Abstract
Purpose
Revision surgery for failed unicompartmental knee arthroplasty (UKA) with bone loss is challenging. Several options are available including cement augmentation, metal augmentation, and bone grafting. The aim of the present study was to describe a surgical technique for lateral tibial plateau autografting and report mid-term outcomes.
Methods
Eleven consecutive patients (median age 69.5 years) affected by posteromedial tibial plateau collapse after medial UKA were enrolled in the present study. The delay between UKA and revision surgery was 21 months (range 15–36 months). All patients were revised with a cemented posterior-stabilized implant, with a tibial stem. Medial tibial plateau bone loss was treated with an autologous lateral tibial plateau bone graft secured with two absorbable screws. All patients were evaluated with the Oxford Knee Score (OKS), visual analogue scale for pain (VAS), and complete radiographic evaluation.
Results
At a median follow-up of 60 months (range 36–84 months), the OKS improved from 21.5 (range 16–26) to 34.5 (range 30–40) (p < 0.01) and the median VAS score improved from 8.0 (range 5–9) to 5.5 (range 3–7) (p < 0.01). No intraoperative complications were recorded. Partial reabsorption of the graft was observed in two cases at final follow-up.
Conclusion
Lateral tibial plateau bone autograft is an alternative to metal wedge or cement augments in the treatment of medial plateau collapse after UKA. Primary fixation of the tibial plateau autograft can be achieved with absorbable screws and a tibial-stemmed implant. Further comparative studies with a larger series may be helpful to draw definitive conclusions.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
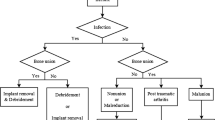
Unicompartmental knee arthroplasty (UKA) has emerged in the last decade as an alternative to total knee arthroplasty (TKA) and high tibial osteotomy (HTO) in the treatment of isolated medial compartment osteoarthritis [11]. Unicompartmental knee arthroplasty should not be considered a temporary solution before TKA, because clinical outcomes are not equal to results of a primary knee arthroplasty when revised [20]. The most common cause for a revision of a UKA to TKA is loosening. Loosening accounted for half of all revisions that were performed in the New Zealand Joint Registry [13]. Since aseptic loosening is often asymptomatic initially, it tends to be associated with progressive osteolysis and leads to bone defects that require advanced surgical management in the revision setting [15]. The presence of extensive bone loss at the time of UKA revision is challenging and may require bone grafting [12, 14, 18], the need for stemmed revision components and metal or tantalum augments, or even the need for custom made implants [1].
It is well established that the integration of metal augments with the sclerotic bone of the medial plateau may be difficult and aseptic loosening of the tibia is the most common cause UKA re-revision [8, 13]. Addressing such bone defects with biologic solutions such as autologous bone graft may be advantageous in terms of biologic integration and economic costs. The aim of the present study was to describe a technique for lateral tibial plateau autograft to address the posteromedial tibial plateau collapse in revision surgery for failed UKA and to report the mid-term outcomes in a consecutive series of patients. It was hypothesized that lateral plateau autografting would result in good clinical outcomes and stable radiographic findings at mid-term follow-up.
Materials and methods
Eleven consecutive patients affected by posteromedial tibial plateau collapse after medial UKA were enrolled in the present retrospective cohort study. Medial plateau collapse was detected on lateral radiographs as an increase in posterior inclination of the tibial plateau. Eight patients were female, and three patients were male. The right knee was involved in seven cases, while the left side was involved in four cases. All patients were revised with the same surgical technique, the same cemented posterior-stabilized implant, and by the same senior surgeon (GC). The index procedure was performed in our department for two cases, while the index procedure was performed at outside facilities in nine cases. The median age at the time of revision surgery was 69.5 years (range 65–71 years). The median delay between UKA and revision TKA was 21 months (15–36 months). The knee flexion was on median 100° (range 89°–112°), and three patients had a flexion contracture of 7° (range 5°–10°). All patients had significant pain and tibial component loosening with posteromedial bone loss that was evident on serial radiographs. Tibial plateau bone loss was detected with conventional radiographic examination including weight-bearing anteroposterior and lateral views. All patients were evaluated with the Oxford Knee Score (OKS) [5] and a visual analogue scale for pain (VAS). All the methods described in this article were approved by the local ethics committee (Health Director of the Villa Betania Hospital in Rome).
