Abstract
Purpose
We describe the outcome in a series of patients treated for metastatic peri-actetabular and iliac bone destruction using a modified technique of Harrington’s procedure.
Methods
Between 2006 and 2012, nine patients with a mean age of 62.2 years (42–75 years) were treated using a modified Harrington technique. Thereby, total hip replacement implants augmented by two to three threaded pins and cement were used to restore bony continuity of the pelvis and to achieve a stable construction allowing immediate full-weight bearing mobilisation.
Results
Acetabular destruction was graded according to Harrington’s classification of peri-acetabular metastatic destruction, as class IV in one case, class III in six, and class II in two cases. The pre-operative ASA score ranged from II–IV. There were no intra-operative deaths or major complications such as excessive haemorrhage, deep infections, lesions of the femoral nerve, loss of fixation, or dislocations at final follow-up. Eight patients achieved an improvement of their functional status postoperatively. One reconstruction required revision and four patients died due to their underlying disease ten to 36 months after surgery.
Conclusion
We found this technique an effective, reproducible, and long-lasting method to relieve pain and improve or restore function in patients with destructive metastatic lesions of the peri-acetabular bone and the iliac wing. Although we performed surgery even in severely ill patients with extended, generalised metastatic disease we had no intra- or postoperative death and observed no major complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pelvis represents one of the most commonly affected sites in patients with bony metastases and although surgical interventions are less frequent compared to those for metastases of the long bones, the frequency will increase due to continuous improvements in quality of life and prognosis for the survival in patients living with invasive cancer [1]. Treatment strategies for peri-acetabular metastatic lesions include non-operative options such as systemic chemotherapy, local irradiation, bisphosphonates or hormonal treatment, and surgical reconstruction of the pelvis [2]. The decision to perform a surgical reconstruction of metastatic pelvic bone cancer is dependent on many different factors such as comorbidities, prognosis for survival, not responding to non-operative treatment strategies as well as the pre-operative functional status of the patient.
Although surgical advances in the past few years have facilitated the treatment of bony metastases, the surgical reconstruction of peri-acetabular lesions remains a challenging task. The therapeutic goal should be almost painless full-weight bearing postoperatively and the achievement of a stable reconstruction for the remaining expected lifetime of the patient [2]. The technique of iliac and acetabular reconstruction using threaded pins, acetabular shell, and bone cement was first described by Harrington in 1981 [3].
We describe the outcome in nine patients operated upon for metastatic peri-actetabular and iliac bone destruction using a modified technique of Harrington’s procedure. Total hip arthroplasty (THA) implants augmented by two to three threaded pins and cement or a single compound osteosynthesis of the iliac wing without simultaneous THA were used to restore bony continuity of the pelvis and to achieve a stable reconstruction allowing immediate full-weight bearing mobilisation and ensure stability for the remaining expected lifetime of the patient.
Patients and methods
From 2006 to 2012, nine patients with metastatic pelvic bone destruction were treated operatively at our department using THA implants augmented by threaded pins and cement in seven cases or a single compound osteosynthesis of a metastatic area in the iliac wing after curettage of the defect in two cases. The patients underwent surgery for pain, increased risk of fracture, or to re-establish the possibility to bear weight. The operations were performed by two experienced tumour surgeons (WME and AL) at a single institution. Acetabular reconstruction was considered for patients with an established oncological diagnosis and a pre-operative anaesthetic assessment (ASA 1–4) [4]. Further criteria for surgery were an impending or preceding pathological fracture, non-weight bearing due to pain or fractures and expected survival for more than six months. Patients were excluded if further fracture threatening lesions of the ipsilateral tibia, distal femur, or metastases in the contralateral acetabulum/iliac bone were detected. The extent of peri-acetabular osteodestruction was classified using Harrington’s classification (Table 1) [3]. We observed one patient with class IV destruction, six with class III, and two with class II destruction of the peri-acetabular bone. The mean age of all patients included in this series was 62.2 years (range, 42–75). There were four female and five male patients. The left side was affected in all of the cases. The primary tumour was known in all of the cases except one (cancer of unknown primary, histologically confirmed squamous cell metastasis). The most frequent diagnosis was a renal cell carcinoma (Table 2).
