Abstract
Purpose
We hypothesized that osteoarthritis developing after instability surgery is radiographically similar to primary arthritis and that arthroplasty provides comparable outcomes in patients with these two types of osteoarthritis.
Methods
Patients with osteoarthritis due to instability surgery (group I) and with primary osteoarthritis (group II) were included. Mean follow-up was 52.6 and 41.6 months, respectively. Hemiarthroplasties (HA) were 32% in group I and 27% in group II; total shoulder arthroplasties (TSA) were 68 and 73% respectively. Outcome measures included active shoulder mobility (anterior elevation [AAE], lateral elevation [ALE], external rotation [ER], and internal rotation [IR]), pain, Constant-Murley score, and Simple Shoulder Test. Pre-operative and post-operative radiographs were taken. Glenoid arthritis was assessed by computed tomography.
Results
Participants were 19 in the group I (mean age 44.5 years, 12 males, 7 females) and 30 in the group II (mean age 48.2 years, 28 males, 12 females). Both patient groups had pre-operative concentric arthritis. Group II had higher rates of A2 and B1 glenoids (p = 0.003). A longer interval from stabilization to replacement was associated with lower post-operative IR (p = 0.017) and ALE (p = 0.035). Post-operative ER and IR were higher in group I (p < 0.001 and p = 0.001, respectively). In group I, AFE and ALE were higher in HA than TSA patients (both p = 0.009). The CS and SST score increased significantly in both groups (both p < 0.001). Group II showed significantly greater humeral radiolucency (p = 0.025) and a higher rate of TSA revision to reverse prostheses compared with group I.
Conclusions
Shoulder replacement provides similar clinical and radiographic outcomes in arthritis secondary to instability surgery and in primary osteoarthritis. Posterior glenoid wear is more common in primary osteoarthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical procedures performed to treat anterior glenohumeral instability and glenoid deficiency have proved capable of restoring shoulder function with low recurrence rates and good clinical outcomes [1,2,3]. Nevertheless, osteoarthritis, a recognized long-term complication after instability surgery, has adverse clinical and histopathological effects [4,5,6,7,8] that have been reported in 12 to 60% of cases [9,10,11,12]. The fact that most of these patients are young and active individuals with high functional demands compounds the problem.
The most common arthrogenic factors include excessive anterior soft tissue tightening, especially due to anterior fixation of the subscapularis to the glenoid (Putti-Platt procedure) [5, 6, 13,14,15], lateral graft overhanging after bone-block procedures [16], and intra-articular hardware prominence [17, 18]. According to a recent clinical investigation, the number of anchors and the state of the labrum are the main factors associated with a higher risk of radiographic degenerative changes after arthroscopic anterior Bankart repair [19]. Matsen et al. have coined the phrase “capsulorrhaphy arthropathy” to describe arthritis arising as a consequence of overly tightened soft tissues [20]. Three studies of anatomical shoulder replacement, including hemiarthroplasty (HA) and total shoulder arthroplasty (TSA), in patients with osteoarthritis arising after instability surgery have reported good mid-term clinical outcomes in terms of pain relief and mobility [5, 7, 21]; notably, Sperling et al. [21] have found a non-negligible revision rate and unsatisfactory results due to component failure, instability, and painful glenoid arthritis. The radiographic patterns of shoulder osteoarthritis described in these studies share several similarities with those of primary arthritis, but the glenoid type was not reported.
In this study, we tested the hypothesis that patients treated with shoulder replacement for arthritis due to instability surgery have a similar pre-operative pattern of osteoarthritis as those treated for primary osteoarthritis and share similar post-operative clinical and radiographic outcomes.
