Abstract
Purpose
In vitro studies have shown promising results for balloon-guided inflation tibioplasty. It was our hypothesis that this technique may be safe and effective for use in depressed lateral tibial plateau fracture.
Methods
We performed a prospective study of all patients suffering from a depressed lateral tibial plateau fracture, managed in our institution with inflation tibioplasty and a resorbable calcium phosphate bone substitute injection, between January 2012 and December 2013. Twenty patients, mean age 54.3 ± 12. 8 years, suffering from a depressed lateral tibial plateau fracture (Schatzker type II and III) were included. We then aimed to evaluate at a minimum follow-up of one year: (1) the rate of complications, (2) the clinical outcome (Knee Injury and Osteoarthritis Outcome (KOO) and 12-Item Short Form Health Survey (SF-12) scores); and (3) the radiographic outcome (evaluated by CT-scan).
Results
No peri-operative complications occurred. In one patient, calcium phosphate substitute was found in the infrapatellar fat pad on post-operative radiography with no clinical or radiographic consequences at one year. At one year after surgery, the KOO subscores were: Pain 80 (range 64—93), other symptoms 81.3 (69–93), daily living activities 81.9 (46–99), sport 65.83 (20–100), and quality of life 67.04 (31–100). The SF-12 activity component was 40.4 (28.6—52.2) and SF-12 mental component 47.71 (28 – 67.1). The mean depressed step-off of the lateral joint decreased from 10.7 ± 4.8 mm pre-operatively to 2.7 ± 1.7 mm post-operatively (p < 0.0001).
Conclusion
Our observations suggest that the use of balloon-guided inflation tibioplasty with injection of a resorbable bone substitute is safe, and results in a high rate of anatomic reduction and good clinical outcomes in patients with depressed tibial plateau fractures.
Level of Evidence: Therapeutic Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
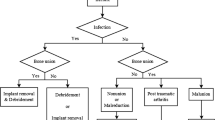
Tibial plateau fractures are complex intra-articular and metaphyseal lesions, accounting for 5–8 % of all fractures of the lower leg [1]. Ideal management of tibial plateau fracture must provide (1) anatomical restoration of joint surface to prevent cartilage damage and post-traumatic arthritis [2], and (2) rigid fixation to allow early post-operative rehabilitation and prevent stiffness [3, 4].
Several studies have described balloon-guided inflation tibioplasty techniques using polymethyl methacrylate (PMMA) cement as a graft following the initial vertebroplasty procedure [5–9]. This technique allows minimally invasive fracture reduction with more accurate control of bone elevation and broader reduction than classic bone tamps [6]. However, current literature describing a tibioplasty technique contains only cadaveric studies, case reports and technical notes [5, 7]. A single observational retrospective study has been published, which investigates only the potential complications of this procedure [8]. Even though a study protocol for a randomized control trial has been published, no data concerning post-operative outcomes of this technique are available [9].
It was our hypothesis that depressed tibial plateau fractures treated by balloon-guided inflation tibioplasty and calcium phosphate bone substitute (CPBS) as subchondral graft can be safe and provide optimal post-operative outcomes.
Our objectives were to evaluate at a minimum follow-up of 1 year after surgery: (1) The safety of the technique and its potential adverse events; (2) clinical results using the Knee Injury and Osteoarthritis Outcome Score (KOOS) [10] and the 12-Item Short Form Health Survey (SF-12) [11]; and (3) radiological results using CT-scan evaluation (Heiney and Redfern score) [12].
Methods
Between January 2012 and December 2013, 56 patients with tibial plateau fractures were admitted to our emergency department. For this study, inclusion criteria were: patients aged between 18 and 85 years presenting with an acute, closed, isolated depression (Schatzker type III, AO/OTA type 41.B2) or a lateral split plus depression (Schatzker type II, AO/OTA type 41.B3) tibial plateau fracture. The exclusion criteria were: Posteriorly displaced fractures, skeletally immature patients, pathological fractures, significant pre-existing degenerative joint disease, severe systemic illness (active cancer, chemotherapy, renal failure or other co-morbidities that contraindicated surgery), or a neurological condition that would interfere with rehabilitation. Pre-operatively after clinical evaluation, all of the patients underwent both knee X-rays and CT scans to evaluate fracture depression and plan the optimal position of the intra-operative inflatable device.
