Abstract
Purpose
The purpose of this observational study was to evaluate serum levels of 25-OH-D of elderly patients presenting with orthopaedic illness. Furthermore, we enquired about potential confounders and risk factors of hypovitaminosis D in comorbidities and daily medication of the elderly.
Methods
Vitamin D levels in 1,083 patients aged >70 years and admitted to an orthopaedic surgery department were measured. Univariate and multivariate analyses were used to assess risk factors for insufficient vitamin D levels.
Results
Overall, 86 % of patients had insufficient serum levels of 25-OH-D and >60 % were vitamin D deficient. Serum vitamin D levels were lower during winter and months with fewer sunshine hours. Patients presenting with obesity, hypertension and osteoporosis were more likely to have low vitamin D levels.
Conclusions
We found a high prevalence of hypovitaminosis D in elderly, nonhospitalized orthopaedic patients. Given the well-known effects of vitamin D on bone metabolism and muscle health, as well as its nonskeletal effects, vitamin D insufficiency may have a negative impact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The essential role of vitamin D on bone health and calcium regulation is well known [1]. Inadequate low serum or plasma levels of 25-hydroxyvitamin D (25-OH-D) leads not only to skeletal effects such as rickets, osteoporosis and osteomalacia, but, as several recent studies suggest, exhibits also a number of nonskeletal effects [2]. In particular, hypovitaminosis D has been reported to increase the risk of cardiovascular diseases, type 2 diabetes and mental illness [3–5]. Furthermore, several studies suggest that it also regulates innate and adaptive immune function by activating macrophages, dendritic cells and lymphocytes [6]. Low serum 25-OH-D levels have been shown to increase the risk of respiratory tract infection and periprosthetic joint infection, and a recent clinical trial demonstrated that vitamin D supplementation reduced the risk of influenza A infection [7–9].
Vitamin D deficiency and insufficiency have been reported in several studies around the world [10]. It is estimated to affect more than one billion people of all races, ethnic backgrounds and age groups [1]. Especially among the elderly, high rates of vitamin D deficiency have been described [11–14]. Among inpatients of geriatric acute care units, lower vitamin D serum levels have been associated with a greater severity of chronic diseases, increased risks of acute decompensation and a higher risk of in-hospital mortality [15–17]. In line with this, hypovitaminosis D doubled the risk of hospitalisation for >14 days in a geriatric acute care unit [18].
Although several studies reported a widespread rate of vitamin D deficiency, epidemic data on orthopaedic patients, and furthermore, geriatric/orthopaedic patients, is scarce. Data revealing the prevalence of vitamin D insufficiency and deficiency in elderly patients may be of value to orthopaedic surgeons and geriatricians when treating their patients to prevent potential negative consequences in the operative and postoperative settings, to maintain good physical function and to preserve independence in daily life.
The purpose of this observational study was to evaluate serum levels of 25-OH-D of elderly patients presenting with orthopaedic illness in an orthopaedic university hospital in central Europe. Furthermore, we enquired about potential confounders and risk factors of hypovitaminosis D in comorbidities and daily medication of the elderly, as comorbidities and multimedication use are well known in such patients. We also assessed possible seasonal variations in serum 25-OH-D levels and its feasible association with the mean sunshine hours per month.
Methods
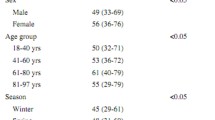
Between 1 January 2011 and 31 December 2012, serum 25-OH-D levels of all patients >70 years admitted to the orthopaedic department of our institution (1,083) were measured on admission. Generally, blood was taken on the day of admission. Mean patient age was 76 (±7.9) years (Table 1).
Measurement of serum 25-OH-D was standardised; the hospital laboratory used the ARCHITECT® 25-OH Vitamin D assay (Abbott GmbH & Co KG, Wiesbaden-Delkenheim, Germany). Patient demographic variables and background data were evaluated by retrospective chart review and checked for potential association with 25-OH-D levels. Included variables were age, sex, primary musculoskeletal diagnosis, body mass index (BMI), comorbidities, orally administered medication and any vitamin D supplements taken before admission (Table 1).
