Abstract
Purpose
Pathological fractures of the long bones are common complications of metastatic disease; however, the outcome of different surgical techniques for the treatment of these fractures has not been clearly defined. The aim of this study was to evaluate differences in prophylactic and therapeutic intramedullary nailing in femoral metastasic implants.
Methods
Sixty-five patients with metastasis of the femur were analysed retrospectively (37 females; 28 males) between 1995 and 2011 (follow-up 15 months). Forty-four presented with pathological fractures and 21 impending fractures (Mirel ≥7). The operative treatments used were intramedullary fixation with reamed long Gamma nails. The studied parameters were survival, radiological and analytical findings, and functional outcomes.
Results
Prophylactic nailing resulted in immediate postoperative deaths in 5 % vs. 11.4 % in therapeutic, and one technical complication was detected in each group. Among the surviving patients 75.9 % of the fractures and 100 % of impending lesions were able to walk after the operation. The mean survival time was 11 months in the therapeutic (range 1–49) and 14 in the prophylactic group (1–34). The prophylactic intramedullary nails required a lower transfusion rate (1.4 concentrates vs. 3.0), mobilised earlier (day 4.0 vs. 9.7) and needed a shorter hospital stay (eight days vs. 16 days) compared to therapeutic nails (p < 0.05).
Conclusion
Femoral intramedullary nailing of metastasic lesions provides satisfactory results both clinically and radiologically. Early treatment of the metastases prevents fractures and gives better results, improving life quality of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathological and impending fractures of the long bones caused by metastatic disease are a common complication of a variety of primary malignant tumours [1]. Advances in oncological treatment over recent years have led to an increased life expectancy and a higher incidence of metastases [2] with the skeleton as the third most frequent site [1]. These lesions lead to pathological or impending fractures of long bones causing a serious decrease in quality of life. Many methods have been described to treat pathological fractures of the long bones such as the use of conventional osteosynthesis. However, the exact role of different surgical treatments of pathological fractures with respect to the outcome and patient benefit has not yet been clearly defined [3]. Intramedullary fixation is a useful solution for palliation being less invasive and allowing early weight bearing to preserve independence as long as possible [4]. Fixation of long bone fractures usually can be accomplished with minimal blood loss or morbidity, thereby improving quality of life of the remaining months significantly [5].
The detection and treatment of impending pathological fractures has steadily improved [6]. Prophylactic surgical stabilisation of such lesions before fracture is of great benefit to patients with metastases, and results in an improved quality of life.
This study examined two groups of patients with the aim of comparing the results of prophylactic and therapeutic nailing according to radiological findings such as reduction and consolidation in addition to analytical (blood loss and need of transfusion) and clinical (hospitalisation, ambulation) results and complications.
Material and methods
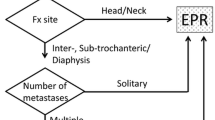
We made a retrospective study of 65 patients with femoral metastases treated with intramedullary nails between 1995 and 2011 at the Department of Traumatology in Hospital Clinico San Carlos in Madrid. There were 21 prophylactic and 44 therapeutic nails with a mean follow-up of 15 months (range 3-27). The fixation of the impending fractures were performed according the Mirels’ scoring system (≥7), and the mean value in our study was 9.1 (Fig. 1).
In the therapeutic group 26 patients were females and 18 were males vs. 11 females and 10 males in the prophylactic nailing. Mean age was 69.1 years in the first group presenting with multiple metastases at the time of surgery in 84.1 %, while these values were 64.5 years and 64.7 % in the latter. The metastases were located primarily in the axial skeleton, lungs and liver. The most frequent primary tumour in females was breast carcinoma (73.1 %) in therapeutic nailing; among the prophylactic group, breast carcinoma (27.3 %) was as frequent as multiple myeloma (27.3 %) and pulmonary carcinoma (27.3 %). Among men pulmonary carcinoma was the primary tumour in 27.8 % of the therapeutic and multiple myeloma in 60.0 % of prophylactic nailing. As to the localisation of the metastases, the subtrochanteric region predominated in both groups, followed by the diaphyseal and pertrochanteric region.
Therapeutic intramedullary nailing was performed with 44 long reamed static Gamma nails, closed reduction was achieved in 40 fractures and four cases needed an open reduction of the fracture. As to the prophylactic nails 21 were reamed long static Gamma nails. The cephalomedular angles used were, in order of frequency, 125°, 130° or 135° and the cephalic nails 90, 95, 100, 85 or 105 mm. None of the patients had other fractures or metastases that needed fixation at the time of surgery according to the Mirels’ scoring system (Fig. 2).
