Abstract
Purpose
Osteoarthritis may be observed after surgery for instability and in the natural history of pathology. The primary objective was to analyze the late clinical and radiographic results of reverse shoulder arthroplasties (RSA) for patients who had instability arthropathy.
Methods
This is a retrospective cohort of 25 patients with a mean follow-up of 6.6 years. Patients had a history of instability surgery (80%) or multiple closed reductions. All were clinically evaluated with the constant score (CS), and radiologically (true AP view and Y view).
Results
No significant differences in pre- and post-operative function, radiologic status, and complication rate between the patients treated with a prior bone block procedure for the anterior instability and those treated by a capsular plication or non-operatively. A 36-mm sphere was implanted in 67%. Bone grafting of the glenoid was needed in 71%. No intra-operative complication has been reported. Clinically, the active anterior elevation increased from 70° to 140° (p < 0.01) and external rotation from 9° to 21° (p = 0.02). The adjusted CS increased from 38 to 98 (p < 0.01). Two early post-operative complications were collected: one spine fracture and one superficial infection. No early or late dislocation or neurologic complication was observed. At the latest follow-up, there were 38.10% of glenoid spurs, and 55% of scapular notch.
Conclusions
The overall complication rate in this specific group is relatively low. Patients’ satisfaction rate is high and clearly higher than those reported with anatomic TSA for this indication. Clinical results are comparable to other studies describing results of RSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent anterior shoulder dislocation is a challenging pathology with a relative high rate of recurrence even after surgery. At the long term follow-up, osteoarthritis may be observed even if the shoulder remains stable, due to the pathology itself, and to recurrence [1,2,3,4,5,6], or to the treatment (technical errors—problems related to intra-articular screws or anchors placement) [7,8,9,10,11].
Non-constrained anatomic shoulder arthroplasties (total shoulder replacement or hemiarthroplasties) lead to good clinical results if the shoulders remain stable. Nevertheless, this surgical option is associated with a high rate of revision (18 to 35%) essentially because of failure with one or more dislocations [12,13,14,15,16]. Therefore, semi-constrained reversed shoulder arthroplasty (RSA) could theoretically reduce the rate of recurrent dislocation due to the inherent stability of this implant design. This surgical option has also the advantage to manage both associated rotator cuff deficiency together with glenoid bone loss (possible bone grafting behind the glenoid baseplate). Results of RSA for locked anterior shoulder dislocation are known [17, 18]. Even if clinical and radiological results are in this indication not as good as RSA for more classic indications, the stability of the implants seems better than the stability of TSA, as well as the revision rate [18].
The working hypothesis of this study is that results of RSA for patient with instability arthropathy, i.e., had previous surgical stabilization procedures for recurrent anterior shoulder instability or a long-standing history of dislocations are specific or differ from reverse shoulder arthroplasties for cuff tear arthropathy [19,20,21]. The primary objective of this study was to analyze the late clinical and radiographic results of RSA for patients who had instability arthropathy (patients with chronic locked dislocation excluded). The secondary objective was to analyze the complications rate and survival curves of this cohort.
Patients and methods
Flowchart
This is a retrospective and a multicenter study. Twenty-five patients with a minimum follow-up of two years have been included and 19 have an over five year follow-up. All patients were included even if the follow-up was not of five years to have an overview on the population, and on the potential complications in this specific indication. But only those with a minimal follow-up of five years have been included for the study of the long-term results. Inclusions criteria were as follows:
-
1.
Previous history of shoulder instability with a previous surgery (Bankart repair or bone block procedure as Latarjet or Bristow) (Fig. 1)
-
2.
Previous multiple closed reductions.
Exclusion criteria were chronic locked dislocations or dislocations.
This cohort included 52% of women, with a mean age of 69.9 years at inclusion and a mean follow-up of 6.6years (maximum of 11.6 years). Only two patients were lost for the follow-up (dead). Seventy-six percent right shoulders were involved, and the dominant side was involved in 77.3% of the cases. Patient’s mean BMI was 26.92. Eighty percent of the patients had a prior surgery for instability (36% of Latarjet or Bristow (7 patients) and capsular surgery for the others) and 20% had multiple closed reduction in their history. Mean delay between the initial procedure or first dislocation and the surgery was 50.3 years (SD 13.48 years). Thirteen percent of the 25 patients had a failed history of cuff repair (3 patients); an intact cuff was found for the others. Main risks factors for shoulder instability found were alcoholism in 15.4%, dementia in 7.7%, and Parkinson disease in 7.7% of the cases. None of the patients experienced transitory axillary nerve palsy in their instability history.
