Abstract
Purpose
Modular cementless elastic acetabular systems have advantages over cemented and hard shell cementless acetabular systems. There are few reports on the medium-term and long-term follow up of this particular type of implant. This study describes our experience with the Atlas IIIp modular acetabular system, which is a thin shell cementless elastic acetabular implant for total hip replacement commercialized under this name in many countries.
Methods
We prospectively followed 244 patients treated with Atlas IIIp acetabular system between 2001 and 2004. Minimum ten year follow up was available for 148 hips (139 patients) from the original cohort of 263 hips (244 patients). One hundred five patients had died from unrelated causes and were excluded from the results. Post-operative and follow up radiographs of patients were assessed; and Harris hip scores were used as clinical outcome. Revision for any reason was defined as the end point for survivorship analysis.
Results
The mean pre-operative Harris hip score was 48 (S.D. 16) and the average post-operative score was 82 (S.D. 12). The mean follow up in our series was 11.5 years, ranging from ten to 13.5 years. Thirteen hips required further surgery in our cohort; of which ten cases required cup revision. The 13-years cumulative implant survival was 91.2 % and the risk of implant revision was 8.8 % at 13 years in 148 hips (139 patients). Kaplan-Meier analysis showed the implant survival rate of 95.2 % at ten years for revision for any reason and 99.4 % for aseptic loosening.
Conclusions
Our clinical experience with this acetabular cup suggests good long-term survival rates that are similar to other cups on the market. The clinical experience in this study shows long-term survival rates that are consistent, acceptable and good results achieved with a low revision rate.
Level of evidence: Therapeutic III; therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Atlas IIIp hip implant (FH medical) is a hydroxyapitite (HA) coated cementless elastic press-fit acetabular component. There have been reports from France suggesting excellent long-term results, with <1 % of fixation failure at ten years [1, 2]. There are no long-term clinical results of this component from an independent centre in the United Kingdom (UK).
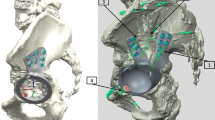
The Atlas IIIp is a modular cementless system consisting of a rough under surface, multi-perforated HA coated hemispherical titanium alloy (TiAl6V4) shell with four anti rotation spikes. It also has a large central opening with a vertical split in the lower part of the shell (Fig. 1). The cylindrical conventional polyethylene (GUR1050) liner features an anti-rotation cuff and edge protection design (Fig. 2) [3]. The press fit fixation of the acetabular component, is achieved as the shell is impacted, the split closes and stores elastic energy and facilitates its penetration into the acetabulum. When the polyethylene liner impacts into the shell, the split opens and releases some of the energy to produce a strong bone to component interface as well as component-to-component interface (Fig. 3) [2]. In vitro biomechanical studies have suggested that this method of fixation can produce an expansion force of 400 N in a 50 mm diameter system [3]. The primary fixation of the Atlas IIIp system is provided by the elastic recoil, which allows an impaction on preload and also by the four anti-rotating pins.
The press fit fixation of the acetabular component, is achieved as the shell is impacted, the split closes and stores elastic energy and facilitates its penetration into the acetabulum. When the polyethylene liner impacts into the shell, the split opens and releases some of the energy to produce a strong bone to component interface as well as component-to-component interface
The secondary fixation of a cementless component requires osteointegration, the firm and reliable adherence of the bone to the implant and later the absence of adverse bone remodelling or reaction, including stress shielding and osteolysis. Pakvis et al. demonstrated in their finite element analysis that the press fit elastic socket model showed the most equivalent load transmission compared to the anatomical acetabular model [4]. It suggested that the elastic model has the most physiological load transmission on acetabular bone and therefore will lead to the least acetabular stress shielding. The aim of this paper was to report the long-term results for the Atlas IIIp elastic cementless acetabular component from an independent centre in the United Kingdom.
Patient and methods
Between March 2001 and December 2004, 263 consecutive hip arthroplasties in 244 patients underwent primary and revision total hip arthroplasty, using the Atlas IIIp acetabular component and various femoral implants, 19 had staged bilateral surgery and 75 were for revision indications. The exclusion criterion for patient selection for revision surgery was recurrent dislocation where a capture device would be used instead. Our institutional review board approved this study and all data was collected prospectively.