The parameters studied were survival, radiological findings, such as reduction and consolidation, anaemia, need for transfusion, ambulation, hospital stay and complications. Statistical correlation was analysed with ANOVA and p < 0.05 was deemed a statistically significant level.
Results
The mean surgery time was 47.8 minutes (range 15–90) in the therapeutic nails and 22.7 minutes (range 15–55) in the prophylactic (p = 0.003).
Survival
The mean survival time was 11 months in the therapeutic (range 1–49) and 14 in the prophylactic (1–34), excluding postoperative immediate death in six cases (p = 0.032). The mean follow up was 14.5 months (range 3–27).
Radiological findings
In the therapeutic nailing 71 % of the fractures obtained medial contact, 21 % did not have medial contact and 8 % of the fractures showed lysis after fixation. A total of 69 % of the implants consolidated—100 % of prostate carcinomas, 90 % of multiple myeloma, 56 % of breast cancers and 3 % of pulmonary tumours.
Anaemia
The need for transfusion was 2.5 concentrates in mean, of which 3.0 (0–14) in therapeutic and 1.4 (0–6) in prophylactic were statistically significant (p = 0.027) (Table 1).
Ambulation
Mobilisation usually started on the second day in both groups. In therapeutic nailing ambulation started on day 9.7 (range 2-20) with a mean hospital stay of 16.3 days (range 4–60). The same values in the prophylactic group were 4.0 (range 1–15) and 8.2 (range 3–27), which were significantly lower (p = 0.012). Among the surviving patients (67.4 % vs. 81.9 %) at six months after surgery, 75.9 % vs. 100 % ambulated (Table 2).
Complications
Immediate postoperative death was statistically less (p = 0.041) in prophylactic nailing 1 (5 % vs. 11.4 %): one respiratory failure vs. one cardiovascular emboli and four respiratory failures in therapeutic nailing.
One technical complication was detected in each group, i.e. in therapeutic (iatrogenic fracture) and in prophylactic (Gamma nail failure). No difference in complications was found between prophylactic and therapeutic nailing (p = 0.52).
Discussion
Femur and spine constitute the most frequent sites for metastatic tumours of the skeleton [7, 8]. In our study the predominating primary tumour was breast carcinoma followed by pulmonary carcinoma, multiple myeloma and prostate carcinoma which correlates with other reports [7].
Approximately 10 % of the patients with bone metastases develop a pathological fracture of the long bones [8]. The foremost aims of the metastatic treatment are to relieve pain, permit early mobilisation and preserve the function of the affected limb, allowing the patient to regain independency while keeping hospital stay as short as possible [3, 8]. Benefits of treatment must be judged against the possible complications and expected life span of the patients avoiding overtreatment [8].
The management of metastatic deposits in long bones is a source of debate and the best method of reconstruction is uncertain [9]. Conservative treatment has shown a greater morbidity/mortality leaving surgery as the main method of therapy [4]. Some surgeons prefer endoprosthetic replacement while others advocate the use of reconstruction nails or other osteosynthetic devices with or without the adjunct of cement [3]. The techniques of long-lasting biological reconstruction are more demanding, being only justified in selected situations such as for patients with a solitary metastasis, e.g. metastatic lesion from a primary renal carcinoma [1, 8]. Osteosynthesis is less aggressive than endoprosthetic replacement, providing an increased quality of life in these patients and full weight-bearing with fewer complications [3]. As to osteosynthesis, intramedullary nailing is biomechanically superior to the plate with greater axial stability, rotational control and better distribution of the loads along the bone. The long nails also prevent future potential diaphyseal fractures; the use of short Gamma nails in pathological fractures has therefore been restricted. Nails also provide the possibility to perform a closed approach with low morbidity and early functional recovery. Reamed nails have shown biomechanical advantages over unreamed and the theoretical risk of dissemination of tumour cells has not been demonstrated [10–13]. Preventive stabilisation, in contrast, reduces the number of fractures and does not lead to an increase in the number of pulmonary metastases [14]. We therefore prefer to perform osteosynthesis with reamed Gamma nails whenever possible, e.g. femoral implants not affecting femoral head or its vascularisation.
Other studies report a mean hospital stay of 23 days, achieving weight bearing on day 57 with a mean survival of 272 days in therapeutic and 148 days in the prophylactic group [5]. Our clinical results show better clinical results with earlier ambulation and shorter hospital stay.
Intramedullary nailing as a preventive measure of impending fractures provides easier osteosynthesis with less morbidity and shorter recovery, permitting optimisation at the time of surgery and pain relief. The Mirels’ scoring system has proved to be a reliable assessment to determine the precise timing of surgical intervention of these implants, ≥7 indicating osteosynthesis [9, 15, 16]. Our study suggests less need for transfusion with earlier ambulation and shorter hospital stay in prophylactic nails compared to therapeutic nailing. A wider range of haemoglobin and hematocrit values were detected in therapeutic nails, although this was not statistically significant. Other studies didn’t detect any significant difference in the complications in patients with complete or impending fracture, which is supported by our results [3].