Materials and methods
This was a retrospective analysis of prospective data collected from January 2011 (when computer records became available at our hospital) to February 2016. The charts of 210 patients who received HA and TSA were retrospectively reviewed to identify cases with a pre-operative diagnosis of osteoarthritis due to glenohumeral stabilization (“osteoarthritis stabilization,” group I). Patients who received HA or TSA for primary osteoarthritis were the control group (“primary osteoarthritis,” group II). The study was performed at the Shoulder and Elbow Unit of “Cervesi” Hospital, Cattolica (Italy) and was approved by the institutional review board as part of a larger Shoulder Arthroplasty investigation (prot. no. 2964/20141.5/20 CEAV/IRST Meldola, Italy). Patients with a preoperative diagnosis of shoulder arthritis following surgical stabilization or primary osteoarthritis and a minimum follow-up of 24 months were included. Prior shoulder stabilization procedures were performed using (i) a metal staple (Putti-Platt procedure) in five patients, (ii) glenoid bone sutures or two metallic anchors in open capsulorraphy patients, (iii) anchors (metallic in three and resorbable in two) in arthroscopic capsulorraphy patients. One patient had a Latarjet procedure with one anchor prominent on the glenoid surface. Glenoid replacement was based on the pre-operative status of glenoid arthritis (only A1 glenoids received HA). There were no other specific exclusion criteria. Patients who lived more than 600 km from the hospital declined to participate and eight had incomplete radiographic follow-up data, leaving 49 patients (49 shoulders), 19 in group I and 30 in group II. Procedures in group I included 13 TSAs (4 standard stems with a metal back [MB] glenoid and 9 short stems with a polyethylene [PE] glenoid), two short-stem HAs, and four humeral head resurfacing (HHR) procedures (1 using a pyrocarbon head). Procedures in group II included 22 TSAs (6 standard stems/MB glenoid and 16 short stems/PE glenoid), five short-stem HAs, and three HHR procedures. Pyrocarbon humeral head was used in HAs of both groups. Participants’ demographics and peri-operative data are reported in Table 1.
Pre-operative imaging
Pre-operative imaging included plain radiographs in anteroposterior (AP) Grashey, Y lateral, and axillary views and computed tomography (CT) scans.
Arthritis severity was graded according to Samilson-Prieto [22] as modified by Gerber et al. [23]. Glenoid morphology was graded according to Bercik et al. [24] (Fig. 1). These data are reported in Table 1.
Implant design
For short-stem TSA and stemmed HA, we used the non-constrained Ascend™ prosthesis (Wright Medical, Memphis, TN, USA). Standard-stem TSA patients received the SMR™ system with the curved MB glenoid (LIMA Corporate, San Daniele del Friuli, Italy). HHR included two Copeland Mark II™ (Biomet, Swindon, UK) and four SMR-R devices (LIMA Corporate); the pyrocarbon head (PyroTITAN™, Ascension Orthopedics, Austin, TX, USA) was required in a patient with multiple metal allergies. The Copeland Mark II™ and LIMA SMR-R implants were provided with a cobalt-chrome humeral head and hydroxyapatite sprayed undersurface coating. All implants were press-fitted.
Clinical evaluation and outcome measures
Clinical status, active range of motion (ROM), pain (with a visual analog scale, VAS), and the Constant-Murley score (CS) [25] were assessed before arthroplasty and at the last follow-up visits. Active ROM was assessed in terms of forward elevation (AFE), lateral elevation (ALE), external rotation (ER; with the patient standing) using a goniometer, and internal rotation (IR; the ability to reach different levels of the spine with the thumb). Pain was graded from 0 to 10, where 0 was no pain. The ROM and clinical scores were calculated by an examiner who did participate in the surgical procedures.
Operative technique
Stemmed arthroplasty
The shoulder was exposed using a deltopectoral approach and lesser tuberosity osteotomy in continuity with the subscapularis tendon. Glenoid was replaced with a PE component fixed using low-viscosity cement (Cemex® System, Tecres S.p.A, Sommacampagna, Italy) for the peripheral pegs and finely morselized bone around the fins, to enhance bone ingrowth, for the central peg. In MB glenoids, the implant was pushed into the central hole so that its major axis coincided with major glenoid axis; after inserting the screws, at a 30° angle, the PE liner was pushed in with the thumb.
As regards the Ascend™ short-stem component, the metaphysis was prepared with rasps of increasing size, carefully preserving and gently packing the cancellous bone. For the standard stem, the canal was bored using a hand drill, then the stem and humeral body of the SMR humeral component were assembled and fixed. The definitive press-fit humeral component in titanium alloy and the pyrocarbon humeral head were impacted. Extensive anterior capsular release was performed in all cases; the subscapularis was reattached with a bone suture medial to its lateral insertion on the lesser tuberosity, to achieve tendon lengthening in patients with IR contracture (≤ 20° of ER with the arm at the side.
Humeral head resurfacing
The shoulder was exposed using the deltopectoral approach as described above. With the humerus dislocated, the centre of the head was found using a k wire as a guide. Humeral head shape and contour were restored by reaming with fully cannulated instruments, to achieve a close fit of the final implant. After drilling the central hole for the tapering docking peg, implant size was chosen using the trial head and the resurfacing head was fixed. To reduce lateralization stress on the rotator cuff, we used a size smaller than the native head (Fig. 2).