As yet there is no universally accepted classification of vitamin D levels. Vitamin D status was categorised primarily according to cutoff points used by Holick [1]. We defined sufficient vitamin D status as a serum 25-OH-D level >30 ng/ml. Vitamin D inadequacy was defined as >30 ng/ml and was further divided into insufficiency (20–30 ng/ml) and deficiency (<20 ng/ml). The distribution percentages of patients with insufficiency and deficiency were determined. To investigate the correlation between climate factors and vitamin D levels, sunshine hours for every month in 2011 and 2012 were collected by Deutscher Wetterdienst (the German weather center) in the region around Mainz, Germany. Weather data were taken for a radius of 50 km around the city centre of Mainz, corresponding to the living area of most tested patients. For each month, we correlated mean sunshine hours with mean vitamin D levels measured in the same month to evaluate any significant correlation.
Univariate analyses were used to assess the independent relative risk (RR) for vitamin D insufficiency or deficiency associated with potential risk factors [age, sex, nicotine abuse, obesity (BMI >30 kg/m2), carcinoma, psychiatric diseases, osteoporosis, hypertension, diabetes, cardiovascular diseases, alcoholism, hyperthyroidism/hypothyroidism, pulmonary diseases, renal failure, infectious diseases]. All analyses were performed with use of two-tailed tests. The level of significance was set at p ≤ 0.05.;95 % confidence interval (CI) and p value were calculated for each risk factor.
To determine what factors are predictors and what factors are confounders of hypovitaminosis D, multivariate linear regression analysis using the vitamin D level as a continuous variable was performed. All collected potential risk factors were included. To evaluate a possible association between the different medications patients received, these were also included in the multivariate regression analyses. The medication had to have been taken for at least the last three months before measurement of serum vitamin D level. All collected medications (proton-pump inhibitors, acetylsalicylic acid, metamizol, diclofenac, iso-butyl-propanoic-phenolic acid, N-acetyl-p-aminophenol, indomethacin) were included. The level of significance was set at p ≤ 0.05. With use of a forward stepwise method, variables were considered to be of significance if they had a final p ≤ 0.05 after adjusting for all other variables .
Results
A total of 1,083 patients participated in this study: 52.4 % were women, and ranged from 70 to 97 (mean 76) years. Overall, 86 % of patients were vitamin D insufficient and 64 % deficient; only 8 % were in the target range of 30–60 ng/ml. Serum vitamin D levels of all patients were normally distributed, with a mean of 17.1 ng/ml; minimum and maximum values ranged from 8 to 78.5 ng/ml, respectively.
Univariate analyses showed that obesity [p = 0.028, odds ratio (OR) 3.09], hypertension (p = 0.011, OR 3.08), osteoporosis (p = 0.001, OR 5.79), diabetes (p = 0.001, OR 5.4), and renal failure (p = 0.018, OR 5.93) were associated with low vitamin D levels. Patients supplementing vitamin D orally had a significantly higher level (p = 0.009) than patients without supplementation; sex (p = 0.433) was not associated with differences. Furthermore, the following variables showed no association with low levels: nicotine abuse (p = 0.673), carcinoma (p = 0.522), psychiatric diseases (p = 0.462), cardiovascular diseases (p = 0.812), alcoholism (p = 0.128), hyperthyroidism/hypothyroidism (p = 0.553) and pulmonary (p = 0.493) and infectious (p = 0.732) diseases (Table 2).
In multiple regression analysis, osteoporosis was significantly associated with low vitamin D levels (p = 0.007), as was hypertension (p = 0.032) and diabetes (p = 0.033) after adjustment for possible confounders. All other factors significantly associated with low vitamin D levels in univariate analysis showed no significant relationship and were dropped from the model obesity (p = 0.059), and renal failure (p = 0.246). Multivariate regression analyses showed no significant correlation between medication history and hypovitaminosis D (Table 3).