The operations were performed via standard posterior approach by the senior author or by trainees under his direct (scrubbed) supervision as first assistant. The Atlas IIIp component was inserted with the standard instruments provided by the manufacturer. The acetabulum was reamed as per pre-operative template and the final component impacted was 2 mm greater than the diameter of the final reamer. The size of the polyethylene liners varied between 28 and 32 mm depending on the size of the acetabular component. Operation notes were recorded prospectively into a local database and patients were followed up at six weeks, three months, one year, two years, five years, ten years and yearly thereafter, with clinical review and radiological assessments. Patients were assessed pre-operatively and at regular intervals post-operatively. In addition to physical examination, pain and functional outcomes were reported by the patient Harris hip scores (HHS). The primary outcome was revision. The secondary outcomes were the Harris hip scores (HHS) and radiographic evaluation. All patients were followed up until further revision or death (Fig. 4).
Anteroposterior pelvis and cross-table lateral radiographs at last follow-up were analysed for the presence of radiolucent lines and osteolytic lesions around the acetabulum according zones defined by De Lee and Charnley [5]. Osteolysis was defined as a lucent zone devoid of trabecular bone and usually with a sclerotic border not visible on the immediate post-operative radiograph [6, 7]. The acetabular component was considered to be loose if there was migration of >3 mm in any direction over time or a circumferential radiolucent line. Heterotopic ossification was graded according to [8]. The acetabular ARA-scoring method, from poor (1 point) to excellent (6 points), was used as a radiographic evaluation of the status of the cup [9]. Cup position was evaluated by comparing the immediate post-operative radiograph with the last follow-up radiograph using Imitri Software (v 1.2) and acetabular inclination was measured using the transischial line as reference (Fig. 5).
Results
Regarding implant survivorship, all 263 hips (244 patients) in the study were followed up; 105 patients had died from unrelated causes without revision and were excluded from the survival analysis. All remaining 139 patients were reviewed. Of the total 244 patients, 73 were male (30 %) and 171 were female (70 %) with the mean age of 71, ranging from 36 to 92 years on initial surgery (Fig. 4). The mean body mass index was 30 kg/m2, ranging from 19 to 56. The median ASA score was 2; and 3 % of patients were smokers. All patients were followed up with minimum ten years clinical and radiological review, the mean follow up was 11.5 years, ranging from ten to 13.5 years (Fig. 6). The mean pre-operative Harris hip score was 48 (S.D. 16) and the average post-operative score was 82 (S.D. 12), which is associated with good outcome (Table 1).
The indications for primary total hip arthroplasty (n = 188) in our cohort were osteoarthritis (78 %), inflammatory arthritis (15 %), AVN (5 %) and trauma 2 %. The most common cup size used was 60 mm in males and 54 mm in females. Twenty hips were classified as complex primary for hip dysplasia related pathology, for which the most common cup size was 54 (bimodal, secondary mode at 66). The indications for revision total hip arthroplasty (n = 75) in our cohort were aseptic loosening (22 %), wear (38 %), infection (12 %) and periprosthetic fractures (28 %). The most common cup size used for revisions was 58 mm (bimodal, secondary mode at 68). The polyethylene inserts were used according to cup and head size, the majority, 212, articulated with a size 28 mm head size, 50 used a size 32 mm head, and in one revision case, a size 22.5 mm articulate surface was used. All liners used were GUR 1050 ultra high molecular weight polyethylene (non-crosslink) with a 10° lip (raised wall). A combination of femoral implants was used, which included cement tapered design in 70 % of cases and un-cemented stem in 30 % of cases. In revisions, un-cemented stems were used in all cases. Radiological evaluation showed an excellent ARA-score in all but five patients who progressed to revision surgery due to septic and aseptic loosening. Cancellous bone densification was seen in 90 % of the cases in zone 1 and in 65 % of the cases in zone 3. None of the cups showed osteolysis and all cup positions remained unchanged at final follow up.
A total of 13 patients had a grade II complication according to the classification system of [10], implying recovery after re-operation. No patients had grades I, III, IV or V complications. 13 hips returned to theatre for a further surgical intervention for any reason. Of which, four were for dislocation, three were for two stage revision due to deep infections, one was for periprosthetic fractures of acetabulum, one was for periprosthetic fractures of femur, one was failure of the femoral stem, two were for wear and one for aseptic loosening. Out of these 13 hips, ten had the cup revised and 11 had the stem revised (Table 2) (Figs. 7 and 8).
According to life table analysis, the 13 years cumulative implant survival was 91.2 %, the risk of implant revision was 8.8 % at 13 years. The Kaplan Meier survivorship analysis of cumulative failure showed an implant survival rate of 95.2 % at ten years for revision for any reason and 99.4 % for aseptic loosening (Fig. 9).