Anteroposterior Grashey view of the pyrocarbon resurfacing head (PyroTITAN™ Ascension Orthopedics, Austin, TX, USA). The prosthesis was a size smaller than the native head, to reduce lateralization stress on the rotator cuff. Black circle: diameter of the native head; red circle: diameter of the resurfacing prosthesis
Post-operative rehabilitation
The arm was immobilized in a sling for four to six weeks. Passive mobilization in the scapular plane was allowed from the first post-operative day; active assisted exercises, including IR and ER, were initiated at four to six weeks and strength exercises at eight weeks.
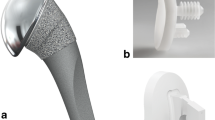
Post-operative radiographic analysis
The humeral and glenoid components were examined on standard AP and axillary radiographs using standardized criteria for short-stem and standard-stem humeral components. Glenoid wear in HAs was assessed on radiographs by measuring the glenohumeral joint space [26]. Radiological changes around the humeral component included radiolucency, condensation lines (CLs), cortical thinning (CT), spot welding (SW), subsidence and resorption of the tuberosities, and loosening [27, 28]. We assessed radiolucency in five zones of the glenoid [28] and in five and seven zones of the short-stem and standard-stem humeral components, respectively [27, 29], and graded it from 0 to 5 based on its presence and width according to Sperling et al. [29] (Fig. 3a, b). We also assessed acromiohumeral distance, subsidence, tilt, PE wear, migration, fractures, and prosthesis stability. Osteophytes were identified and heterotopic ossifications (HOs) classified from grade 1 to 4. The resurfacing prostheses were evaluated as described by Levy et al. [30] according to the criteria reported by Rispoli et al. [31] by assessing oversizing, periprosthetic radiolucency, glenohumeral subluxation, progression in glenoid erosion, and subsidence (Fig. 2).
Anteroposterior Grashey views of the two TSA designs assessed in the study. a Curved short stem with a bone-ingrowth central peg PE glenoid component (Ascend™, Wright Medical, Memphis, TN, USA). b Standard stem with an MB glenoid (SMR™, LIMA Corporate, San Daniele del Friuli, Italy). Humeral bone remodeling and radiolucency were assessed in five (short stem) and seven zones (standard straight stem). Glenoid radiolucency was assessed in five zones around the MB and PE glenoid components. M1: medial 1; M2: medial 2, L1: lateral 1, L2: lateral 2, US: under stem
Statistical analysis
Descriptive statistics (absolute and percent frequency, mean, median, standard deviation [SD], and range) for HAs and TSAs were calculated for all variables (age, gender, side, dominance, body mass index [BMI], years from stabilization to replacement, prosthetic design, and glenoid morphology). Delta scores were computed for the clinical scores as the difference between post-operative and pre-operative values. The pre-operative scores and delta scores of the two groups were compared using the Mann-Whitney test.
Relationships between each group and the qualitative baseline and post-operative variables were explored with Pearson’s χ2 test.
Significance was set at 0.05. Analyses were performed with Stata Intercooled 9.2 software for Windows.
Results
There were no differences in age, gender, BMI, or rotator cuff fatty infiltration between the groups. The rate of B1 and A2 glenoids was higher in the primary osteoarthritis group (p = 0.003). Mean follow-up duration was 52.6 months (SD, 18) in group I and 41.6 months (SD, 12) in group II (Table 1).
Clinical outcomes
The AFE, ALE, ER, and IR delta scores were significantly different in both groups (p < 0.0001). Pain decreased significantly by a median of 6 points in group I and of 7 points in group II (both p < 0.0001). The CS and Simple Shoulder Test (SST) score increased significantly in both groups (p = 0.006 and p = 0.007, respectively) (Tables 2 and 3).
In group I, a longer interval from shoulder stabilization to replacement was associated with lower IR (p = 0.017) and ALE (p = 0.035) delta scores. The stabilization procedure did not affect outcomes. ER was significantly greater in group I than group II (both post-operative values and delta scores, p = 0.0001 and p = 0.0003, respectively). Post-operative IR was also significantly greater in group I (p = 0.001), whereas the IR delta scores were not significantly different between the groups. The differences in the other planes of motion, pain, SST scores, and CS were not significant between the groups (Table 2).