Surgical technique
All cases were performed with patients in the supine position with the operative leg in a leg holder in order to keep the knee in deep flexion. The tourniquet was inflated at 350 mmHg just prior to the skin incision. The prior surgical incision was utilized and extended distally to reach the inferior border of the tibial tuberosity and proximally around 4 cm proximal to the superior pole of the patella. Medial capsulotomy was performed with electrocautery. Dissection of the anteromedial capsule was completed to improve joint exposure and to achieve partial medial release. The fat pad was excised, and the patella was everted. Complete circumferential osteophyte removal and patellar denervation was performed in all cases. The femoral notch was released, and both anterior and posterior cruciate ligaments were resected. The lateral meniscus was completely resected to allow complete visualization of the lateral compartment. After scar tissue excision, the tibial and femoral components were assessed for stability. The femoral component was well integrated in all cases, but the tibial tray was grossly loose in all cases. Component removal was carried out with sharp osteotomes taking care to preserve the host bone. Tibial resection was performed first. The same instrumentation and implants (Tornier Inc. Montbonnot Saint Martin. France) were used in all cases. This implant has an intramedullary guide for the tibia that controls the tibial slope. The resection was performed with 0° of tibial slope. An extramedullary jig controls varus–valgus alignment and aligns the tibial cut perpendicular to the mechanical axis and also controls the extent of medial bone resection. The resection of medial plateau was performed flush to the residual bone in order to obtain a flat surface perpendicular to the mechanical axis. The difference in height among the medial side and the lateral side could be easily calculated. In fact, on the lateral side, a preliminary orthogonal resection was completed to just below the cartilage level extending medially below the level of the tibial spine. The bony resection was performed in a standard fashion (like for standard primary TKA) 9 mm below the lateral plateau. Once the posterior aspect of the lateral plateau was released, an autograft of around 8 mm was available. Additional bone chips were obtained from the tibial spine. The autograft was prepared to match the medial plateau (Fig. 1).
The tibial canal was prepared to host a tibial stem. Size and length of the stem were chosen according to the quality of the metaphyseal bone. The preparation of the metaphysis was performed without the graft in place to avoid any risk of graft fracture, whereas the graft was gently prepared with a luer. Once the match was satisfactorily achieved, the autograft was gently impacted to obtain the same height level for the medial and lateral plateau. The graft was then fixed with two 4.5-mm cancellous absorbable poly lactic acid screws with hydroxyapatite coating (Taikron Co Lpt, Japan) (Fig. 2). On the femoral side, distal resection was performed with the aid of an intramedullary cutting guide. The philosophy of this prosthesis is a posterior resection parallel to the plane of the posterior condyles. To achieve this goal and to avoid malrotation, the same thickness of the removed implant must be considered when performing the posterior resection. A double check with the epicondylar axis was also performed. Satisfactory ligament balancing was obtained with a (9 mm) polyethylene insert in all cases. The tibial and femoral components were cemented once the stability and the range of movement (ROM) were assessed and deemed to be satisfactory. The tibial stem was not cemented in any case. The tourniquet was released after cementation was completed. The surgical field was irrigated, and bleeding was controlled. A medium drain was placed and left into the joint for the first 24 h. The capsule was closed with a #2 absorbable suture. The subcutaneous layer and skin were sutured in standard fashion. A compressive dressing was applied to the whole leg and left in place for the first 24 h.
The physical therapy protocol was the same in all patients. Continuous passive motion was initiated from the first post-operative day and then carried on for the first 3 weeks while increasing knee flexion by 5° daily. Isometric strengthening exercises for the quadriceps strengthening were performed from day 1 as well. Weight bearing was not allowed for the first month. Partial weight bearing was encouraged after one month for 15 more days. Complete weight bearing was allowed 45 days after surgery following radiographic review. Pulsed electromagnetic field therapy (Igea spa, Carpi, Italy) was performed in all patients for the first 45 days after surgery.
