Abstract
Purpose
This retrospective cohort study aims to evaluate the effects of introducing the O-arm-based navigation technique into the traditional posterior lumbar interbody fusion (PLIF) procedure treating elderly patients with three-level lumbar degenerative diseases.
Methods
Forty-one consecutive elderly patients were enrolled according to the criteria. There were 21 patients in the free-hand group and 20 patients in the O-arm group. Both two groups underwent the PLIF with or without the O-arm-based navigation technique. The demographic features, clinical data and outcomes, and radiological information were collected for further analysis.
Results
The average follow-up time was 18.3 (range, 12–28) months in the free-hand group and 16.7 (range, 12–24) months in the O-arm group. Comparison between two groups revealed no significant difference regarding demographic features. The operation time took in the navigation group was significantly less than that in the free-hand group (222.55 ± 38.00 mins versus 255.19 ± 40.26 mins, P < 0.05). Both VAS and ODI were improved post-operatively in two groups while comparison between groups showed no difference. The accuracy rate of pedicle screw positioning was 88.7% in the free-hand group to 96.9% in the O-arm group (P < 0.05).
Conclusion
The O-arm-based navigation is an efficacious auxiliary technique which could significantly improve the accuracy of pedicle screw insertion, especially in cases of patients with complex anatomic degenerative diseases, without sacrificing the feasibility and reliable outcome of traditional PLIF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar degenerative disease mainly consists of lumbar disc herniation, lumbar stenosis, and spondylolisthesis and has a high prevalence in the working years. Since Cloward et al. first introduced the posterior lumbar interbody fusion (PLIF) in 1953 [1], it has become one of the most recommended methods once such patients reach the indications to perform the surgery. Transpedicular screw fixation has been proved to have an advantage over other forms of spinal instrumentation and effective fusion between vertebrae ensures the maintenance of lumbar stability [2, 3]. As a well-accepted and classic surgical procedure, PLIF still has a broad indication compared to modified approach or minimally invasive surgeries, especially for treating multilevel lumbar degenerative disease.
However, PLIF continues to have a high complication rate (dural tear, 5.4 to 10%; neurologic injury, 9 to 16%) [4] and malposition of the pedicle screws could significantly contribute to severe complications. Penetration on the sagittal plane may cause neural root stimulation and injury while severe medial penetration could cause a dural tear or spine injury. Also, overlong screws may breach the vertebral anterior edge and bleeding could occur once screws pierce the presacral vessels. Further, the surgery performed on elderly patients was proved to be challenging, for the anatomic bony structures were usually imprecise. As a result, the surgical technique for PLIF continues to be modified and refined. Besides the use of supplemental posterolateral bone grafting and engineered interbody devices to add spine stability, the employment of equipment that improving pedicle screw instrumentation accuracy extremely promotes the outcome of patients undergoing the surgery. There have been various techniques fulfilling the demands of screw positioning navigation. Among these clinically used image-assisted systems, the O-arm-based navigation has high precision robotics for real-time and preset positioning and could obtain both 2D or 3D images intra-operatively, which shows great advantages over other devices. This retrospective study aims to research on the effects of the O-arm-based navigation applied in the conventional PLIF procedure treating elderly patients with three-level lumbar degenerative diseases.
Materials and methods
Patients
From January 2014 to June 2016, the database of patients who admitted to the spinal department of our hospital for surgical treatment were screened with criteria as follows. The including criteria were (1) all patients were operated upon by the same surgical team; (2) patients presented low back pain with or not radiation pain to the lower extremities, intermittent claudication, and neurological symptoms; (3) radiological examination revealed lumbar disc herniation, spinal stenosis, degenerative spondylolisthesis or instability, and other degenerative changes in three consecutive segments; (4) patients underwent at least three months of regular conservative therapy with an unsatisfactory outcome; (5) patients were at least 65 years old; and (6) at least one segment was performed fusion. The exclusive criteria were (1) patients had previous history of lumbar surgery; (2) adjacent tumours, active tuberculosis or other infections, fractures, or other traumas were found; (3) patients had arthritis deformans; (4) isthmic spondylolisthesis; and (5) patients with severe osteoporosis and/or internal medical diseases were unsuitable for surgery.