Subgroup analysis showed significantly higher AFE and ALE in HAs compared with TSAs in group I (both p = 0.009) and no significant differences in the other planes of motion. Pain, CS, and SST scores were not significantly different between the two subgroups. The differences in shoulder motion and clinical scores between HAs and TSAs in group II were not significant. Moreover, there were no significant differences between these two patient subsets from each group. One SMR MB implant in group II was revised to a reverse arthroplasty after 37 months. The MB and PE glenoid components of TSA implants did not involve significantly different clinical outcomes in either group.
Radiographic outcomes
The radiographic outcomes are reported in Table 4. The only difference between the groups was a significantly higher rate of humeral radiolucency found in group II.
In group I, humeral radiolucency was found in seven (37%) shoulders, in one Ascend™ HA implant (grade 1) and six TSAs (grade 2 in one SMR™ and grade 1 in five Ascend™ implants, respectively). CL and SW were detected in four (33%) shoulders: one Ascend™ HA and three SMR™ TSA implants, respectively. CT was seen in two SMR™ TSAs (17%). Humeral radiolucency in this group was significantly associated with a lower SST score (p = 0.013). Grade 1 radiolucency was found in the pyrocarbon head. Glenoid radiolucency was depicted in five (26%) TSAs: grade 2 in one MB and grade 1 in three PE glenoids, respectively. Glenoid wear was found in five HAs (mean joint space, 1.9 mm; range, 0.9–2.1). Partial greater tuberosity resorption was observed in one Ascend™ TSA. Pre-operative and post-operative radiographs of a case of the group I underwent Ascend™ TSA are described in Fig. 4a–g.
Pre-operative and post-operative images of a shoulder where osteoarthritis developed after open anterior stabilization (group I). a Anteroposterior Grashey view showing the two metal anchors used for labral repair and the two screws implanted for coracoid bone grafting. The humeral head is subluxated inferiorly due to deltoid muscle hypotrophy and weakness. b The axillary view was poorly informative due to severe shoulder stiffness and pain. c Axial CT scan showing posterior subluxation of the arthritic humeral head and posterior glenoid erosion (B1 type glenoid). d, e Immediate post-operative (2 months) anteroposterior and axillary view of the joint with the PE glenoid component (Ascend™ Wright Medical, Memphis, TN, USA). The humeral head is well centered in the glenoid. f, g Last follow up radiographs (anteroposterior and axillary views, 61 months) of the patient whose joint is depicted in (d, e) showing a stable implant with slight humeral radiolucency (grade 1) in zones L1 and M1 and an HO below the humeral head; there were no significant changes around the PE glenoid. CT computed tomography, PE polyethylene, HO heterotopic ossification
In group II, humeral radiolucency was found in 12 (40%) shoulders: 2 Ascend™ HA (both grade 1) and 10 TSA implants (grade 1 in 6 Ascend™ and in 2 SMR™ implants; grade 2 in 2 SMR™ implants). CLs were detected in seven (36%) cases: one Ascend™ HA, five SMR™, and one Ascend™ TSA. CT was seen in three (17%) TSAs: two Ascend™ and one SMR, and SW in two Ascend™ TSAs. Partial greater tuberosity resorption was observed in three SMR™ TSAs. Glenoid radiolucency was depicted in 12 (54%) TSAs: grade 2 in 2 MB and 2 PE glenoids and grade 1 in 3 MB and 3 PE glenoids respectively. Radiolucency around the central peg of the PE component was seen in two shoulders. Glenoid wear was found in all seven HAs (mean joint space, 1.7 mm; range, 0.8–2.3). Pre-operative and post-operative radiographs of a case of the group II underwent SMR™ TSA with MB glenoid component are described in Figs. 5a–f and 6.
Pre-operative and post-operative radiographs of a patient with primary osteoarthritis (group II). a, b Anteroposterior Grashey and axillary views showed concentric osteoarthritis with central glenoid erosion. c, d Immediate post-operative (2 months) anteroposterior and axillary views of the joint with the MB glenoid component (SMR™ LIMA, San Daniele del Friuli, Italy). The humeral head is centered in the glenoid and the implant is stable. e, f Last follow-up radiographs (32 months) of the patient whose joint is depicted in (c, d) showing superior (e) and anterior subluxation (f) of the humeral head
The modularity of the failed implant described in the Fig. 5 c, d allowed revision to a reverse prosthesis using a 44 mm polyethylene glenosphere without changing the humeral stem and the baseplate. MB metal-backed
There were no cases of oversized resurfacing heads.
HOs were detected in four SMR™ TSAs (one in group I and three in group II) and in one Ascend™ of the group I.