The duration of follow-up after revision surgery was 60 months (range 36–84 months). OKS and radiographs were obtained at final follow-up, and an additional subjective evaluation was completed asking the following question: “are you very satisfied, satisfied or not satisfied with your functional result?”
Statistical analysis
Statistical analysis of the preoperative and post-operative values was performed using the Wilcoxon signed-rank test: XLSTAT 2009 (G*Power 3.1.0.) setting the alpha value at 0.05.
Results
One patient died 3 years after revision surgery due to natural causes unrelated to the knee replacement. Ten patients were available for both clinical and radiographic evaluation at final follow-up. Tibial plateau bone loss was evaluated radiographically and intraoperatively. A cavitary defect with an intact cortical rim was found in seven cases. In all cases, initial radiographs after UKA revealed an undersized prosthetic tibial tray. The alignment of the tibial component was judged to be correct, with an orientation within 3° to the preoperative joint line in all cases. Serial radiographs demonstrated progressive subsidence of the implant prior to the revision surgery. In the remaining three cases, the defect was segmental with interruption of the cortical rim. In these cases, the sizing of the tibial component was judged to be appropriate. In these cases, the analysis of pre-UKA radiographs revealed that the native posterior tibial slope was not restored. In these circumstances, an insufficient slope may lead to posterior overload during knee flexion with increased risk of tibial tray collapse into the host bone. No intraoperative complications were recorded.
At final follow-up, the knee flexion was on median 110° (range 97°–120°) with one patient having a persistent flexion contracture of 10°. The median OKS improved from 21.5 (range 16–26) to 34.5 (range 30–40) (p < 0.01), and the VAS score improved from 8.0 (range 5–9) to 5.5 (range 3–7) (p < 0.01). Three patients were very satisfied with their functional result and six were satisfied. One patient was not satisfied and reported persistent pain under weight-bearing conditions. Radiographs revealed complete integration of the graft in eight patients, while partial reabsorption of the graft was present in two cases (Fig. 3). The partial graft reabsorption occurred within the first 6 months, however, in both cases, and the reabsorption was neither symptomatic nor progressive.
Discussion
The most important finding of the present study is the reliable surgical technique of lateral plateau autografting for revision of UKA. To our knowledge, this is the first report on a homogenous population of patients affected by tibial plateau collapse after UKA. The same surgical technique of autologous bone graft from the lateral tibial plateau to address medial plateau bone loss as well as the same implant was utilized in all patients.
In the present series, a purely cavitary defect was observed in cases of undersized tibial trays with the posterior aspect sinking into the cancellous bone. Partial involvement of the posterior cortical rim was found in cases of insufficient posterior tibial slope. The bone loss was addressed in all cases with an autograft of the lateral tibial plateau. In fact, the tibial resection, which was performed in the same way as for primary implants, allowed us to harvest an 8–10 mm graft. The primary stability of the graft was secure fixation with two 4.5-mm absorbable screws. To bypass the bone-to-bone interface, a short stem was implanted in all cases and the tibial plateau was cemented as well. The graft was then protected from loading for the first post-operative period, and bone remodelling was stimulated with prolonged pulsed electromagnetic field therapy [19]. Nevertheless, partial reabsorption of the graft was observed in two cases, although it was not clinically symptomatic. No intraoperative complications were reported.
Patients were generally satisfied with their functional result with a significant and stable improvement of Oxford and VAS scores even in the two cases that developed a partial reabsorption of the graft. Conversely, the improvement of flexion was not significant. Most of the patients had satisfactory preoperative flexion, and this could be the consequence of the pathologic anatomy. In fact, the posterior involvement of the tibial plateau may have not negatively influenced the preoperative flexion. These positive outcomes may be related to the very strict indications, with limited bone loss exclusively on the tibial side.