Forty-one patients were eligible in this cohort study ultimately. Of all the patients enrolled in this study, 21 patients underwent conventional open PLIF while the remaining 20 patients underwent open PLIF under the O-arm-based navigation. All the patients were free to choose the surgical procedure when surgeon explicated the pre-operative informed consent.
Surgical techniques
PLIF under the O-arm-based navigation
Under general anesthesia, the patient was placed in a prone position on the Jackson carbon-fibre operating table. The segments were verified before operation by palpating the spinal process, iliac crest, and other superficial bony landmarks. The dynamic reference frame was fixed on the adjacent spine process. A median incision was made according to the prepared markers and paravertebral muscles were subsequently retracted to expose the relevant bony structures. Before the screw implantation, 3D reconstructed images were obtained from intra-operative scans which was performed by the O-arm device and the data was then transferred to the StealthStation navigation system. Passive Planar Probe was utilized to preset the entry point and canal direction based on the virtual elongated navigation trajectory. Afterwards, a cannula and a high-speed drill were used to avoid deviating while creating the screw path. The pedicle hole was explored using a guided tap to eliminate any possibility of severe penetration. Appropriate screws with best length and width were inserted through the pedicle. Following the serial placement of pedicle screws, spinal process along with lamina was removed and then cut into stripes as autogenous bone graft. Also, the ligamentum flavum was detached carefully to acquire the complete decompression. A discectomy was performed and the vertebral endplates were carefully prepared. Filled with previously processed bone chips, the cage was inserted deeply into the intervertebral space. After two rods were attached connecting the adjacent pedicle screws respectively, a final scan was performed using the O-arm technique to recheck the appropriate position of implantations. These intra-operative data were all saved and transmitted to the StarPACS computerized imaging software system. The fascia, subcutaneous tissue, and skin were closed carefully.
Conventional PLIF
The conventional PLIF was performed as other literature reviewed [5]. A C-arm fluoroscopy was used for intra-operative assessment and the pedicle screw was positioned by free-hand on the basis of the Roy-Camille technique [6].
Clinical and radiological evaluation
Clinical data including operating time, intra-operative blood loss, post-operative drain, amounts of transfusion, length of stay, post-operative complications, and surgical outcomes were collected for analysis. CT scan for patients of the free-hand group was acquired before they discharged from the hospital. All the patients received favorable follow-up for at least 12 months. They were asked for making both clinical and radiological assessment at six and 12 months post-operatively and annually afterwards. The fusion status was evaluated referring to the Bridwell’s posterior fusion grades, by means of plain radiographs [7]. Intra-operative O-arm scans and post-operative CT scans were used to evaluate the position of pedicle screws, according to the classification used by the vast majority of eligible studies [8, 9]. In terms of clinical outcomes, visual analog scale (VAS) was used to quantify the back and leg pain while the daily life condition was assessed by the Oswestry Disability Index (ODI). To reduce bias, independent researchers made individual analysis in their respective works.
Statistical analysis
Statistical analyses were performed with the SPSS 19.0 software (SPSS Inc., Chicago, IL). The continuous variables were checked by Shapiro-Wilk (W test) to determine whether they are normal distribution. The Student’s t test was used to operate comparison when the data obey normal distribution, and the nonparametric rank sum test was adopted when the data was non-normal distribution. Paired t test was used to operate intra-group comparisons that the data were at different time points in the same group. The chi-square test or Fisher’s exact test were used to compare categorical variables between two groups. P < 0.05 indicated that the difference was statistically significant.