A subgroup analysis failed to highlight any radiographic differences between the pyrocarbon and the standard cobalt-chromium HAs in either group. Humeral radiolucency was significantly associated with SST and ER delta scores (p = 0.035 and p = 0.01, respectively). The ER delta scores were also associated with glenoid radiolucency (p = 0.007).
Discussion
Replacement of a joint where arthritis had developed after glenohumeral stabilization ensures good pain relief and recovery of shoulder function, as demonstrated in this and other studies [5, 7, 21]. These patients had significantly better post-operative ER and IR than the primary osteoarthritis patients, whereas there were no between-group differences in the other planes of motion. The significantly higher flexion and abduction recorded in HA compared with TSA group I patients should be interpreted with caution, given the limited HA sample. This notwithstanding, we believe that the careful anterior soft-tissue release performed in patients of both groups was more effective to recover shoulder rotations in arthritis after instability surgery patients. Pain, SST score, and CS were similar in the two groups, also after comparing HA and TSA between groups.
All participants shared pre-operative concentric osteoarthritis [22, 23], but group II showed a prevalence of A2 and B1 glenoids. The difference may be due to fast osteoarthritis onset and good superior-posterior rotator cuff balance in group I. Moreover, the lack of associations between type of glenoid arthritis and clinical outcomes is probably related to the absence of B2 glenoids (severe wear) and to the small number of B1 glenoids in both groups. Although the present findings do not fully confirm the starting hypothesis that the two patient groups would share comparable outcomes, they do highlight some close similarities. Persistently altered glenohumeral kinematics and increased posterior forces secondary to rotator cuff imbalance reasonably contribute to posterior glenoid wear [32]. Anterior glenoid wear (type D) was detected in a group I patient where open staple capsulorrhaphy promoted anterior humeral head subluxation. The controversy surrounding glenoid replacement in young arthritic patients led us to prefer, in some cases, a stemmed HA or HHR. Resurfacing restores proximal humeral head anatomy [33]; in our study, it was performed in patients with good rotator cuff status and normal glenoid retroversion, which ensure that the head is centered in the glenoid. We used a size smaller than the native head, to prevent oversize stress on the rotator cuff. The curved design of the press-fit stem used in stemmed HAs and in 45% of TSAs preserved the tuberosities (except in one case), reduced the risk of stress-shielding, and was associated with little radiolucency, as reported by other researchers [34, 35] and by a recent study of a standard straight stem [36]. We implanted the standard modular stem in 4 of 13 TSA patients with proximal humeral arthritic deformity or head necrosis, where a short stem is at risk of loosening. In stemmed HAs and in one HHR patient, we used a pyrocarbon prosthesis, whose elastic module is similar to cortical bone; the device has demonstrated favourable wear characteristics in an animal model [37] and could reduce the risk of bone resorption [38]. Two recent clinical studies have reported promising mid-term outcomes with pyrocarbon interposition shoulder arthroplasty in young patients with avascular necrosis and primary and secondary osteoarthritis (sequelae of instability surgery or fractures) [39, 40]. The PE glenoid component of TSA implants also showed good clinical outcomes in both groups; this agrees with our previous experience [41], where central peg osteolysis did not affect clinical outcomes but was considered as a risk factor for loosening and was thus monitored yearly by CT.
The MB glenoid used in 50% of TSAs of group I and 30% of group II prompts some considerations. In 2010, Castagna and co-workers reported that it provided good to satisfactory mid-term results in patients with shoulder osteoarthritis [42]. However, we detected problems (PE wear and dissociation and metallosis) in the failed MB glenoid component of group II in line with the results of the SMR™ system recorded in the Australian shoulder prosthesis registry [43] and by other reports [44].
