any potential complication such as hinge fractures [31, 32].
Thirdly, the mean follow-up time was two years following surgery, which may be sufficient to assess the complication rate. However, longer follow-up will be necessary to estimate clinical benefits and TKA-free survivorship.
Finally, many factors might have influenced postoperative outcomes; upon those, the type of graft used to fill the osteotomy gap seems to be detrimental. Better functional outcomes (UCLA score) were found in patients operated on using femoral head allograft, as compared to phosphocalcic cement (Table 5). Those results corroborate with recent literature in both translational [33] and clinical sciences [34] underlining the need for more research in this peculiar area.
Despite these limitations, this is the largest reported series to date (100 cases as compared to 14 [8] and 8 for [9]). The use of PSCG in OW-HTO surgery was observed to be safe and accurate, and allows significant improvement in commonly used functional outcome scores two years after the procedure.
Conclusion
In the largest series to date, PSCG technology used for OW-HTO was safe and allows accurate achievement of the desired correction in the coronal and sagittal planes without increasing the rate of specific or non-specific complications.
PSCG and OW-HTO provide satisfactory and favourable functional outcomes at two years of follow-up.
References
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 21:197–205. https://doi.org/10.1007/s00167-012-2122-3
Bode G, von Heyden J, Pestka J et al (2015) Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 23:1949–1955. https://doi.org/10.1007/s00167-013-2762-y
Ferner F, Lutter C, Dickschas J, Strecker W (2019) Medial open wedge vs. lateral closed wedge high tibial osteotomy - indications based on the findings of patellar height, leg length, torsional correction and clinical outcome in one hundred cases. Int Orthop 43:1379–1386. https://doi.org/10.1007/s00264-018-4155-9
Saragaglia D, Chedal-Bornu B, Rouchy RC et al (2016) Role of computer-assisted surgery in osteotomies around the knee. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3387–3395. https://doi.org/10.1007/s00167-016-4302-z
Elson DW, Petheram TG, Dawson MJ (2015) High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci’s method. Knee Surg Sports Traumatol Arthrosc 23:2041–2048. https://doi.org/10.1007/s00167-014-2920-x
Nicolau X, Bonnomet F, Favreau H et al (2018) Précision de la correction dans les ostéotomies tibiales proximales de valgisation par ouverture médiale : comparaison entre table de Hernigou et méthode classique. Rev Chir Orthopédique Traumatol 104:S101. https://doi.org/10.1016/j.rcot.2018.09.095
Munier M, Donnez M, Ollivier M et al (2017) Can three-dimensional patient-specific cutting guides be used to achieve optimal correction for high tibial osteotomy? Pilot study. Orthop Traumatol Surg Res OTSR 103:245–250. https://doi.org/10.1016/j.otsr.2016.11.020
Victor J, Premanathan A (2013) Virtual 3D planning and patient specific surgical guides for osteotomies around the knee: a feasibility and proof-of-concept study. Bone Jt J 95–B:153–158. https://doi.org/10.1302/0301-620X.95B11.32950
Pérez-Mañanes R, Burró JA, Manaute JR et al (2016) 3D surgical printing cutting guides for open-wedge high tibial osteotomy: do it yourself. J Knee Surg 29:690–695. https://doi.org/10.1055/s-0036-1572412
Donnez M, Ollivier M, Munier M et al (2018) Are three-dimensional patient-specific cutting guides for open wedge high tibial osteotomy accurate? An in vitro study. J Orthop Surg 13. https://doi.org/10.1186/s13018-018-0872-4
Ahlbäck S (2096) Rydberg J (1980) [X-ray classification and examination technics in gonarthrosis]. Lakartidningen 77:2091–2093
Nakamura R, Komatsu N, Murao T et al (2015) The validity of the classification for lateral hinge fractures in open wedge high tibial osteotomy. Bone Jt J 97–B:1226–1231. https://doi.org/10.1302/0301-620X.97B9.34949
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64. https://doi.org/10.1186/1477-7525-1-64
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplast 13:890–895
Van den Bempt M, Van Genechten W, Claes T, Claes S (2016) How accurately does high tibial osteotomy correct the mechanical axis of an arthritic varus knee? A systematic review. Knee 23:925–935. https://doi.org/10.1016/j.knee.2016.10.001
Marti CB, Gautier E, Wachtl SW, Jakob RP (2004) Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthrosc J Arthrosc Relat Surg 20:366–372. https://doi.org/10.1016/j.arthro.2004.01.024
Saragaglia D, Roberts J (2005) Navigated osteotomies around the knee in 170 patients with osteoarthritis secondary to genu varum. Orthopedics 28:s1269–s1274
Martineau PA, Fening SD, Miniaci A (2010) Anterior opening wedge high tibial osteotomy: the effect of increasing posterior tibial slope on ligament strain. Can J Surg J Can Chir 53:261–267