We prospectively identified 20 patients meeting the inclusion/exclusion criteria (11 males, nine females; mean age 54.37 ± 12.94 years). In ten cases fractures were related to sports injuries (50 %), in nine cases to vehicle-related collisions (45 %), and an accidental fall was described by the remaining patient (5 %). Eight patients suffered from Schatzker type III and 12 from Schatzker type II fractures. All patients were stable during varus/valgus and Lachman clinical testing. The mean time to surgery was 5.3 ± 4.3 days after trauma.
The same surgical protocol was used for every patient evaluated in this study. Patients were placed in the supine position with the knee flexed at 80° without tourniquet. A fluoroscopic device allowed identification of the optimal entry point (defined on pre-operative CT scan) for inflatable bone tamps (Kyphon®, Medtronic, Minneapolis, MN, USA). A working cannula was inserted into the metaphyseal bone in a medial-lateral direction 4–5 mm under the main depressed area. As described by Messina et al. [13], 2 mm rafting Kirshnser-wires were inserted below the desired balloon position. The role of these k-wires is to direct inflatable bone tamp forces towards the depressed zone (Fig. 1). For Schatzker type II fractures (split and depression) a peri-articular clamp was used to prevent displacement of the fragment during balloon inflation. After having the balloon pushed forward through the cannula, we verified the correct position, the shape and the integrity of the balloon, and the gradual reduction of the fracture under fluoroscopy view. The maximum pressure did not go beyond 250 PSI as described by Broome et al. [5]. After balloon deflation, injectable calcium phosphate bone substitute (GRAFTYS® QUICKSET, Aix en Provence, France) was injected in the void left by the balloon. A mean of 10 cc per patient was injected to fill the bone void. The fracture was then fixed with two percutaneous partially threaded cannulated screws (Fig. 2).
No brace was applied. The post-operative rehabilitation protocol consisted of immediate active full range of motion and six weeks of non-weight bearing. Post-operative complications such as cement overflow into the soft tissues or the knee joint, wound dehiscence and infection, were recorded.
Clinical and radiological assessment
Patients were evaluated post-operatively by the same examiner: physical examination, KOOS [10] and SF-12 evaluation [11] , range of motion, and delay to return to professional were assessed at three, six, nine, and 12 months.
The radiological evaluation included standard knee X-rays (after surgery, then 3, 6, 9, and 12 months post surgery) and CT scan (pre-operatively, post-operatively, and 1 year after surgery) with coronal and sagittal views.
Fracture depression and residual post-operative step-off were measured on CT scans. We used the Heiney and Redfern score to analyze the quality of the reduction [12]. Coronal reformatted CT images allowed identification of the perpendicular line to the longitudinal tibial axis that passes from the highest point of the unaffected tibial condyle. This line defined the level of the pre-traumatic tibial plateau [12]. From this line we measured the millimetric gap of the tibial plateau fracture and the residual post-operative step off. Appendix 1 presents details of the Heiney and Redfern scoring system.
Statistical analysis
The normality of the distribution of the parameters was tested using the Kolmogoroff-Smirnoff test; parametric tests were used to compare normally distributed parameters (paired Student-t test: preoperative/postoperative radiological outcomes). All statistical analysis assumed a 2-tailed test; PASW Statistics version 20 (SPSS, IBM Inc., Chicago, IL, USA) was used. The threshold for statistical significance was set at p < 0.05.
Results
No patient was lost to follow-up at a mean follow-up of 18 months.
Safety of the technique
An intra-articular diffusion of calcium phosphate bone substitute was observed in one patient and registered as a complication. Post-operatively we observed the presence of a bone substitute mass (max measurement: 17.05 mm) into the infrapatellar fat pad (Fig. 3). As the patient did not complain, and showed a good clinical status (SF-12 45/51, mean KOOS 79) with a normal range of motion and radiographic outcomes (H–R score: 11) at last follow-up (19 months), no treatment was performed. No other intra-operative or post-operative complications occurred during follow-up.
Clinical outcomes
At the last follow-up the mean SF-12 activity component score was 40.4 ± 10.1 (28.6—52.2 points) and the mean SF-12 mental component score was 47.71 ± 12.3 (28 – 67.1 points). KOOS at last follow-up were: pain 80 ± 12.2 (64—93 points), symptoms 81.3 ± 10.1 (69—93 points), daily living activities 81.9 ± 12.6 (46—99 points), sports and recreational activities 65.83 ± 18.3 (range 20—100 points), and quality of life 67 ± 16.7 (31—100 points) (Fig. 4).