The outcome data of our patients with arthritis secondary to stabilization surgery are in line with other studies. Bigliani et al. [5] described 77% of satisfactory and 23% of unsatisfactory results at an average follow-up of three years in 12 TSA patients and five patients with humeral head replacement. We concur with their decision to replace the glenoid based on its bone stock and shape, choosing HA in young active patients with concentric joints and glenoid replacement in patients with asymmetric bone loss. Subscapularis shortening was mostly managed by suturing the tendon to the anatomical neck rather than to its lateral anatomical insertion on the lesser tuberosity and in the other cases by z-lengthening. Since in our experience z-plasty is not effective in treating IR contracture, we medialized its insertion as described by Bigliani et al. [5]. We found subscapularis shortening and severe anterior soft-tissue contracture in patients with a longer interval from shoulder stabilization to replacement. Green et al. [7] reported pain relief and increased shoulder mobility in 93% of 17 arthroplasties (15 TSAs and 2 HAs) at a mean follow-up of 62 months. They used z-lengthening in patients with ER stiffness, to which the above considerations apply. The largest series was described by Sperling and co-workers [21], who reported significant improvement in pain, ER, and abduction in 33 patients at a mean follow-up of seven years, despite unsatisfactory results in 4/10 HAs and 13/21 TSAs; 11 revisions (3 among HA and 8 among TSA patients); and a survivorship of 86% at five years and 61% at ten years. Young patients with high physical demands remain an outstanding concern; we feel that glenoid replacement in shoulders with A2 and B1 morphology contributed to the low rate of complications and revisions. Furthermore, the strict criteria applied for humeral replacement (preferably A1 glenoid type) may explain the difference from a recent study reporting better IR and clinical outcomes in TSA than HA patients with A2 or B1 glenoids [45]. Systematic reviews and randomized controlled trials have also confirmed that TSA is more effective than HA in patients with shoulder arthritis [46,47,48] and involves less need for revision [49].
The present findings prompt the following considerations:
-
i)
The clinical and radiographic outcomes of shoulder replacement in arthritis secondary to instability surgery are partially comparable to those of primary arthritis
-
ii)
Careful anterior capsular release and subscapularis tendon medialization are recommended to manage IR contracture
-
iii)
HA is a reasonable option in young patients with a centered humeral head and few arthritic changes, where glenoid replacement is controversial;
-
iv)
Although pyrocarbon is a promising alternative to standard head materials, inconsistent evidence in large joints warrants long-term studies before it is used in shoulder arthritis [37, 50]
-
v)
In patients with advanced glenoid arthritis (A2 and B1) and in those aged 50 years or older, TSA with a partially cemented PE glenoid is preferable to an MB implant. In B2 and B3 glenoids, posterior augmented components or reverse TSA should be considered.
The main limitations of this study are the retrospective design and the small samples of patients with arthritis secondary to instability surgery and of HA cases (which include HHR and short-stem prostheses). Nonetheless, we feel these data provide fresh insight on standard and short-stem humeral components and on the use of a pyrocarbon humeral head. Moreover, they confirm that the degenerative changes arising after shoulder stabilization are similar to those seen in primary osteoarthritis.
References
Rollick et al (2017) Long-term outcomes of the Bankart and Latarjet repairs: a systematic review. Open Access J Sports Med 8:97–105. https://doi.org/10.2147/OAJSM.S106983
Paladini P, Singla R, Merolla G, Porcellini G (2016) Latarjet procedure: is the coracoid enough to restore the glenoid surface? Int Orthop 40:1675–1681. https://doi.org/10.1007/s00264-015-3093-z
Hohmann E, Tetsworth K, Glatt V (2017) Open versus arthroscopic surgical treatment for anterior shoulder dislocation: a comparative systematic review and meta-analysis over the past 20 years. J Shoulder Elb Surg 26:1873–1880. https://doi.org/10.1016/j.jse.2017.04.009
Neer CS (1990) Shoulder reconstruction. WB Saunders, Philadelphia, pp 208–212
Bigliani LU, Weinstein DM, Glasgow MT et al (1995) Glenohumeral arthroplasty for arthritis after instability surgery. J Shoulder Elbow Surg 2:87–94