Demographic characteristics
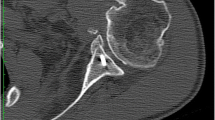
All patients were evaluated through their charts for the pre-operative data and evaluated at the last follow-up with a clinical examination: constant score (CS) [22], simple shoulder value (SSV) [23], and with a radiologic evaluation (minimum: true AP view and scapular Y view and pre-operative CT scan when available (Fig. 2)). All complications (pre- and post-operative) were documented and analyzed as minor (without surgery) or major (vascular or nerve complication and/or with revision surgery).
Statistical analysis
Appropriate descriptive statistics, including means, minimums, maximums, and standard deviations (SD) were computed for each of the examined variables. Wilcoxon signed rank tests were performed to compare pre-operative and post-operative changes in active mobility, and clinical objective and subjective scores. For all statistical tests, p < 0.05 was used to determine the significance.
Results
Surgery
The pre-operative glenoid morphology according to Walch’s classification was type A1—67%, A2—17%, B1—11%, and B2—5% in the horizontal plane [24]; and on the vertical plane according to Favard’s classification: E0—38%, E1—23%, E2—8%, E3—8%, and E4—23% [25].
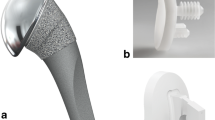
Eighty percent of the patients were operated upon through a deltopectoral approach. In all case, an extensive peri-glenoidal release, biceps tenotomy, has been done, without resection of osteophytes. A glenoid bone graft, harvested from the humeral head, was needed in 71% of the cases to correct deformation in the horizontal or vertical plane or to graft the anterior defect related to previous dislocations (asymmetrical Bio-RSA) [26, 27]. A 36-mm sphere was implanted in 67% with a 29-mm-diameter baseplate in 91% and a short post in 70% of the cases (to secure the bone graft needed for glenoid reconstruction) (Aequalis Reversed system, Tornier, Montbonno, France). On the humeral side, a Gramon type of reversed prosthesis (Aequalis Reversed 2, Tornier, Montbonno, France) was implanted with 20° of retroversion. Trans-osseous sub-scapularis was done at the end of the surgery for those detached (deltopectoral approach).
All patients were put in a sling in neutral rotation for a month, before starting their rehabilitation under the control of a physiotherapist. In the case of dementia, patients were authorized to move their shoulder right away.
Pre-operative cuff status
Seven patients had a rotator cuff rupture, involving the anterosuperior cuff in one case, the antero-superior cuff with an extension to the posterior cuff in three cases and a postero-superior tear in three cases. All had a previous repair of their cuff. The pre-operative fatty infiltration for each muscle of the rotator cuff is reported in Table 1.
Clinical results
The age- and gender-adjusted constant score improved from 37.9% (range, 0–22%) pre-operatively to 97.8% (range, 26–79%) at the most recent follow-up (p < .001). All items of the CS significantly increased, especially for the arc of motion.
Active forward Elevation increased from 70.4° pre-operatively to 139.5° post-operatively (p < .001) and mean active external rotation from 8.8° to 20.5° (p = 0.02).
Patient’s satisfaction is high with a final SSV of 75.
The clinical results are presented in Tables 2 and 3.
Radiologic results
Pre-operative arthritic changes (n = 25 patients) shown on plain X-rays according to Hamada’s classification [28]: two stage 1 (Fig. 1), three stage 2, four stage 3, ten stage 4A, one stage 4B, and five stage 5.
Post-operatively, the baseplate was inserted flush in 35%, low in 50%, and very low 15%. At the latest follow-up, glenoid spurs were observed in 38.10% of the cases. A scapular notch was found in 40% of the cases (10 patients): five grade 1, three grade 2, and two grade 4.
Complications
No intra-operative complication has been reported. Two early post-operative complications were collected during the first post-operative year: one spine fracture treated conservatively with a good result (SSV = 90 and CS = 72) (Fig. 3) and one superficial infection treated with a washout and a synovectomy with a favourable evolution. No dislocation or neurologic complication has been reported.
For the long-term complication, one patient presented a severe stiffness of his shoulder treated with capsular release and synovectomy. The result was considered as unsatisfactory.