Variations in 25-OH-D levels between the winter and summer months were seen in our participants. During the summer months, the mean vitamin D level was 17.9 ng/ml; during the 6 winter months, the mean level was 15.1 ng/ml. The lowest concentrations occurred in November (13.1 ng/ml) and peak concentrations in August (19.97 ng/ml). Mean sunshine hours per month showed a strong correlation (p = 0.004, Pearson’s correlation 0.072) with mean levels, with higher mean levels during sunnier months (Table 4).
Discussion
To the best of our knowledge, this is the first study to report on an association between hypovitaminosis D and elderly orthopaedic patients in general. We found a high prevalence of vitamin D deficiency and insufficiency in our patients. These results are in line with former studies showing high rates of hypovitaminosis D in the elderly [13, 19]. We were able to show that not only orthopaedic patients with hip or vertebral fractures have low vitamin D levels but also the elderly orthopaedic patient in general. A novelty in this study is that mainly nonhospitalised elderly patients were tested. Extremely low vitamin D levels have been associated with osteomalacia and impaired muscle function, both core elements in the field of orthopaedic surgery. Good muscle function and healthy bones are essential for fast rehabilitation and positive outcome after orthopaedic surgery, and, especially in elderly patients, for good physical function [11, 20]. Physical function is important for the preservation of independence in daily life and the prevention of falls, which are associated with fractures and high mortality rates [21, 22]. Vitamin D depletion has been linked with impaired cognition, with specific damage to executive functions and speed of information processing, which can have a direct impact on selection of postural control strategies and reaction to falls [23]. Low vitamin D levels negatively affect muscle strength, which may impact fall patterns, severity and reaction to them [24]. Furthermore, several studies showed that lower 25-OH-D serum levels are a risk factor for orthostatic hypotension, which was reported to deteriorate functional autonomy of older patients and to have a close relationship with mortality and morbidity in the elderly [25, 26]: In a study of 546 patients >65 years, it was shown that vitamin D deficiency is a factor in the development of orthostatic hypotension. The authors concluded that during the evaluation of orthostatic hypotension, serum 25-OH-D levels should be checked and detected deficiency should be treated [25].
In our study, we found a mean vitamin D level of 17.1 ng/ml amongst 1,083 patients >70 years. There are few data on such geriatric and elderly orthopaedic patients, but they all report a widespread rate of hypovitaminosis D in the elderly [27, 28]. This is an alarming fact, knowing that the official recommendation by the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) is a minimum serum 25-OH-D level of 30 ng/ml in fragile elderly individuals, who are at an elevated risk of falls and fractures [29]. Bischoff-Ferrari et al. showed a 22 % reduction in falls of patients taking vitamin D supplements [30]. Gerdhem et al. evaluated 986 postmenopausal women and showed a twofold increased fracture risk for patients with 25-OH-D levels <20 ng/ml compared with patients with higher serum vitamin D levels [31]. Furthermore, a contributing role of vitamin D deficiency in the occurrence of simultaneous fractures has recently been described in a study of 472 elderly hip fracture patients [32].
We show the extent of seasonal variation in 25-OH-D levels throughout a two year period, as well as the association between mean sunshine hours and mean 25-OH-D serum levels in central Europe or comparable latitudes (e,g, Vancouver, 49°, 17′ N). Brustad et al. described seasonal variations a latitude of 69° North (northern Europe), which is in line with our results; however, owing to a generally high dietary intake of vitamin D in their patients, mean levels were sufficient (>30 ng/ml) in all tested seasons [33]. Our work demonstrated a correlation between sunshine hours per month and patient serum vitamin D levels, with higher mean levels during sunnier months. However, even in the months with the most sunshine hours, the mean level did not reach sufficient values. In May 2011, the sunniest month in the region around Mainz, a mean level of 18.75 ng/ml was measured. Vitamin D synthesis in the skin under the influence of UV light decreases with aging due to insufficient sunlight exposure and decreaes functional capacity of the skin [34, 35]. Our data suggest increasing vitamin D production from sunlight is not a realistic option for most elderly patients living in latitudes comparable with that of Mainz [50° N; e.g. Vancouver (49°, 17° N), Paris (48°, 51′ N) or Kiev (50°, 17′ N)].