Results
Detailed characteristics of the patients were displayed in Table 1. Comparison between two groups revealed no significant difference regarding demographic features. Also, in terms of clinical assessments including intra-operative blood loss and post-operative drainage, as well as total blood transfusion, no significant difference was observed between two groups. The average operation time was 255.19 ± 40.26 min in the free-hand group and 222.55 ± 38.00 min in the O-arm group (P = 0.011, Table 2). There were four patients in the free-hand group compared to two patients in navigation group developed post-operative complications. One patient was found to have a dural tear during the surgery while another one patient developed temporary nerve root symptoms when he woke up from anesthesia in the free-hand group, and their symptoms improved before leaving the hospital. Also, there occurred two superficial infections in both two groups respectively.
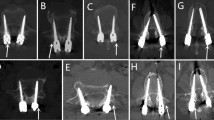
In all, 168 screws were implanted in the free-hand group and 160 screws were implanted in the O-arm group. Every segment involved received a screw insertion and no fixation failure occurred intra-operatively while, among them, two screws were revised in the free-hand group shortly after the fluoroscopy. One hundred forty-nine screws were satisfactorily remained inside the pedicle in the free-hand group in comparison to 155 screws in the O-arm group. Twelve screws versus three screws, five screws versus two screws, and two screws versus zero screws were observed penetration in two groups respectively in an ascending grade of minor (0–2 mm), moderate (2–4 mm), and severe (4–8 mm) penetration (Table 3). To add together, 19 of 168 screws were considered as malposition in the O-arm group compared to five of 160 screws in the free-hand group (Table 3). The accuracy rate of screw positioning was 88.7 to 96.9% accordingly (P < 0.05). One representative challenging case treated under the O-arm base navigation was attached as Figs. 1 and 2.
Preoperative images of an 80-year-old male patient who suffered from multilevel disc herniation accompanied with spine canal stenosis. Anteroposterior and lateral radiographs (a, b) showed slight scoliosis and narrowing of the L3–4 segment. Sagittal scan (c) demonstrated the severe sclerosis, and MR (d, e) revealed the severe spine canal stenosis generated from disc herniation and hypertrophy of ligamentum flavum of L2-5 segments
The average follow-up time was 18.3 (range, 12–28) months in the free-hand group and 16.7 (range, 12–24) months in the O-arm group. The intra-group comparison revealed that VAS scores for back/leg pain and ODI were significantly improved at six and 12 months after operation. However, no significant differences were observed between two groups either pre-operatively or during the follow-up. The fusion rate was 89.7% (35/39) in the free-hand group and 92.5% (37/40) in the O-arm group (Table 3) by checking the plain radiographs at end of the follow-up (P > 0.05). No cage was found displaced throughout the follow-up (Fig. 2).
Discussion
Multilevel degenerative lumbar spine disease is the common cause of lumbar and leg pain in elderly patients which severely affect the quality of life of patients. It is characterized by severe degeneration, and often combined with degenerative scoliosis, spinal stenosis, and spondylolisthesis, and accordingly, the treatment is challenging. PLIF has been a classical surgical procedure for decades and still been used worldwide in the treatment for elder patients with multilevel lumbar degenerative diseases. In order to overcome the difficulty of pedicle screw implantation, plenty methods have been introduced in clinical, such as repeated fluoroscopy during operation, pre-operative 3-D printing technique, navigation-assisted surgery, and robot-guided surgery [10, 11]; however, the optimal method remains controversial. As a result, in this article, we integrate the navigation technique with the conventional PLIF. It is notable that the latest studies have already acquired an exhaustive comprehension on the great importance of the different guidance methods on lumbar surgery, and the superiority of navigation via O-arm device has already reached broad consensus [12, 13]. To the best of our knowledge, few clinical studies have been published regarding the difference between the clinical outcomes and radiological assessments between conventional PLIF and PLIF under navigation in elder patients suffered from multi-segment lumbar degenerative diseases.