The range of motion at last-follow-up was mean flexion 111 ± 18 (87—130°) and mean extension 2 ± 2 (0—6°). All active patients returned to their previous employment with a mean delay of four ± three months (1—7 months) after surgery.
Radiological outcomes
At last follow-up all 20patients had healed their fractures with no loss of reduction. None of the patients exhibited lysis of the cancellous bone/cement interface; moreover we observed a resorption of the CPBS in all patients (Fig. 4).
The mean depressed step-off of the lateral joint decreased from 10.75 ± 7.2 mm (4.11–19.86 mm) pre-operatively to 2.71 ± 1.71 mm (0.63–5.7 mm) post-operatively (p < 0.0001). We obtained a ≤ 2 mm step-off in 75 % of patients and a >2–5 mm step-off in 95 % of patients with only one patiens having an articular step-off > 5 mm (5.7 mm).
These radiological results were stable until the last follow-up as at one year after surgery we found a mean depressed step-off of the lateral joint of 2.9 ± 1.64 mm (p = 0.3)
Finally, CT-scan evaluation of the treatment showed good results in all patients with mean a Heiney and Redfern score of 12.7 ± 0.97 a at minimum follow-up of one year. No evidence of post-traumatic osteoarthritis was observed at a maximum follow-up of two years.
Discussion
Balloon-guided inflation tibioplasty techniques allow minimally invasive fracture reduction with more accurate control of bone elevation and broader reduction than classic bone tamps [5]. As the current literature contains only cadaveric studies, case reports, and technical notes [5–7], we aimed to conduct a study to evaluate the safety and efficacy of this new technique.
Our first aim was to evaluate the safety of this procedure. We only recorded one specific complication in our series, calcium phosphate bone substitute was found intra-articularly in one patient. Mauffrey et al. [8] described a comparable rate for this complication in their study; conversely, they described a very high rate (13 patients, 65 %) of complications [8]. Six cases were balloon bursts and four were failures to elevate the depressed articular fragment. They, however, described bursting only when the balloon was inflated beyond 400-PSI. In this preliminary study we scrupulously followed Broome et al.’s [5] recommendation and instead changed the rafting wires position rather than inflating the balloon beyond 250 PSI. Finally, Mauffrey et al. [8] described reduction failures in four patients undergoing surgery more than two weeks after trauma. All of our patients were operated on at least ten days after trauma (average 5 days). Those differences may explain why we did not notice any balloon bursts or reduction failures in our series.
Knee stiffness, infections, thromboembolic complications, and complex regional disease, widely related to traditional tibial plateau fracture reductions and fixation techniques, were not observed in this series [14, 15]. Open Reduction Internal Fixation (ORIF) supposes soft tissue dissection that may predispose to complications such infections or wound dehiscence. Infection rates are reported in a range of 3–32 % with open reduction techniques, with a higher prevalence for males smokers, with poor ASA status and/or respiratory disease and/or bicondylar fractures [16, 17]. Minimally invasive procedures such as Arthroscopic Reduction and Internal Fixation (ARIF) or balloon-guided inflation tibioplasty could reduce this type of complication; however, no prospective randomized controlled trial compared the complications and outcomes of ARIF versus minimally invasive procedures. In a systematic review of ARIF for tibial plateau fracture, Chen et al. [18] reported a few cases of severe complications such as deep venous thrombosis or deep infection. Thus, two cases of leg compartment syndrome are described after ARIF [18, 19]. The authors hypothesized that the elevated intra-articular pressure in a context of fracture and capsular damage could lead to fluid extravasation into the calf.
Our study confirms that balloon-guided inflation tibioplasty and subchondral CPBS provide good clinical outcomes, as our results are comparable with those in the literature concerning Schatzker type II and III fractures. Siegler et al. [14] reported similar KOOS using percutaneous/arthroscopic fixation. Other studies used Hospital for Special Surgery (HSS) or the Rasmussen score to evaluate clinical outcomes: Dall’Oca et al. [20] found similar clinical results for patients treated for Schatzker type II and III fracture using arthroscopic (33 patients) or open reduction (23 patients). This series presented optimal outcomes in term of HSS and clinical Rasmussen scores, and the author emphasized the role of arthroscopic evaluation regarding the high number of meniscal co-morbidities [20].