van der Zwaag HM, Brand R, Obermann WR, Rozing PM (1999) Glenohumeral osteoarthrosis after Putti-Platt repair. J Shoulder Elbow Surg 8:252–258
Green A, Norris TR (2001) Shoulder arthroplasty for advanced glenohumeral arthritis after anterior instability repair. J Shoulder Elbow Surg 10:539–545
Buscayret F, Edwards TB, Szabo I, Adeleine P, Coudane H, Walch G (2004) Glenohumeral arthrosis in anterior instability before and after surgical treatment: incidence and contributing factors. Am J Sports Med 32:1165–1172. https://doi.org/10.1177/0363546503262686
Allain J, Goutallier D, Glorion C (1998) Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 80:841–852
Chapnikoff D, Besson A, Chantelot C et al (2000) Bankart procedure: clinical and radiological long-term outcome. Rev Chir Orthop Reparatrice Appar Mot 86:558–565
O’Neil DB (1999) Arthroscopic Bankart repair of anterior detachments of the glenoid labrum: a prospective study. J Bone Joint Surg Am 81:1357–1366
Rosenberg BN, Richmond JC, Levine WN (1995) Long-term followup of Bankart reconstruction: incidence of late degenerative glenohumeral arthrosis. Am J Sports Med 23:538–544
Hawkins RJ, Angelo RL (1990) Glenohumeral osteoarthrosis: a late complication of the Putti-Platt repair. J Bone Joint Surg Am 72:1193–1197
Lusardi DA, Wirth MA, Wurtz D et al (1993) Loss of external rotation following anterior capsulorrhaphy of the shoulder. J Bone Joint Surg Am 75:1185–1192
MacDonald PB, Hawkins RJ, Fowler PJ et al (1992) Release of the subscapularis for internal rotation contracture and pain after anterior repair for recurrent anterior dislocation of the shoulder. J Bone Joint Surg Am 74:734–737
Hawkins RH, Hawkins RJ (1985) Failed anterior reconstruction for shoulder instability. J Bone Joint Surg Br 67:709–714
O’Driscoll SW, Evans DC (1993) Long-term results of staple capsulorrhaphy for anterior instability of the shoulder. J Bone Joint Surg Am 75:249–258
Zuckerman JD, Matsen FA (1984) Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg am 66:175–180
Franceschi F, Papalia R, Del Buono A, Vasta S, Maffulli N, Denaro V (2011) Glenohumeral osteoarthritis after arthroscopic Bankart repair for anterior instability. Am J Sports Med 39:1653–1659. https://doi.org/10.1177/0363546511404207
Matsen FA, Rockwood CA, Wirth MA et al (1998) Gleno-humeral arthritis and its management. In: Rockwood CA, Matsen FA (eds) The shoulder, 2nd edn. WB Saunders, Philadelphia, pp 870–872
Sperling JW, Antuna SA, Sanchez-Sotelo J, Schlek C, Cofield RH (2002) Shoulder arthroplasty for arthritis after instability surgery. J Bone J Surg Am 84-A:1775–1781
Samilson RL, Prieto V (1983) Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 65:456–460
Gerber C (1992) Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Relat Res:152–160
Bercik MJ, Kruse K II, Yalizis M, Gauche M-O, Chaoui J, Walch G (2016) A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elbow Surg 25:1601–1607. https://doi.org/10.1016/j.jse.2016.03.010
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Parsons IM, Millett PJ, Warner JP (2004) Glenoid wear after shoulder hemiarthroplasty. Clin Orthop Rel Res 421:120–125
Schnetzke M, Coda S, Raiss P, Walch G, Loew M (2016) Radiologic bone adaptations on a cementless short-stem shoulder prosthesis. J Shoulder Elb Surg 25:650–657. https://doi.org/10.1016/j.jse.2015.08.044
Sperling JW, Cofield RH, O’Driscoll SW, Torchia ME, Rowland CM (2000) Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg 9:507–513
Sperling JW, Cofield RH, Rowland CM (1998) Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less: long-term results. J Bone Joint Surg Am 80:464–473
Levy O, Tsvieli O, Merchant J, Young L, Trimarchi A, Dattani R et al (2015) Surface replacement arthroplasty for glenohumeral arthropathy in patients aged younger than fifty years: results after a minimum ten-year follow-up. J Shoulder Elb Surg 24:1049–1060. https://doi.org/10.1016/j.jse.2014.11.035
Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH (2006) Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am 88:2637–2644. https://doi.org/10.2106/JBJS.E.01383
Domos P, Checchia CS, Walch G (2018) Walch B0 glenoid: pre-osteoarthritis posterior subluxation of the humeral head. J Shoulder Elb Surg 27:181–188. https://doi.org/10.1016/j.jse.2017.08.014
Deladerrière JY, Szymanski C, Vervoort T, Budzik JF, Maynou C (2012) Geometrical analysis results of 42 resurfacing shoulder prostheses: a CT scan study. Orthop Traumatol Surg Res 98:520–527. https://doi.org/10.1016/j.otsr.2012.03.010