Our data confirmed a significant association between vitamin D deficiency and obesity, diabetes mellitus, renal failure, hypertension and osteoporosis [14, 36]. Comparable with former studies, multivariate analyses showed no significant correlation between medication history and hypovitaminosis D [11].
As with any single-centre analysis, our study has some limitations. The majority of tested patients was light skinned. Given the predisposition of darker-skin-toned humans towards lower 25-OH-D levels, vitamin D deficiency and insufficiency amongst darker-skin-toned patients may be underrepresented in this study. The reported associations do not prove causal relationship. Actual daily sunlight exposure of our patients was only approximated, not truly known. Furthermore, doses of and compliance with vitamin D supplementation were not assessed.
We found a high frequency of vitamin D deficiency among our elderly orthopaedic patients in central Germany. More than 85 % of patients were vitamin D insufficient, with values measured below the target of 30–60 ng/ml. Adequate levels are required for effective bone metabolism and fracture and fall prevention, especially in the elderly, and also for many paracrine effects. Vitamin D supplementation is often perceived by patients and their physicians as an excessive medication and is easily dismissed to avoid polypharmacy. Therefore, screening and treating hypovitaminosis D is difficult, but it appears to be important in this patient population.
References
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Annweiler C, Souberbielle JC, Schott AM, de Decker L, Berrut G, Beauchet O (2011) Vitamin D in the elderly: 5 points to remember. Geriatr Psychol Neuropsychiatr Vieil 9:259–267
Mattila C, Knekt P, Mannisto S, Rissanen H, Laaksonen MA, Montonen J, Reunanen A (2007) Serum 25-hydroxyvitamin D concentration and subsequent risk of type 2 diabetes. Diabetes Care 30:2569–2570
Giovannucci E, Liu Y, Hollis BW, Rimm EB (2008) 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med 168:1174–1180
Menkes DB, Lancaster K, Grant M, Marsh RW, Dean P, du Toit SA (2012) Vitamin D status of psychiatric inpatients in New Zealand’s Waikato region. BMC Psychiatry 12:68
Hewison M (2010) Vitamin D and the immune system: new perspectives on an old theme. Endocrinol Metab Clin N Am 39:365–379
Ginde AA, Mansbach JM, Camargo CA Jr (2009) Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med 169:384–390
Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H (2010) Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr 91:1255–1260
Maier GS, Horas K, Seeger JB, Roth KE, Kurth AA, Maus U (2014) Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop 38:1499–1504
Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA et al (2009) Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 20:1807–1820
Maier GS, Jakob P, Horas K, Roth KE, Kurth AA, Maus U (2013) Vitamin D deficiency in orthopaedic patients: a single center analysis. Acta Orthop Belg 79:587–591
Hirani V, Primatesta P (2005) Vitamin D concentrations among people aged 65 years and over living in private households and institutions in England: population survey. Age Ageing 34:485–491
Schilling S (2012) Epidemic vitamin D deficiency among patients in an elderly care rehabilitation facility. Dtsch Arztebl Int 109:33–38
Maier GS, Jakobs P, Roth KE, Kurth AA, Maus U (2013) Is there an epidemic vitamin d deficiency in german orthopaedic patients? Clin Orthop Relat Res 471:3029–3035
Sutra Del Galy A, Bertrand M, Bigot F, Abraham P, Thomlinson R, Paccalin M et al (2009) Vitamin D insufficiency and acute care in geriatric inpatients. J Am Geriatr Soc 57:1721–1723