Six patients underwent pre-operative selective embolism of the metastatic deposit. Five patients had been receiving local radiotherapy one to three months before surgery and nine patients underwent postoperative local radiotherapy.
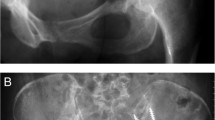
Radiological assessment was based on two plane radiographs of the pelvis, hip and femur, a CT- and MRI scan of the pelvis and a whole-body radio-isotope bone scan (Figs. 1 and 2).
a Plain antero-posterior radiograph of a 69-year-old male patient with supra-acetabular osteolysis, classified as class III according to Harrington [3]. b Antero-posterior radiograph of the same patient after six months of follow-up. Two pins were sufficient to achieve stable conditions. Having established that the pins were in the correct position, bone cement (Palacos, Heraeus, Germany) was inserted and pressed into the curetted area
a Plain antero-posterior radiograph of a 70-year-old male patient with a supra-acetabular osteolysis, classified as class III according to Harrington [3]. b, c Same patient at six months of followup. Having established that the pins were in the correct position, bone cement (Palacos, Heraeus, Germany) was inserted and pressed into the curetted area. In addition, total hip arthroplasty (THA) was implanted according to the previously described technique.
Pre- and postoperative information on pain and functional status (unaided mobilisation, walking stick, crutches, or use of a wheel chair) was obtained from all patients included in this series. In addition, we classified complications according to Goslings and Gouma [5].
Surgical technique
A transverse incision was made over the iliac crest with the patient in supine position, followed by preparation of the tumour capsule and curettage of the metastasis under direct vision. A second, transgluteal (Bauer’s approach) or anterolateral approach (modified Watson-Jones approach) to the hip was performed in patients who underwent simultaneous THA, followed by femoral neck section, extraction of the femoral head, exposure of the acetabulum to assess the bony architecture and the level of osteodestruction. Continued curettage of the tumour on the acetabular side was performed, if necessary. Two or three threaded pins were inserted from the iliac crest. With the aid of fluoroscopic imaging the ideal positions of at least two pins (to the front, behind and medial floor of the acetabulum) were achieved in five cases. In the other four cases at least two pins were sufficient to achieve stable conditions. Having established that the pins were in the correct position, bone cement (Palacos, Heraeus, Germany) was inserted and pressed into the curetted area. A cavity for the acetabular component was established by the use of a cup pressuriser. Finally, the acetabular component (Müller II flat-profile polyethylene cup, Zimmer, Germany; Triloc acetabular shell, DePuy, Germany; ACCIS large-head total hip system, Implantcast, Germany) was cemented in place. In five cases we used a polyethylene cup for acetabular reconstruction, two patients were treated by the use of large-head metal-on-metal implants in order to achieve security against luxation as well as to improve range of motion. These patients have been either cachectic and/or have had significant gluteal atrophy as a result of longer-term immobility due to their underlying disease. The standard acetabular component used for this procedure at our institution is a flat-profile polyethylene cup (Müller II). In two cases, we used another polyethylene cup (Triloc acetabular shell) because our standard implant was not available at the time of surgery.
Finally, the femoral component (Weber Curved Stem, Zimmer, Germany; Alloclassic stem, Zimmer, Switzerland; ACCIS total hip system, Implantcast, Germany) was implanted in the standard manner.
Postoperatively, full weight-bearing mobilisation on two crutches was possible for seven of nine patients, and partial weight-bearing was necessary for two patients, due to poor bone quality or unexpected extended bony defects of the acetabulum/iliac wing.
Results
There were no intra-operative deaths or major complications such as vascular or nerve injuries and excessive haemorrhage. At final follow-up (mean 13 months, range 2–30 months) we did not observe complications such as a loss of fixation or dislocations, but we had one complication for which further surgery was necessary—removal of the threaded pins performed ten months after initial surgery due to refractory pain from the iliac crest and radiological evidence of protruding pins in this area. This was classified as grade 2 according to Goslings and Gouma. No further postoperative complications could be observed among the other patients. Of the nine patients, four died due to their underlying disease. The mean time from surgery to death was 20 months (10–36). The mean follow-up time for survivors was 13 months (1–30 months). Functional results were carried out six months after surgery by assessment of patients’ mobility (unaided walking, one walking stick, two crutches, wheelchair, bedridden). Six patients improved their functional status, two pre-operatively unaided mobile patients remained mobile postoperatively, and one patient who underwent surgery recently required a wheelchair pre-operatively due to severe pain on weight bearing and postoperatively she is able to walk with crutches. Further details are shown in Table 2. All patients reported an improvement in terms of pain, especially under exertion; however, eight patients required non-opiate or opiate analgesia due to progression of their disease.