Nerhus TK, Ekeland A, Solberg G et al (2017) Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 25:910–917. https://doi.org/10.1007/s00167-015-3817-z
Ducat A, Sariali E, Lebel B et al (2012) Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res OTSR 98:68–74. https://doi.org/10.1016/j.otsr.2011.08.013
Tseng T-H, Tsai Y-C, Lin K-Y et al (2019) The correlation of sagittal osteotomy inclination and the anteroposterior translation in medial open-wedge high tibial osteotomy-one of the causes affecting the patellofemoral joint? Int Orthop 43:605–610. https://doi.org/10.1007/s00264-018-3951-6
Saragaglia D, Blaysat M, Inman D, Mercier N (2011) Outcome of opening wedge high tibial osteotomy augmented with a Biosorb® wedge and fixed with a plate and screws in 124 patients with a mean of ten years follow-up. Int Orthop 35:1151–1156. https://doi.org/10.1007/s00264-010-1102-9
Schröter S, Ihle C, Elson DW et al (2016) Surgical accuracy in high tibial osteotomy: coronal equivalence of computer navigation and gap measurement. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3410–3417. https://doi.org/10.1007/s00167-016-3983-7
Han S-B, Lee J-H, Kim S-G et al (2018) Patient-reported outcomes correlate with functional scores after opening-wedge high tibial osteotomy: a clinical study. Int Orthop 42:1067–1074. https://doi.org/10.1007/s00264-017-3614-z
Ekhtiari S, Haldane CE, de Sa D et al (2016) Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am 98:1568–1577. https://doi.org/10.2106/JBJS.16.00036
Bastard C, Mirouse G, Potage D et al (2017) Return to sports and quality of life after high tibial osteotomy in patients under 60 years of age. Orthop Traumatol Surg Res OTSR 103:1189–1191. https://doi.org/10.1016/j.otsr.2017.08.013
Kim MS, Koh IJ, Sohn S et al (2018) Unicompartmental knee arthroplasty is superior to high tibial osteotomy in post-operative recovery and participation in recreational and sports activities. Int Orthop. https://doi.org/10.1007/s00264-018-4272-5
Seo S-S, Kim O-G, Seo J-H et al (2016) Complications and short-term outcomes of medial opening wedge high tibial osteotomy using a locking plate for medial osteoarthritis of the knee. Knee Surg Relat Res 28:289–296. https://doi.org/10.5792/ksrr.16.028
Han S-B, In Y, Oh KJ et al (2019) Complications associated with medial opening-wedge high tibial osteotomy using a locking plate: a multicenter study. J Arthroplast 34:439–445. https://doi.org/10.1016/j.arth.2018.11.009
Nelissen EM, van Langelaan EJ, Nelissen RGHH (2010) Stability of medial opening wedge high tibial osteotomy: a failure analysis. Int Orthop 34:217–223. https://doi.org/10.1007/s00264-009-0723-3
Boonen B, Kerens B, Schotanus MGM et al (2016) Inter-observer reliability of measurements performed on digital long-leg standing radiographs and assessment of validity compared to 3D CT-scan. Knee 23:20–24. https://doi.org/10.1016/j.knee.2015.08.008
Chernchujit B, Tharakulphan S, Prasetia R et al (2019) Preoperative planning of medial opening wedge high tibial osteotomy using 3D computer-aided design weight-bearing simulated guidance: technique and preliminary result. J Orthop Surg Hong Kong 27:2309499019831455. https://doi.org/10.1177/2309499019831455
Belsey J, Diffo Kaze A, Jobson S et al (2019) The biomechanical effects of allograft wedges used for large corrections during medial opening wedge high tibial osteotomy. PLoS One 14:e0216660. https://doi.org/10.1371/journal.pone.0216660
Slevin O, Ayeni OR, Hinterwimmer S et al (2016) The role of bone void fillers in medial opening wedge high tibial osteotomy: a systematic review. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3584–3598. https://doi.org/10.1007/s00167-016-4297-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Patient consent was collected pre-operatively after they were informed of the procedure in accordance with the principles of the Helsinki declaration. A local ethics committee approved our study protocol prior to the investigation.
Conflict of interest
Matthieu Ollivier is an educational consultant for New-Clip, Stryker, and Arthrex.
Sebastien Parratte is an educational consultant for New-Clip, Zimmer, and Arthrex.
Jean-Noël Argenson receives royalties from Zimmer.
Samir Chaouche, Maxime Fabre, Akash Sharma, and Christophe Jacquet have nothing to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was performed at the Institute for Locomotion, Aix-Marseille University, Marseille, France.
Rights and permissions
About this article
Cite this article
Chaouche, S., Jacquet, C., Fabre-Aubrespy, M. et al. Patient-specific cutting guides for open-wedge high tibial osteotomy: safety and accuracy analysis of a hundred patients continuous cohort. International Orthopaedics (SICOT) 43, 2757–2765 (2019). https://doi.org/10.1007/s00264-019-04372-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04372-4