Finally, our radiological outcomes are promising as we obtained a ≤ 2 mm step-off in 75 % of patients and a >2–5 mm step-off in 95 % of patients with only one patient with an articular step-off > 5 mm. Current reduction techniques involve elevating any depressed segments with a metal tamp or elevator and filling the resulting void with bone graft or other desired material [21]. These reduction techniques are often imprecise and risky [21–23]. Thus, for comminuted fractures, such as Schatzker type II and III, anatomic restoration of the articular surface is virtually impossible to achieve. In actual clinical studies concerning tibial plateau fractures, articular reduction of the depressed surface remains highly variable, as some authors accepted residual step-off of <3 mm and others accepted up to 10 mm [21–23]. We selected step-off values of <2 mm as optimal and 2–5 mm as acceptable based on the Lefkoe et al. [24] study demonstrating that 2-mm step-off defects can be replaced by repair tissue and healed with hyaline cartilage. However, cartilage healing is unpredictable; Chang et al. [25] performed second-look arthroscopic evaluation in 20 Schatzker type II fractures. Chondromalacia was seen for 11 patients (68 %) who had a step-off smaller than 2 mm at least 18 months after surgery; when articular step-off was > 2 mm, chondropathy grade III or worse was found for each of the patients (four patients) [25].
Some limitations to this study should be acknowledged. First, there was no control group with which to compare our results. The goal of our study was, however, not to compare but only to describe and evaluate a new technique introduced in our department. Second, the number of patients included in this study was small. The inclusion criteria for this study were, however, strict, focusing on tibial fracture Schatzker type II and III, and this continuous series reflects the number of patients operated on in a single year in a level one trauma center. The duration of follow-up in our protocol allowed us to register intra-operative and early post-operative complications; however, we were not able to provide data concerning midterm complications and failures such as a reduction loss or onset of arthritis. In addition, our study was not aimed at analyzing the cost-effectiveness of this new technique, only safety and efficacy.
Despite those limitations this series is to our knowledge the first to describe the clinical and radiological results of tibial plateau fractures treated using balloon tibioplasty and CPBS as a bone substitute. We chose to use CPBS in our study based on actual literature evidence suggesting that autologous bone graft in conventionally treated plateau fractures is associated with inferior results [21]. Simpson et al. [21] described in their comparative study that patients treated with the calcium phosphate cement had a shorter operation time, reduced surgical exposure, and avoided morbidity associated with the harvested site. Moreover, they described better maintenance of articular reduction at one year follow-up for patients grafted with calcium phosphate cement than autologous bone (23 % vs. 62 % loss of reduction). As described by Hannouche et al. [26], the anterolateral approach to lateral plateau fractures is harmful to epiphyseal vascularization and thus compromises bone healing. As we do believe that maintenance of articular reduction is strongly related to soft-tissue and vascularization sparing since the introduction of balloon tibioplasty with CPBS augmentation, we only used percutaneous screws for Schatzker type II and III fracture fixations.
Conclusion
Our observations suggest that balloon-guided inflation tibioplasty is a safe technique that will result in a high rate of anatomic reduction and good clinical outcomes in patients with depressed lateral tibial plateau fractures. However further comparatives studies with a higher number of patients and longer follow-up are needed to confirm our short-term data.