Revision surgery after failed medial UKA may be technically demanding when bone loss or ligament insufficiency are present [6] leading to outcomes that are generally inferior to primary surgery [20]. The presence of bone loss must be carefully evaluated when dealing with revision of a UKA. It can be contained or segmental. In medial UKA’s, bone loss is often attributable to mechanical loosening of the implant. It may be the consequence of technical errors such as excessive varus inclination of the joint line, insufficient posterior tibial slope, or a downsized tibial tray. Finally, additional bone loss may be the result of polyethylene wear [3] or it may be caused at the time of tibial component removal. Different strategies in dealing with bony defects have been described including metal wedges, cement, and allogenic or autologous bone grafting [2, 4, 7, 9, 10, 17, 18, 21]. According to the literature, the use of long stems and “wedges” is necessary in up to 69 % of the UKA revisions [13, 22]. Currently, no option has been demonstrated to be superior to the others and all these options have shown potential disadvantages. Padgett et al. [12] reported a higher complication rate when cement alone was used to fill the bone defect. Metal wedges are the most common and easiest way to address medial plateau bone loss. Unfortunately, bone sclerosis at the tibial metaphysis can be a problem when metal augments are applied. The excessive stiffness may decrease fixation properties of the implant leading to subsequent loosening of the revision prosthesis [8, 13].
Allografting or autografting may be advantageous in preserving the host bone stock and reproducing the same elasticity of the metaphyseal bone allowing for a physiologic remodelling of the metaphysis. Tibial autograft has several additional advantages. First of all, it is easily accessible during surgery with the possibility of perfect match with the host tibial metaphysis. In addition, autografts offer economic benefits over traditional metal wedges, allografts, or custom implants with the only cost being represented by the two absorbable screws. This is a major issue especially in countries or hospital systems where the budget for revision procedures is limited. However, some doubts may arise regarding the stability of initial fixation of the graft and late integration. Nevertheless, the primary stability of the graft can be increased with absorbable or metallic screws and bypassing the bone-to-bone interface with tibial stems. The integration can be stimulated with external devices such as magnetotherapy or pulsed electromagnetic field therapy [19]. In any case, it is important to highlight the importance of periodic follow-up examination after UKA and the revision surgery. Posterior tibial collapse occurring after UKA may be easily detected in the early phase with radiographic follow-up in symptomatic patients. This is crucial to avoid extensive bone loss that can increase the complexity of revision surgery and affect post-operative outcomes. In a similar way, the presence of tibial reabsorption after revision surgery must be detected and its evolution and clinical impact must be followed with seriate controls.
To our knowledge, the study by Pietschmann et al. [14] is the only other one describing a technique of lateral plateau bone grafting. However, in his series of 17 patients, revision surgery was necessary for either an aseptic loosening (tibial, femoral or tibial, and femoral component), progression of osteoarthritis at the lateral compartment or dislocation of the insert and prosthetic fracture. The tibial plateau was fixed with two absorbable pins. At an average follow-up of 3.1 years, no radiographic signs of loosening wear or implant subsidence were observed and significant improvement of all clinical scores was reported.
The outcomes of the present study are comparable to those of Pietschmann et al., and both are similar to those reported with metal wedges and augments [14, 16]. The potential biologic and economic advantages make bone autografts an alternative to traditional metal wedges when dealing with bone loss during revision surgery for failed medial UKA’s.
Our study has several limitations. First of all, the study population was small with strict inclusion criteria and the study was limited to a single centre. Secondly, even though the follow-up was 5 years, this is still relatively short given the expected duration of the implants. Longer-term follow-up may yield graft complications that were not noticed during the follow-up period. Finally, the series was retrospective and lacked a control group, which makes any definitive conclusions questionable.
Conclusion
Tibial plateau autograft is an economic and valid alternative to metal wedges in the treatment of medial plateau collapse following UKA. Clinical results and satisfaction rates are encouraging and comparable between the two options. Potential advantages of autograft include preservation of the host bone stock, elasticity, which is similar to the surrounding bone and reduced costs. Partial reabsorption of the graft may be of concern with longer-term follow-up.