A limitation of this study is the difference in mean age (69.1 years vs. 64.5 years) and associated metastases (84.1 % vs. 64.7 %) between therapeutic and prophylactic intramedullary nailing. Both these parameters could affect mean survival, and less metastatic disease could depend on less progression of the disease and thereby a better prognosis. Although, it is well established that the prophylactic treatment of impending pathological fractures results in longer postoperative survival than the treatment of complete pathological fractures [4].
The timing of surgery is dependent on the patient’s general condition, but can ideally be performed at the first safe opportunity, reducing the operative risk due to the avoidance of emergency surgery. According to our study, preventive fixation has both a higher survival and ambulation rate at six months after surgery. Our study supports the early treatment of metastatic implants prevents future fractures and that these operations present less need for transfusion, provide earlier ambulation and a shorter hospital stay, thus improving oncological patients’ quality of life.
References
Sarahrudi K, Hora K, Heinz T, Millington S, Vécsei V (2006) Treatment results of pathological fractures of the long bones: a retrospective analysis of 88 patients. Int Orthop 30(6):519–524
Harrington KD (1997) Orthopedic surgical management of skeletal complications of malignancy. Cancer 80(8 Suppl):1614–27
Wedin R, Bauer HCF (2005) Surgical treatment of skeletal metastatic lesions of the proximal femur, endoprothesis or reconstruction nail? J Bone Joint Surg [BR] 85-B:1653–7
Katzer A, Meenen NM, Grabbe F, Rueger JM (2002) Surgery of skeletal metastases. Arch Orthop Trauma Surg 122:251–258
Obert L, Jarry A, Lepage D, Jeunet L, Tropet Y, Vichard P, Garbuio P (2005) Centromedullary nailing of the femur for bone metastasis: clinical and radiological evaluation using the Tokuhashi score in 24 patients. Rev Chir Orthop Reparatrice Appar Mot Dec 91(8):737–45
Weikert DR, Schwartz H (1991) Intramedullary nailing for impending pathological subtrochanteric fractures. J Bone Joint Surg [Br] 73-B:668–70
Toma CD, Dominkus M, Nedelcu T, Adbolvahab F, Assadian O, Krepler P, Kotz R (2005) Metastatic bone disease: a 36-year single centre trend analysis of patients admitted to a tertiary orthopaedic surgical department. Rev Chir Orthop Reparatrice Appar Mot Dec 91(8):737–745
Böhm P, Huber J (2002) The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg [Br] 84-B:521–529
Ruairi F, Quinlan JF, Stapleton RD, Hurson B, Dudeny S, O’Toole GC (2011) Inter- and intra-observer variability associated with the use of the Mirels’ scoring system for metastatic bone lesions. Int Orthop 35(1):83–86
Cole AS, Hill GA, Theologis TN, Gibbons CL, Willett K (2000) Femoral nailing for metastatic disease of the femur: a comparison of reamed and unreamed femoral nailing. Injury 31(1):25–31
Harrington KD, Sim FH, Enis JE, Johnston JO, Diok HM, Gristina AG (1976) Methylmethacrylate as an adjunct in internal fixation of pathological fractures. Experience with three hundred and seventy-five cases. J Bone Joint Surg Am 58(8):1047–1055
Pongracz N, Zimmermann R, Kotz R (1988) Orthopaedic management of bony metastases of renal cancer. Semin Surg Oncol 4(2):139–142
Windhager R, Ritschl P, Ursula Rokus W, Kickinger O, Braun RK (1989) Die Rezidivhäufigkeit von intra- und extraläsional operierten Metastasen langer Röhrenknochen. Z Orthop 127:402–405
Bouma WH, Mulder JH, Hop WC (1983) The influence of intramedullary nailing upon the development of metastases in the treatment of an impending pathological fracture: an experimental study. Clin Exp Metastasis 1:205–212
Mirels H (1989) Metastasic disease in long bones: a proposed scoring system for diagnosing impending pathological fractures. Clin Ortop 249:256–264
Damron TA, Morgan H, Prakash D, Grant W, Aronowitz J, Heiner J (2003) Critical evaluation of Mirels’ rating system for impending pathologic fractures. Clin Orthop Relat Res Oct 415:S201–207
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arvinius, C., Parra, J.L.C., Mateo, L.S. et al. Benefits of early intramedullary nailing in femoral metastases. International Orthopaedics (SICOT) 38, 129–132 (2014). https://doi.org/10.1007/s00264-013-2108-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2108-x