In this study, the O-arm group was found take visibly less surgical time in comparison to the free-hand group. Operation time is one of the pivotal causes which have been proved to have strong relations with the prognosis of patients [14]. Elderly people are considered to have less compensatory capacity for the post-operative recovery so that reduction in operative time may save a critical situation to a great extent. For all the surgery was performed by the same surgical team and there was no obvious difference between groups until the screws insertion, we supposed that the radiology-associated activities play the major role in the operation time. We have estimated the frequency and time for intra-operative assessment usage and found that the O-arm scan took less time in total compared to the C-arm radiography, as the scan based on O-arm device needs only one shot for succeeding activities while the C-arm has to repeatedly change its location and arm position to cater for the proper angle of filming. This advantage may not be noticed in just single-level operation but to be amplified when performing multilevel screw placement. It is worth mentioning that, though as a better technique than the 3D fluoroscope-based navigation, the O-arm-based navigation still needs time for peri-operative preparation including interface between O-arm and navigation system, date transmission, date reconstruction, and processing. Nonetheless, more valuable time could be saved once we master this technology.
Accuracy of the pedicle screw placement was evaluated by post-operative CT scans in the free-hand group and O-arm films in navigation group. The accuracy rate was 88.7 to 96.9% respectively, indicating that application of the O-arm-based navigation device could further evolve the craft of screw insertion. The accuracy rates that antedate this study range from 69 to 94% in the free-hand group while the O-arm-based navigation group reported an accuracy rate from 91.9 to 99% [15,16,17,18], which is in conformity with our results. Unfortunately, despite great caution, two patients in the free-hand group still developed relatively severe complications. Both of them had trouble with screw positioning. By rechecking the pre-operative CT of them referring to the classification regarding the grading of facet joint degeneration [19] and degenerative scoliosis [20], we discovered that both the two patients had severe degeneration that one’s facet joint reached grade 4 by criteria of Pathria on CT while the other had scoliosis along with a grade 3 facet joint degeneration. It is worth mentioning that either advanced age or long-level degeneration could significantly contribute to the secondary local anatomic changes, for instance, excessive thickness of the facet joint, osteophyte generation, and degeneration combined with slight acquired deformity. Such cumbersome alterations may partly conceal the necessary landmarks while surgeons perform PLIF referring to the classical principles. Comparatively, by resorting to the navigation technique, working canal through the pedicle may become directly visible so that subsequent adjustment could be maneuvered in advance to ameliorate the screw positioning despite the superficial osseous hyperplasia.
The intra-operative blood loss, transfusion volume, postoperative drainage volume, and duration of hospital stay in the O-arm group were all slightly less than those in the free-hand group. However, the difference between two groups was not statistically significant. This seems to be a weak point compared to minimally invasive surgeries in treating single segment lesions due to the open procedure [21]. Yet, in multi-segmental degenerative diseases with complex anatomies, an open incision is still recommended to guarantee the absolute safety of the surgery. As for clinical outcomes and post-operative complications, though two relatively troublesome morbidities occurred as mentioned above, combined analysis revealed no significant difference between two groups, which means both two procedures ensure the remarkable effect of surgery.
The radiation exposure to medical staff is always an inevitable issue while orthopaedic surgeons perform internal implant placement. Mroz et al. reported that radiation exposure was associated with potential morbidity like cataract formation, skin erythema, or malignancies [22]. As all the staff would leave operation room in advance, the hazard could be deemed as nearly zero level.
Although navigation brings great benefits, it may significantly prolong the operation time when surgeons initiate this novel technique despite its merit of reducing the learning curve of junior doctors. Consequently, essential practices are recommended before carrying out this technology, especially in the extreme case of advanced age. It is also a pity that surgery via open incisions could reduce neither the blood loss, nor the duration of hospital stay, which deviates the principle of fast recovery. As to the study design, this article failed to gather more cases and almost all the patients were indigenous residents.
Conclusions
Open PLIF under navigation based on the O-arm device is an efficacious, safe modification of the traditional PLIF. The accuracy of pedicle screw positioning assisted by the O-arm-based navigation is superior to the free-hand group. Besides, the operation time is significantly shortened and still has great potential to make progress. Meanwhile, it maintains a guaranteed clinical outcome but does not sacrifice the merits of primary surgery. To sum up, we deem that surgery under navigation based on the O-arm device deserves to be promoted as a routine surgical procedure treating elderly patients with three-level degeneration diseases.