References
Barrett WP, Scott RD (1987) Revision of failed unicondylar unicompartmental knee arthroplasty. J Bone Joint Surg Am 69:1328–1335
Brandes M, Ringling M, Winter C, Hillmann A, Rosenbaum D (2010) Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res (Hoboken) 63(3):328–334
Bruni D, Akkawi I, Iacono F, Raspugli GF, Gagliardi M, Nitri M, Grassi A, Zaffagnini S, Bignozzi S, Marcacci M (2013) Minimum thickness of all-poly tibial component unicompartmental knee arthroplasty in patients younger than 60 years does not increase revision rate for aseptic loosening. Knee Surg Sports Traumatol Arthrosc 21(11):2462–2467
Chakrabarty G, Newman JH, Ackroyd CE (1998) Revision of unicompartmental arthroplasty of the knee. Clinical and technical considerations. J Arthroplasty 13(2):191–196
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 80(1):63–69
Hang JR, Stanford TE, Graves SE, Davidson DC, de Steiger RN, Miller LN (2010) Outcome of revision of unicompartmental knee replacement. Acta Orthop 81(1):95–98
Levine WN, Ozuna RM, Scott RD, Thornhill T (1996) Conversion of failed modern unicompartmental arthroplasty to total knee arthroplasty. J Arthroplasty 11(7):797–801
Lewold S, Robertsson O, Knutson K, Lidgren L (1998) Revision of unicompartmental knee arthroplasty: outcome in 1,135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand 69(5):469–474
Martin J, Wallace D, Woods D, Carr AJ, Murray DW (1995) Revision of unicondylar knee replacements to total knee replacement. Knee 2(2):121–125
McAuley JP, Engh GA, Ammeen DJ (2001) Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res 392:279–282
Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V (2014) Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res 472(5):1496–1501
Padgett DE, Stern SH, Insall JN (1991) Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am 73:186–190
Pearse AJ, Hooper GJ, Rothwell A, Frampton C (2010) Survival and functional outcome after revision of a unicompartmental to a total knee replacement: the New Zealand National Joint Registry. J Bone Joint Surg Br 92(4):508–512
Pietschmann MF, Ficklscherer A, Wohlleb L, Schmidutz F, Jansson V, Müller PE (2014) UKA can be safely revised to primary knee arthroplasty by using an autologous bone plate from the proximal lateral tibia. J Arthroplasty 29(10):1991–1995
Revell PA (2008) The combined role of wear particles, macrophages and lymphocytes in the loosening of total joint prostheses. J R Soc Interface 5:1263–1278
Robb CA, Matharu GS, Baloch K, Pynset PB (2013) Revision surgery for failed unicompartmental knee replacement: technical aspects and clinical outcome. Acta Orthop Belg 79:312–317
Saldanha KA, Keys GW, Svard UC, White RH, Rao C (2007) Revision of Oxford medial unicompartmental knee arthroplasty to total knee arthroplasty—results of a multicentre study. Knee 14(4):275–279
Saragaglia D, Estour G, Nemer C, Colle PE (2009) Revision of 33 unicompartmental knee prostheses using total knee arthroplasty: strategy and results. Int Orthop 33(4):969–974
Shi HF, Xiong J, Chen YX, Wang JF, Qiu XS, Wang YH, Qiu Y (2013) Early application of pulsed electromagnetic field in the treatment of postoperative delayed union of long-bone fractures: a prospective randomized controlled study. BMC Musculoskelet Disord 19(14):35
Siddiqui NA, Ahmad ZM (2012) Revision of unicondylar to total knee arthroplasty: a systematic review. Open Orthop J 6(Suppl 2):268–275
Springer BD, Scott RD, Thornhill TS (2006) Conversion of failed unicompartmental knee arthroplasty to TKA. Clin Orthop Relat Res 446:214–220
Tinius M, Klima S, Marquass B, Tinius W, Josten C (2006) Revision possibilities after failed unicompartmental knee arthroplasty, an analysis of 116 revisions. Z Orthop Ihre Grenzgeb 144(4):367–372
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cerciello, S., Morris, B.J., Lustig, S. et al. Lateral tibial plateau autograft in revision surgery for failed medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 773–778 (2017). https://doi.org/10.1007/s00167-015-3610-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3610-z