Schnetzke M, Preis A, Coda S, Raiss P, Loew M (2017) Anatomical and reverse shoulder replacement with a convertible, uncemented short-stem shoulder prosthesis: first clinical and radiological results. Arch Orthop Trauma Surg 137:679–684. https://doi.org/10.1007/s00402-017-2673-3
Szerlip BW, Morris BJ, Laughlin MS, Kilian CM, Edwards TB (2018) Clinical and radiographic outcomes after total shoulder arthroplasty with an anatomic press-fit short stem. J Shoulder Elb Surg 27:10–16. https://doi.org/10.1016/j.jse.2017.08.012
Merolla G, Walch G, Ascione F, Paladini P, Fabbri E, Padolino A, Porcellini G (2017) Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2017.10.016
Cook SD, Thomas KA, Kester MA (1989) Wear characteristics of the canine acetabulum against different femoral prostheses. J Bone Surg Br 71:189–197
Stanley J, Klawitter J, More R (2008) Replacing joints with pyrolytic carbon. In: Rewell PA (ed) Joint replacement technology. Woodhead publishing, pp 631–656
Garret J, Godeneche A, Boileau P, Molé D, Etzner M, Favard L et al (2017) Pyrocarbon interposition shoulder arthroplasty: preliminary results from a prospective multicenter study at 2 years of follow-up. J Shoulder Elb Surg 26:1143–1151. https://doi.org/10.1016/j.jse.2017.01.002
Hudek R, Werner B, Abdelkawi AF, Gohlke F (2017) Pyrocarbon interposition shoulder arthroplasty in advanced collapse of the humeral head. Orthopade 46:1034–1044. https://doi.org/10.1007/s00132-017-3495-2
Merolla G, Ciaramella G, Fabbri E, Walch G, Paladini P, Porcellini G (2016) Total shoulder replacement using a bone ingrowth central peg polyethylene glenoid component: a prospective clinical and computed tomography study with short- to mid-term follow-up. Int Orthop 40:2355–2363. https://doi.org/10.1007/s00264-016-3255-7
Castagna A, Randelli M, Garofalo R, Maradei L, Giardella A, Borroni M (2010) Mid-term results of a metal-backed glenoid component in total shoulder replacement. J Bone Joint Surg Br 92:1410–1415. https://doi.org/10.1302/0301-620X.92B10.23578
Khan LAK, Page RS, Miller LN, Graves SE (2012) Risk factors for early revision after shoulder arthroplasty: 7113 shoulder arthroplasties from the Australian Orthopaedic Association National Joint Replacement Registry. Orthop Proc 94-B(Supp 39):123
Boileau P, Moineau G, Morin-Salvo N, Avidor C, Godeneche A, Levigne C et al (2015) Metal-backed glenoid implant with polyethylene insert is not a viable long-term therapeutic option. J Shoulder Elb Surg 24:1534–1543. https://doi.org/10.1016/j.jse.2015.02.012
Pastor MF, Kaufmann M, Gettmann A, Wellmann M, Smith T (2015) Total versus hemiarthroplasty for glenohumeral arthritis according to preoperative glenoid Erosion. Orthop Rev (Pavia) 7:51–54. https://doi.org/10.4081/or.2015.5923
Duan X, Zhang W, Dong X, Liu M, Gao Y, Huang F, Li J, Xiang Z (2013) Total shoulder arthroplasty versus hemiarthroplasty in patients with shoulder osteoarthritis: a meta-analysis of randomized controlled trials. Semin Arthritis Rheum 43:297–302. https://doi.org/10.1016/j.semarthrit.2013.04.002
Sandow MJ, David H, Bentall SJ (2013) Hemiarthroplasty vs total shoulder replacement for rotator cuff intact osteoarthritis: how do they fare after a decade? J Shoulder Elb Surg 22:877–885. https://doi.org/10.1016/j.jse.2012.10.023
Singh JA, Sperling J, Buchbinder R, McMaken K (2011) Surgery for shoulder osteoarthritis: a Cochrane systematic review. J Rheumatol 38:598–605. https://doi.org/10.3899/jrheum.101008
van den Bekerom MP, Geervliet PC, Somford MP, van den Borne MP, Boer R (2013) Total shoulder arthroplasty versus hemiarthroplasty for glenohumeral arthritis: a systematic review of the literature at long-term follow-up. Int J Shoulder Surg 7:110–115. https://doi.org/10.4103/0973-6042.118915
Bernasek TL, Stahl JL, Pupello D (2009) Pyrolytic carbon endoprosthetic replacement for osteonecrosis and femoral fracture of the hip: a pilot study. Clin Orthop Relat Res 467:1826–1832. https://doi.org/10.1007/s11999-009-0820-z
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merolla, G., Cerciello, S., Marenco, S. et al. Comparison of shoulder replacement to treat osteoarthritis secondary to instability surgery and primary osteoarthritis: a retrospective controlled study of patient outcomes. International Orthopaedics (SICOT) 42, 2147–2157 (2018). https://doi.org/10.1007/s00264-018-3969-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3969-9