Comparisons
No significant differences in pre- and post-operative function, pre- and post-operative radiologic status, and complication rate between the patients treated with a prior bone block procedure for the anterior instability and those treated by a capsular plication or non-operatively.
Discussion
The occurrence of osteoarthritis of the glenohumeral joint following surgical stabilization procedures is related to the pathology itself, and not to surgical procedure (except in case of technical errors such as intra-articular screw placement). These osteoarthritic changes are in all planes [2, 3]. Moreover, there are osseous defect related to instability (5.4 to 32% incidence of anterior glenoid rim fractures in the literature) [1]. Anatomic shoulder arthroplasty (total or hemi) has been suggested as an option for patients with arthritis following shoulder stabilization surgery with improvement of function and pain relief [29]. But, there is a higher rate of complications and revisions for this group of patients when compared with those of unconstrained shoulder replacement for primary osteoarthritis, up to 40% for Lehmann et al. [16], Matsoukis et al. [15], or Sperling et al. [14] with about 20% of patients requiring a revision procedure [12, 13]. For those reasons, reverse shoulder arthroplasty has been introduced to facilitate post-operative rehabilitation and improve function of the shoulder without compromising the stability of the prosthesis (Fig. 4). In this cohort, main indication for RSA instead of TSA was the presence of a rupture of the subscapularis tendon or an isolated fatty infiltration of the subscapularis muscle, and in most cases, other rotator cuff tendons were also ruptured. We have excluded patients with an anterior or posterior locked dislocation because this is a specific group of patients for which reversed shoulder arthroplasty indication has been clearly demonstrated [30].
Bone grafting remains mandatory to reconstruct the defect or to correct the glenoid deformation (71% in this study). The overall complication rate in this specific group is relatively low and acceptable compared with these other studies. We have found no recurrence of instability in this cohort, as it has been published [3, 29]. The satisfaction rate is high and clearly higher than those reported with anatomic TSA in the indication. Clinical results are comparable to other studies describing results of RSA.
The main weakness of this study is its retrospective design. Nevertheless, the cohort is one of the largest published.
The present study has some limitations. The major limitation is the short cohort related to the aetiology.
Conclusions
The improvement in objective and subjective scores, with a low rate of complications makes RSA a reliable treatment option in case of osteoarthritic joints secondary to previous shoulder stabilization procedures, or in case of post-instability arthropathy. The improvements in clinical and radiographic outcomes are comparable with those of another cohort of RSA for cuff tear arthropathy.
References
Rowe C, Sakellarides H (1961) Factors related to recurrences of anterior dislocations of the shoulder. Clin Orthop 20:40–48
Schandelmaier P, Blauth M, Schneider C, Krettek C (2002) Fractures of the glenoid treated by operation. A 5- to 23-year follow-up of 22 cases. J Bone Joint Surg 84(B):173–177. https://doi.org/10.1302/0301-620X.84B2.12357
Raiss P, Baumann F, Akbar M, Rickert M, Loew M (2009) Open screw fixation of large anterior glenoid rim fractures: mid- and long-term results in 29 patients. Knee Surg Sports Traumatol Arthrosc 17:195–203. https://doi.org/10.1007/s00167-008-0677-9
Hovelius L (1987) Anterior dislocation of the shoulder in teen-agers and young adults: five-year prognosis. J Bone Joint Surg 69(A):393–399
Hovelius L, Augustini B, Fredin H, Johansson O, Norlin R, Thorling J (1996) Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am 78:1677–1684
Neyton L, Young A, Dawidziak B, Visona E, Hager J, Fournier Y, Walch G (2012) Surgical treatment of anterior instability in rugby union players: clinical and radiographic results of the Latarjet-Patte procedure with minimum 5-year follow-up. J Shoulder Elb Surg 21:1721–1727. https://doi.org/10.1016/j.jse.2012.01.023
Wall M, Warren R (1995) Complications of shoulder instability surgery. Clin Sports Med 14:973–1000