References
Petersen W, Zantop T, Raschke M (2006) Fracture of the tibial head. Unfallchirurg 109(3):219–232
Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P (2010) Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop 34(4):565–570
Dang A, Kim H (2009) Chondrocyte apoptosis after simulated intraarticular fracture: a comparison of histologic detection methods. Clin Orthop Relat Res 467(7):1877–1884
Rademakers MV, Kerkhoffs GMMJ, Sierevelt IN, Raaymakers ELFB, Marti RK (2007) Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma 21(1):5–10
Broome B, Mauffrey C, Statton J, Voor M, Seligson D (2012) Inflation osteoplasty: in vitro evaluation of a new technique for reducing depressed intra-articular fractures of the tibial plateau and distal radius. J Orthop Traumatol 13(2):89–95
Pizanis A, Garcia P, Pohlemann T, Burkhardt M (2012) Balloon tibioplasty: a useful tool for reduction of tibial plateau depression fractures. J Orthop Trauma 26(7):e88–e93
Ahrens P, Sandmann G, Bauer J, König B, Martetschläger F, Müller D, Siebenlist S, Kirchhoff C, Neumaier M, Biberthaler P, Stöckle U, Freude T (2012) Balloon osteoplasty—a new technique for reduction and stabilisation of impression fractures in the tibial plateau: a cadaver study and first clinical application. Int Orthop 36(9):1937–1940
Mauffrey C, Fader R, Hammerberg EM, Hak D, Stahel P (2013) Incidence and pattern of technical complications in balloon-guided osteoplasty for depressed tibial plateau fractures: a pilot study in 20 consecutive patients. Patient Saf Surg 7(1):8–8
Jordan R, Hao J, Fader R, Gibula D, Mauffrey C (2013) Study protocol: trial of inflation osteoplasty in the management of tibial plateau fractures. Eur J Orthop Surg Traumatol 24:647
Ornetti P, Parratte S, Gossec L, Tavernier C, Argenson JN, Roos EM, Guillemin F, Maillefert JF (2008) Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthr Cartil 16(4):423–428
Ware J, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Heiney J, Redfern R, Wanjiku S (2013) Subjective and novel objective radiographic evaluation of inflatable bone tamp treatment of articular calcaneus, tibial plateau, tibial pilon and distal radius fractures. Injury 44(8):1127–1134
Messina M, Herbert B, Mauffrey C (2013) The use of arthroscopy to assist reduction of depressed tibial plateau fractures. Curr Orthop Pract 24(2):160–164. doi:10.1097/BCO.0b013e318286d227
Siegler J, Galissier B, Marcheix PS, Charissoux JL, Mabit C, Arnaud JP (2011) Percutaneous fixation of tibial plateau fractures under arthroscopy: a medium term perspective. Orthop Traumatol Surg Res 97(1):44–50
Biggi F, Di Fabio S, D’Antimo C, Trevisani S (2010) Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury 41(11):1178–1182
Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23(2):149–154
Basques BA, Webb ML, Bohl DD, Golinvaux NS, Grauer JN (2015) Adverse events, length of stay, and readmission after surgery for tibial plateau fractures. J Orthop Trauma 29(3):e121–126
Chen X-Z, Liu C-G, Chen Y, Wang L-Q, Zhu Q-Z, Lin P (2014) Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy 31(1):143–153
Belanger M, Fadale P (1997) Compartment syndrome of the leg after arthroscopic examination of a tibial plateau fracture. Case report and review of the literature. Arthroscopy 13(5):646–651
Dall’oca C, Maluta T, Lavini F, Bondi M, Micheloni GM, Bartolozzi P (2012) Tibial plateau fractures: compared outcomes between ARIF and ORIF. Strateg Trauma Limb Reconstr 7(3):163–175
Simpson D, Keating JF (2004) Outcome of tibial plateau fractures managed with calcium phosphate cement. Injury 35(9):913–918
Weigel D, Marsh JL (2002) High-energy fractures of the tibial plateau. Knee function after longer follow-up. JBJS J Bone Jt Surg 84-A(9):1541–1551
Lachiewicz PF, Funcik T (1990) Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res 259:210–215
Lefkoe TP, Walsh WR, Anastasatos J, Ehrlich MG, Barrach HJ (1995) Remodeling of articular step-offs. Is osteoarthrosis dependent on defect size? Clin Orthop Relat Res 314:253–265
Chang E-C, Lee J-S, Jung H-S (2014) Second-look arthroscopy after surgical treatment of Schatzker type II plateau fractures through the lateral submeniscal approach. Arch Orthop Trauma Surg 134(4):495–499
Hannouche D, Duparc F, Beaufils P (2006) The arterial vascularization of the lateral tibial condyle: anatomy and surgical applications. Surg Radiol Anat 28(1):38–45
The investigations were performed at St. Marguerite Hospital, Aix-Marseille University, Marseille, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Ollivier, M., Turati, M., Munier, M. et al. Balloon tibioplasty for reduction of depressed tibial plateau fractures: Preliminary radiographic and clinical results. International Orthopaedics (SICOT) 40, 1961–1966 (2016). https://doi.org/10.1007/s00264-015-3047-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3047-5