Kaplan Meier survivorship analysis showed implant survival rate of 95.1 % (95% CI 92.2–98.0) at ten years for revision for any reason (grey line) and 99.4 % (95% CI 100–98.3) for aseptic loosening (grey line). At 13 years, the implant survival rate was 93.7 % (95 % CI 90.2–97.1) with revision for any reason (black line) and 99.4 % (95 % CI 100–98.3) for aseptic loosening (black line)
Discussion
Our study is the first to show the findings at a minimum follow-up of ten years for the Atlas IIIp acetabular component with 100 % follow up in an independent centre in the UK. Our results are superior compared to the inventor’s series reported by Philippe et al. with a survival rate of 92.3 % at ten years for revision for any reason and 95.2 % at ten year for aseptic loosening with 126 patients [2]. Epinette et al. reported similar results with this implant. In 151 patients, ten year survival rate was 96.95 % ± 0.0269 with revision for any reason and for aseptic loosening the ten year survival rate was 99.18 % ± 0.0159 [1], which are similar to our series.
Uncemented acetabular components are becoming more widely used all over the world; there are different designs and theories for these components being associated with good outcomes. There are many reports suggesting that hard metal backed uncemented acetabular components have good long-term results. Kim et al. reported Kaplan-Meier survival rates of an uncemented acetabular component (Duraloc, DePuy, Warsaw) in 79 patients (110 hips) at ten years of 93.6 % [7]. The Allofit cup (Zimmer, Warsaw) reported the Kaplan-Meier survival rate at 11 year to be 98 % (95 % CI: 92.2–99.2) [11, 12]. However, there has been little published literature on flexible metal backed uncemented acetabular components. Our result of 99.4 % (95 % CI 100–98.3) Kaplan-Meier survival rates at ten years is comparable to the hard metal uncemented acetabular components.
The Atlas IIIp is designed for acetabulum press-fit fixation and its thin elastic shell has lower Young’s modulus more in keeping with bone compared to other cementless acetabular systems. This may improve the load transfer to acetabulum bone and prevent stress shielding, hence preventing aseptic loosening [13–15]. The GUR 1050 ultra high molecular weight polyethylene liner (not highly cross-linked) undergoes creep with contained load and press fit fixation, which produces an interlocking surface with the rough titanium shell and prevents back side wear [15]. Owing to the thin shell design of this acetabulum system with only 2.5 mm thickness, the polyethylene thickness can be 5–10 mm thicker compared to other hard shell cementless designs. The thickness of the polyethylene is inversely proportional to wear, which will affect the survival and longevity of the implant [16]. Oonishi et al. demonstrated that a 2 mm decrease of the thickness in the polyethylene can lead to twice the wear rate [17]. Therefore, the increase in thickness of the polyethylene in the Atlas IIIp system would be in favor of reducing volumetric and linear wear. Two cases in this study were revised due to polyethylene wear from the articular interface, but no back side wear was found in the poly-shell interface. Our findings are similar to the microscopic study by Dambreville, noting the absence of any alteration in the machining grooves on the metal-poly interface on the Atlas IIIp explants after more than ten years of use [3]. Published reports suggest that conventional polyethylene liner (GUR 1050) with more than ten years of follow-up have consistently shown a marked decline in survivorship after ten years [7, 15, 18–20]. The low rate of aseptic loosening and implant revision (6.37 %) at 13 years with the Atlas IIIp cup in our series could be due to the combination of flexible design and increased thickness of the polyethylene liners compared to the traditional hard metal back design.
There are some limitations in this study. Firstly, acetabular cup position and orientation were analysed on radiographs using special software. Computer tomography measurements are considered gold standard when accurate measurements are desired. However, the routine use of CT scans has its limitations in terms of cost, practicality and radiation effects. A study by Craiovan et al. has demonstrated that single x-ray 2D/3D reconstruction technique strongly correlated with CT image-processing protocols for both cup inclination and anteversion [21]. Secondly, surgery was performed by the senior author or by trainees under his direct supervision, which could introduce variable experience of the operative surgeon to the study. Thirdly, different types of femoral stems were used in combination with this cup, which could introduce another variable. On the other hand, the implant longevity and the clinical results in our series for both primary and revision with combination of femoral stem and surgeon experience was good, this demonstrates the versatility and ease of use of this cup.
Conclusion
The long-term results of the cementless acetabulum depend on the mode of primary and secondary fixation, implant design, material quality, thickness of the polyethylene and quality of the bearing surface. Our experience from an independent centre in the UK with the Atlas IIIp elastic cementless acetabular component is good and its long-term survival rate is consistent and acceptable.