Walch G (1996) Chronic anterior glenohumeral instability. J Bone Joint Surg (Br) 78:670–677
Walch G (2000) Chronic anterior instability of the shoulder in adults. Summary. Rev Chir Orthop 86(Suppl 1):147–149
Hovelius L, Korner L, Lundberg B, Akermark C, Herberts P, Wredmark T, Berg E (1983) The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow-Latarjet procedure. J Bone Joint Surg 65(A):926–934
Hovelius L, Thorling J, Fredin H (1979) Recurrent anterior dislocation of the shoulder: results after Bankart and Putti-Platt operations. J Bone Joint Surg 61(A):566–569
Bigliani L, Weinstein D, Glasgow M (1995) Glenohumeral arthroplasty for arthritis after instability surgery. J Shoulder Elb Surg 4:87–94
Green A, Norris T (2001) Shoulder arthroplasty for advanced glenohumeral arthritis after anterior instability repair. J Shoulder Elb Surg 10(6):539–545
Sperling J, Cofield R, Steinmann S (2002) Shoulder arthroplasty for osteoarthritis secondary to glenoid dysplasia. J Bone Joint Surg 84(A):541–546
Matsoukis J, Tabib W, Mandelbaum A, Walch G (2003) Shoulder arthroplasty for non-operated anterior shoulder instability with secondary osteoarthritis. Rev Chir Orthop 89:7–18
Lehmann L, Magosch P, Mauermann E, Lichtenberg S, Habermeyer P (2010) Total shoulder arthroplasty in dislocation arthropathy. Int Orthop 34:1219–1225. https://doi.org/10.1007/s00264-009-0928-5
Werner B, Böhm D, Abdelkawi A, Gohlke F (2014) Glenoid bone grafting in reverse shoulder arthroplasty for long-standing anterior shoulder dislocation. J Shoulder Elb Surg 23:1655–1661. https://doi.org/10.1016/j.jse.2014.02.017
Kurowicki J, Triplet J, Momoh E, Moor M, Levy J (2016) Reverse shoulder prosthesis in the treatment of locked anterior shoulders: a comparison with classic reverse shoulder indications. J Shoulder Elb Surg 25:1954–1960. https://doi.org/10.1016/j.jse.2016.04.019
Flatow E, Miller S, Neer C (1993) Chronic anterior dislocation of the shoulder. J Shoulder Elb Surg 2:2–10. https://doi.org/10.1016/S1058-2746(09)80131-6
Buscayret F, Edwards T, Szabo I, Adeleine P, Coudane H, Walch G (2004) Glenohumeral arthrosis in anterior instability before and after surgical treatment: incidence and contributing factors. Am J Sports Med 32:1165–1172
Samilson R, Prieto V (1983) Dislocation arthropathy of the shoulder. J Bone Joint Surg 65(A):456–460
Constant C, Murley A (1987) A clinical method of functional assessment of the shoulder. Clin Orthop 214:160–164
Gilbart M, Gerber C (2007) Comparison of the subjective shoulder value and the constant score. J Shoulder Elb Surg 16:717–721
Walch G, Badet R, Boulahia A, Khoury A (1999) Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplast 14:756–760
Lévigne C, Boileau P, Favard L, Garaud P, Molé D, Sirveaux F, Walch G (2008) Scapular notching in reverse shoulder arthroplasty. J Shoulder Elb Surg 17:925–935. https://doi.org/10.1016/j.jse.2008.02.010
Boileau P, Moineau G, Roussanne Y, O’Shea K (2011) Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 469:2558–2567. https://doi.org/10.1007/s11999-011-1775-4
Hill J, Norris T (2001) Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg 83(Am):877–883
Hamada K, Fukuda H, Mikasa M, Kobayashi Y (1990) Roentgenographic findings in massive rotator cuff tears. Clin Orthop 254:92–96
Merolla G, Cerciello S, Marenco S, Fabbri E, Paladini P, Porcellini G (2018) Comparison of shoulder replacement to treat osteoarthritis secondary to instability surgery and primary osteoarthritis: a retrospective controlled study of patient outcomes. Int Orthop 12. https://doi.org/10.1007/s00264-018-3969-9
Statz J, Schoch B, Sanchez-Sotelo J, Sperling J, Cofield R (2017) Shoulder arthroplasty for locked anterior shoulder dislocation: a role for the reversed design. Int Orthop 41:1227–1234. https://doi.org/10.1007/s00264-017-3450-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Except Agathe Kling, all authors have the same conflict of interest with Wright-Tornier.
Additional information
Level IV study: retrospective study
Level of evidence: Level IV, Case Series, Treatment Study
Rights and permissions
About this article
Cite this article
Clavert, P., Kling, A., Sirveaux, F. et al. Reverse shoulder arthroplasty for instability arthropathy. International Orthopaedics (SICOT) 43, 1653–1658 (2019). https://doi.org/10.1007/s00264-018-4123-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4123-4