Beauchet O, Helard L, Montero-Odasso M, de Decker L, Berrut G, Annweiler C (2012) Hypovitaminosis D in geriatric inpatients: a marker of severity of chronic diseases. Aging Clin Exp Res 24:188–192
Annweiler C, Pochic S, Fantino B, Legrand E, Bataille R, Montero-Odasso M et al (2010) Serum vitamin D concentration and short-term mortality among geriatric inpatients in acute care settings. Adv Ther 27:245–249
Beauchet O, Launay CP, Maunoury F, de Decker L, Fantino B, Annweiler C (2013) Association between vitamin D deficiency and long hospital stay in geriatric acute care unit: results from a pilot cohort study. Aging Clin Exp Res 25:107–109
Simon J, Leboff M, Wright J, Glowacki J (2002) Fractures in the elderly and vitamin D. J Nutr Health Aging 6:406–412
LeBoff MS, Hawkes WG, Glowacki J, Yu-Yahiro J, Hurwitz S, Magaziner J (2008) Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int 19:1283–1290
Bruyere O, Slomian J, Beaudart C, Buckinx F, Cavalier E, Gillain S et al (2014) Prevalence of vitamin D inadequacy in European women aged over 80 years. Arch Gerontol Geriatr 59:78–82
Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293:2257–2264
Annweiler C, Montero-Odasso M, Schott AM, Berrut G, Fantino B, Beauchet O (2010) Fall prevention and vitamin D in the elderly: an overview of the key role of the non-bone effects. J Neuroeng Rehabil 7:50
Hamilton B (2010) Vitamin D and human skeletal muscle. Scand J Med Sci Sports 20:182–190
Soysal P, Yay A, Isik AT (2014) Does vitamin D deficiency increase orthostatic hypotension risk in the elderly patients? Arch Gerontol Geriatr 59:74–77
McCarroll KG, Robinson DJ, Coughlan A, Healy M, Kenny RA, Cunningham C (2012) Vitamin D and orthostatic hypotension. Age Ageing 41:810–813
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
Drinka P (1996) Vitamin D deficiency in older people. J Am Geriatr Soc 44:333
Rizzoli R, Boonen S, Brandi ml, Bruyere O, Cooper C, Kanis JA et al (2013) Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin 29:305–313
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY et al (2004) Effect of Vitamin D on falls: a meta-analysis. JAMA 291:1999–2006
Gerdhem P, Ringsberg KA, Obrant KJ, Akesson K (2005) Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA Study of Elderly Women. Osteoporos Int 16:1425–1431
Di Monaco M, Vallero F, Castiglioni C, Di Monaco R, Tappero R (2011) Low levels of 25-hydroxyvitamin D are associated with the occurrence of concomitant upper limb fractures in older women who sustain a fall-related fracture of the hip. Maturitas 68:79–82
Brustad M, Edvardsen K, Wilsgaard T, Engelsen O, Aksnes L, Lund E (2007) Seasonality of UV-radiation and vitamin D status at 69 degrees north. Photochem Photobiol Sci 6:903–908
Wolpowitz D, Gilchrest BA (2006) The vitamin D questions: how much do you need and how should you get it? J Am Acad Dermatol 54:301–317
Segal E, Zinman C, Raz B, Ish-Shalom S (2009) Low patient compliance–a major negative factor in achieving vitamin D adequacy in elderly hip fracture patients supplemented with 800 IU of vitamin D3 daily. Arch Gerontol Geriatr 49:364–367
de Boer IH, Ioannou GN, Kestenbaum B, Brunzell JD, Weiss NS (2007) 25-Hydroxyvitamin D levels and albuminuria in the Third National Health and Nutrition Examination Survey (NHANES III). Am J Kidney Dis 50:69–77
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maier, G.S., Horas, K., Seeger, J.B. et al. Vitamin D insufficiency in the elderly orthopaedic patient: an epidemic phenomenon. International Orthopaedics (SICOT) 39, 787–792 (2015). https://doi.org/10.1007/s00264-014-2519-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2519-3