References
Dambreville A (2004) Minimum ten years follow-up of the hydroxyapatite-coated ATLAS cup. In: Epinette J-A, Manley MT (eds) Fifteen years of clinical experience with hydroxyapatite coatings in joint arthroplasty. Springer, Paris
Philippe M, Ameil M (2007) Survival analysis at 10 years of a cohort of 297 atlas total hip prostheses. Eur J Orthop Surg Traumatol 17(6):573–578. doi:10.1007/s00590-007-0236-y
Dambreville A (2001) Assessing the stability of metal back acetabular inserts. A microscopic study of explants. Eur J Orthop Surg Traumatol 11(4):213–218. doi:10.1007/BF01686891
Pakvis D, Janssen D, Verdonschot N (2010) Acetabular stress shielding—a finite element analysis of a cemented, a cementless rigid and a cementless elastic socket. In: Deutscher Kongress für Orthopädie und Unfallchirurgie (DKOU), 21/10/2010 2010. doi: 10.3205/10dkou105
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Zenz P, Stiehl JB, Knechtel H, Titzer-Hochmaier G, Schwagerl W (2009) Ten-year follow-up of the non-porous Allofit cementless acetabular component. J Bone Joint Surg (Br) 91(11):1443–1447. doi:10.1302/0301-620X.91B11.22368
Kim YH, Kim JS, Park JW, Joo JH (2012) Periacetabular osteolysis is the problem in contemporary total hip arthroplasty in young patients. J Arthroplasty 27(1):74–81. doi:10.1016/j.arth.2011.03.022
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55(8):1629–1632
Epinette JA (1999) Radiographic assessment of cementless hip prostheses: the “ARA” scoring system. Eur J Orthop Surg Traumatol 9(2):91–94. doi:10.1007/bf01695736
Goslings JC, Gouma DJ (2008) What is a surgical complication? World J Surg 32(6):952. doi:10.1007/s00268-008-9563-3
Streit MR, Schroder K, Korber M, Merle C, Gotterbarm T, Ewerbeck V, Aldinger PR (2012) High survival in young patients using a second generation uncemented total hip replacement. Int Orthop 36(6):1129–1136. doi:10.1007/s00264-011-1399-z
Streit MR, Weiss S, Andreas F, Bruckner T, Walker T, Kretzer JP, Ewerbeck V, Merle C (2014) 10-year results of the uncemented Allofit press-fit cup in young patients. Acta Orthop 85(4):368–374. doi:10.3109/17453674.2014.925351
Ries MD, Harbaugh M, Shea J, Lambert R (1997) Effect of cementless acetabular cup geometry on strain distribution and press-fit stability. J Arthroplasty 12(2):207–212. doi:10.1016/S0883-5403(97)90068-1
Charnley J (1972) The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 54(1):61–76
Hallan G, Dybvik E, Furnes O, Havelin LI (2010) Metal-backed acetabular components with conventional polyethylene: a review of 9113 primary components with a follow-up of 20 years. J Bone Joint Surg (Br) 92(2):196–201. doi:10.1302/0301-620X.92B2.22179
Lee PC, Shih CH, Chen WJ, Tu YK, Tai CL (1999) Early polyethylene wear and osteolysis in cementless total hip arthroplasty: the influence of femoral head size and polyethylene thickness. J Arthroplasty 14(8):976–981
Oonishi H, Iwaki H, Kin N, Kushitani S, Murata N, Wakitani S, Imoto K (1998) The effects of polyethylene cup thickness on wear of total hip prostheses. J Mater Sci Mater Med 9(8):475–478
Duffy GP, Prpa B, Rowland CM, Berry DJ (2004) Primary uncemented Harris-Galante acetabular components in patients 50 years old or younger: results at 10 to 12 years. Clin Orthop Relat Res 427:157–161
Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P (2006) Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop 77(1):57–70. doi:10.1080/17453670610045704
Utting MR, Raghuvanshi M, Amirfeyz R, Blom AW, Learmonth ID, Bannister GC (2008) The Harris-Galante porous-coated, hemispherical, polyethylene-lined acetabular component in patients under 50 years of age: a 12- to 16-year review. J Bone Joint Surg (Br) 90(11):1422–1427. doi:10.1302/0301-620X.90B11.20892
Craiovan B, Renkawitz T, Weber M, Grifka J, Nolte L, Zheng G (2014) Is the acetabular cup orientation after total hip arthroplasty on a two dimension or three dimension model accurate? Int Orthop 38(10):2009–2015. doi:10.1007/s00264-014-2336-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Lee, P.Y.F., Rachala, M., Teoh, K.H. et al. Long-term results with the Atlas IIIp elastic cementless acetabular component in total hip replacement. International Orthopaedics (SICOT) 40, 1835–1842 (2016). https://doi.org/10.1007/s00264-015-3088-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3088-9