Discussion
Metastatic destruction of the acetabulum and the peri-acetabular region is associated with a high incidence of immobilisation and severe pain. Patients should be considered for surgery if non-operative treatment options such as local radiotherapy, bisphosphonate and/or hormonal therapy or partial weight-bearing do not result in sustained improvement of the situation. In consideration of the fact that curative treatment options are not available in most cases of metastatic pelvic bone disease, the goals of surgical reconstruction should be to achieve a stable reconstruction which allows early, fully weight-bearing mobilisation and relief of pain [6–8].
Functional restoration in cases of metastatic periacetabular bone disease often requires reconstruction of much of the pelvis [9]. Surgical options include the use of autogenous bone grafts, allografts, compound osteosynthesis and/or an endoprosthesis [9, 10]. Especially in cases of a less extended bony destruction of the peri-acetabular region (Harrington class II), several authors have described the use of acetabular support rings in combination with THA or reconstruction using saddle prostheses following excision of primary and metastatic peri-acetabular tumours [11–13]. Although they have reported good results immediately after surgery or during early follow-up, reconstruction failures or degradation of the functional status have been observed in a considerable portion of the patients, especially following implantation of saddle prostheses. Renard et al. noted that osteoporosis and insufficient soft tissue quality have affected the functional results in a series of 15 patients treated with saddle prosthesis for periacetabular tumours [14]. A recent study by Jansen et al. reported a high risk of complications and poor long-term function in patients following acetabular reconstruction with saddle prostheses after peri-acetabular tumour surgery [15]. Another technique of endoprosthetic restoration, especially in relation to reconstruction of extended pelvic defects in cases of primary malignant tumours or solitary metastatic bony lesions of the pelvis, is the internal hemipelvectomy and reconstruction with an endoprosthetic pelvic replacement [9, 16–19]. Although this technique, first described in 1978, has been improved due to the possibility of exact planning of resection and construction of the implants using three-dimensional imaging, the functional outcome has been described as limited to poor. Furthermore, this technique seems to be associated with a high incidence of postoperative complications, such as deep infection and dislocation [9, 17–19].
In our series, we performed acetabular reconstruction using a modified technique of the procedure described by Harrington for class II–IV destructions to achieve a stable construct using threaded pins inserted between the superior acetabulum and the sacroiliac joint, cemented together with an acetabular shell (polyethylene or metal), which was placed in conjunction with the pins. This technique allows immediate full-weight bearing mobilisation on one side and achieves an improvement in terms of pain on the other side.
We observed an improvement of the pre-operative functional status in all cases (apart from the two patients who had not been functionally impaired before surgery). Although we performed surgery in patients with many co-morbidities (four patients classified as ASA 4) with extended, generalised metastatic disease we had no intra- or postoperative deaths and observed no major complications such as excessive haemorrhage, deep infections, lesions of the femoral nerve, loss of fixation, or dislocations as described in other series after performing various methods for pelvic reconstruction [9, 14, 15, 17–19]. Tillman et al. have reported similar results in their series of 19 patients treated with a three-pin modified Harrington technique with respect to occurrence of major intra- and postoperative complications as well as the functional outcome [6].
However, similar procedures described in the literature have reported a high risk of significant complications and a high incidence of intraoperative deaths, but the majority of these reports did not distinguish between complications following Harrington’s technique and those resulting from other surgical techniques used in their series [3, 6, 20–22].
Conclusion
We find this technique an effective, reproducible and long-lasting method to relieve pain and improve or restore function in patients with destructive metastatic lesions of the peri-acetabular bone and the iliac wing.