References
Cloward RB (1953) The treatment of ruptured lumbar intervertebral discs by vertebral body fusion: I Indications, operative technique, after care. J Neurosurg 10:154–168
Rafi S, Munshi N, Abbas A, Shaikh RH, Hashmi I (2016) Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. J Neurosci Rural Pract 7:550–553
Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K (2004) Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2040–2048
DiPaola CP, Molinari RW (2008) Posterior lumbar interbody fusion. J Am Acad Orthop Surg 16:130–139
Mehdian H, Kothari M (2017) PLIF and modified TLIF using the PLIF approach. Eur Spine J 26:420–422
Roy-Camille R, Saillant G, Mazel C (1986) Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res 203:7–17
Bridwell KH, Lenke LG, McEnery KW, McEnery KW, Baldus C, Blanke K (1995) Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 20:1410–1418
Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 9:235–240
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15:11–14
Zhang Y, Wen L, Zhang J, Yan G, Zhou Y, Huang B (2017) Three-dimensional printing and computer navigation assisted hemipelvectomy for en bloc resection of osteochondroma: a case report. Medicine (Baltimore) 96:e6414
Schatlo B, Molliqaj G, Cuvinciuc V, Kotowski M, Schaller K, Tessitore E (2014) Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine 20:636–643
Gonschorek O, Hauck S, Spiegl U, Weiß T, Pätzold R, Bühren V (2011) O-arm(®)-based spinal navigation and intraoperative 3D-imaging: first experiences. Eur J Trauma Emerg Surg 37:99–108
Holly LT, Foley KT (2007) Image guidance in spine surgery. Orthop Clin N Am 38:451–461 abstract viii
Kim BD, Hsu WK, De Oliveira GS, Saha S, Kim JY (2014) Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (Phila Pa 1976) 39:510–520
Shin MH, Hur JW, Ryu KS, Park CK (2015) Prospective comparison study between the fluoroscopy-guided and navigation coupled with O-arm-guided pedicle screw placement in the thoracic and lumbosacral spines. J Spinal Disord Tech 28:E347–E351
Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, Gutberlet M (2011) Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: comparison between free-hand and O-arm based navigation techniques. Eur Spine J 20:875–881
Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21:247–255
Lekovic GP, Potts EA, Karahalios DG, Hall G (2007) A comparison of two techniques in image-guided thoracic pedicle screw placement: a retrospective study of 37 patients and 277 pedicle screws. J Neurosurg Spine 7:393–398
Zhou X, Liu Y, Zhou S, Fu XX, Yu XL, Fu CL, Zhang B, Dai M (2016) The correlation between radiographic and pathologic grading of lumbar facet joint degeneration. BMC Med Imaging 16:27
Yang C, Yang M, Chen Y, Wei X, Ni H, Chen Z, Li J, Bai Y, Zhu X, Li M (2015) Radiographic parameters in adult degenerative scoliosis and different parameters between sagittal balanced and imbalanced ADS patients. Medicine (Baltimore) 94:e1198
Jin-Tao Q, Yu T, Mei W, Xu-Dong T, Tian-Jian Z, Guo-Hua S, Lei C, Yue H, Zi-Tian W, Yue Z (2015) Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 24:1058–1065
Mroz TE, Abdullah KG, Steinmetz MP, Klineberg EO, Lieberman IH (2011) Radiation exposure to the surgeon during percutaneous pedicle screw placement. J Spinal Disord Tech 24:264–267
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Yucheng Wang and Kangwu Chen and equal contributors.
Rights and permissions
About this article
Cite this article
Wang, Y., Chen, K., Chen, H. et al. Comparison between free-hand and O-arm-based navigated posterior lumbar interbody fusion in elderly cohorts with three-level lumbar degenerative disease. International Orthopaedics (SICOT) 43, 351–357 (2019). https://doi.org/10.1007/s00264-018-4005-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4005-9