References
Windhager R (2005) Surgical treatment of pelvic metastases. In: Jasmin C, Capanna R, Coia L, Coleman R, Saillant G (eds) Textbook of bone metastases. John Wiley & Sons, Ltd, pp 185–194
Ghert M, Alsaleh K, Farrokhyar F, Colterjohn N (2007) Outcomes of an anatomically based approach to metastatic disease of the acetabulum. Clin Ortop Res 459:122–127
Harrington KD (1981) The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg 63-A:653
Saklad M (1941) Grading of patients for surgical procedures. Anesthesiology 2:281–284
Goslings JC, Gouma DJ (2008) What is a surgical complication? World J Surg 32(6):952
Tillman RM, Myers GJC, Abudu AT, Carter SR, Grimer RJ (2008) The three pin modified “Harrington” procedure for advanced metastatic destruction of the acetabulum. J Bone Joint Surg 90-B:84–88
Faisham WI, Muslim DAJ, Bhavaraju VMK, Nawaz AH, Zulmi W (2009) Modified Harrington procedure for acetabular insufficiency due to metastatic malignant disease. Malays Orthop J 3(1):36–41
Han I, Lee YM, Cho HS, Oh JH, Lee SH, Kim HS (2010) Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg 2:160–166
Mueller PE, Dürr HR, Wegener B, Pellengahr C, Refior HJ, Jansson V (2002) Internal hemipelvectomy and reconstruction with a megaprosthesis. Int Orthop 26(2):76–79
Natarajan MY, Bose JC, Mazhavan V, Rajagopal TS, Selvam K (2001) The Saddle prosthesis in periacetabular tumours. Int Orthop 25(2):107–109
Nilsson J, Gustafson P, Fornander P, Ornstein E (2000) The Harrington reconstruction for advanced periacetabular metastatic destruction: good outcome in 32 patients. Acta Orthop Scand 71(6):591–596
Stark A, Bauer HCF (1996) Reconstruction in metastatic destruction of the acetabulum. Acta Orthop Scand 67(5):435–438
Aboulafia AJ, Buch R, Mathews J, Li W, Malawer M (1995) Reconstruction using the saddle prosthesis following excision of primary and metastatic periacetabular tumors. Clin Orthop 314:203–213
Renard AJS, Veth RPH, Schreuder HWS, Pruszczyuski M, Keller A, Van Hoesel Q, Bokkerink JPM (2000) The Saddle prosthesis in pelvic primary and secondary musculoskeletal tumours: functional results at several post operative intervals. Arch Orthop Trauma Surg 120:188–194
Jansen JA, van de Sande MAJ, Dijkstra PDS (2013) Poor long-term clinical results of saddle prosthesis after resection of periacetabular tumors. Clin Orthop Relat Res 471:324–331
Johnson JTH (1978) Reconstruction of the pelvic ring following tumor resection. J Bone Joint Surg [Am] 60:747–751
Bruns J, Luessenhop SL, Dahmen G (1997) Internal hemipelvectomy and endoprosthetic pelvic replacement: long-term follow-up results. Arch Orthop Trauma Surg 116:27–31
Wirbel RJ, Schulte M, Maier B, Mutschler WE (1999) Megaprosthetic replacement of the pelvis. Acta Orthop Scand 70:348–352
Pilge H, Gradl G, von Eisenhart-Rothe R, Gollwitzer H (2012) Incidence and outcome after infection of megaprostheses. Hip Int 22(8):83–90
Allan DG, Bell RS, Davis AJ, Langer F (1995) Complex acetabular reconstruction for metastatic tumor. J Arthroplasty 10:301–306
Vena V, Hsu J, Rosier RN, O’Keefe RJ (1999) Pelvic reconstruction for severe periacetabular metastatic disease. Clin Orthop 362:171–180
Marco RA, Sheth DS, Boland BJ, Wunder JS, Siegel JA, Healey JH (2000) Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am 82(5):642–651
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vielgut, I., Sadoghi, P., Gregori, M. et al. The modified Harrington procedure for metastatic peri-acetabular bone destruction. International Orthopaedics (SICOT) 37, 1981–1985 (2013). https://doi.org/10.1007/s00264-013-1940-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-1940-3