Abstract
Multiple myeloma (MM) is a clonal plasma cell malignancy typically associated with the high and uniform expression of the CD38 transmembrane glycoprotein. Daratumumab is a humanized IgG1κ CD38 monoclonal antibody (MoAb) which has demonstrated impressive single agent activity even in relapsed refractory MM patients as well as strong synergy with other anti-MM drugs. Natural Killer (NK) cells are cytotoxic immune effector cells that mediate in vivo tumour immunosurveillance. NK cells also play an important role during MoAb therapy by inducing antibody dependent cellular cytotoxicity (ADCC) via their FcγRIII (CD16) receptor. Furthermore, 15% of the population express a naturally occurring variant of CD16 harbouring a single-point polymorphism (F158V). However, the contribution of NK cells to the efficacy of daratumumab remains debatable as clinical data clearly indicate the rapid depletion of CD38high peripheral blood NK cells in patients upon daratumumab administration. In contrast, CD38low peripheral blood NK cells have been shown to survive daratumumab mediated fratricide in vivo, while still retaining their potent anti-MM cytolytic effector functions ex vivo. Therefore, we hypothesize that transiently expressing the CD16F158V receptor using a “safe” mRNA electroporation-based approach on CD38low NK cells in combination with daratumumab could represent a novel therapeutic option for treatment of MM. In the present study, we investigate a NK cell line (KHYG-1), derived from a patient with aggressive NK cell leukemia, as a platform for generating CD38low NK cells expressing CD16F158V which can be administered as an “off-the-shelf” therapy to target both CD38high and CD38low tumour clones in patients receiving daratumumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) is a disease of clonal proliferation of malignant plasma cells in the bone marrow microenvironment and is the second most common haematological cancer [2]. While MM remains largely incurable, the past two decades have witnessed the development of several important new therapies for MM, including proteasome inhibitors, immunomodulatory drugs (IMiDs), and monoclonal antibodies (MoAb), such as daratumumab and elotuzumab [3, 4]. This has led to an increased focus on the role of Natural Killer (NK) cells in MM, as they are considered key effectors of MoAb. NK cells are large granular effector lymphocytes of the innate immune system, and can target malignantly transformed cells without prior sensitization. NK cells can also lyse antibody-tagged target tumour cells by binding the Fc portion of a MoAb via the Fc receptor (FcγRIIIA) (CD16), a mechanism referred to as antibody dependent cell cytotoxicity (ADCC) [5, 6]. A naturally occurring variant of CD16 (CD16F158V) has been shown to bind with the Fc portion of antibodies with higher affinity and induce greater ADCC against tumour cells in the presence of MoAb [7].
Daratumumab is a human IgG1 kappa MoAb that targets CD38, a transmembrane glycoprotein uniformly and highly expressed on MM cells [8]. CD38 has ecto-enzymatic activity and functions as an adhesion molecule [9]. As previously reported in four Phase-3 studies, the addition of daratumumab to the standard of care in both relapsed refractory or transplant-ineligible newly diagnosed MM (NDMM) resulted in a ≥ 45% reduction in the risk of disease progression or death [10,11,12,13]. Daratumumab has a multifaceted effect, which includes both direct and indirect mechanisms of action. Fc-dependent immune effector mechanisms include complement-dependent cytotoxicity (CDC), ADCC and antibody dependent cellular phagocytosis (ADCP), while inhibition of ecto-enzymatic function and direct apoptosis induction may also contribute to the efficacy of the antibodies to kill MM cells [14]. However, treatment with daratumumab leads to rapid depletion (85%) of CD38pos NK cells, lasting up to 6 months following cessation of treatment [15]. This is primarily attributed to the high cell surface expression of CD38 on NK cells. CD38 plays an important role in NK cells by facilitating the production of ADP-ribose Pyrophosphate (ADRP) and subsequent mobilization of intracellular Ca2+ necessary for their cytolytic degranulation [16].
Daratumumab treatment also leads to a decrease in CD38 expression on MM cells, resulting in the generation of CD38low MM clones which may lead to a reduction in the efficacy of direct killing mechanisms [15, 17]. Therefore, as daratumumab mediates NK cell depletion, ADCC may play a lesser biological role than originally thought in terms of clinical response, which may then be more reliant on CDC, macrophage mediated ADCP, and in-particular T cell mediated immunity for long term disease control [18]. This suggests that novel strategies involving the adoptive transfer of low (or absent) CD38 expressing NK cells (CD38low NK) could optimize daratumumab efficacy by fully exploiting ADCC [19]. However, as CD38low NK cells comprise only a small fraction of blood NK cells, the generation of such high numbers of CD38low NK cells is clinically challenging, Furthermore, the elimination of CD38low expressing MM cells with activated NK cells has not been demonstrated in prior studies [6].
In the present study we investigate KHYG1, a CD38low NK cell leukemia cell line as an “off-the-shelf” NK cell platform transiently expressing the CD16F158V receptor which can be administered in combination with daratumumab to target CD38high expressing MM cells. Furthermore, we show that these modified NK cells can also target CD38low expressing MM cells in vitro. We envisage this combination of cellular therapy and daratumumab could be a novel therapeutic strategy for the treatment of MM, leading to increased depth of response and reduced risk of progression.
Materials and methods
Cell lines, primary MM cells and primary NK cells
MM1S, RPMI-8226, JJN3, H929, and U266 were cultured in RPMI-1640 medium supplemented with 10% Fetal Bovine Serum (FBS), and 1% Penicillin/Streptomycin (P/S). KHYG1 cells were supplemented with 100U/ml of IL-2. NK-92 was cultured in X-Vivo 10 media supplemented with 10% human AB serum and 500U/ml IL-2. Fresh bone-marrow was obtained from MM patients, and the CD138pos cells were sorted by positive selection from the mono-nuclear cells obtained from bone marrow of MM patients. Primary NK cells were isolated by negative selection and expanded for 14–18 days using NK MACS media supplemented with 5% human AB serum and 500U/ml IL-2. For additional details refer Supplementary Table S1.
Messenger RNA (mRNA) synthesis and electroporation
mRNA coding for CD16F158V was purchased from Trilink Biotechnology, USA. 2 × 106 KHYG1 cells were either mock electroporated or electroporated with 12.5µg CD16F158V mRNA in a total volume of 100µl using the Amaxa Nucleofector (Program: A-024) or MaxCyte GT electroporation system (Program: NK-4).
Cytotoxicity assay
Twenty-four hours post mRNA electroporation, cytotoxic functions of the electroporated NK cells were determined using a 16-h flow cytometry-based assay. Briefly, MM cells were pre-treated with 10µg/ml daratumumab for 30 min, and subsequently co-cultured with either mock electroporated or CD16F158V mRNA electroporated KHYG1. The co-cultures were stained with an anti-CD2 BV421 antibody. Cell death was determined by staining cells with Propidium Iodide (PI).
Flow cytometry and cytokine production assay
Immunophenotyping was performed according to standard protocols (Supplementary Table S2). Cell viability was determined by Annexin V-PI viability assay protocols (Supplementary Table S1). Mock electroporated or CD16F158V mRNA electroporated KHYG1 were co-cultured with daratumumab pre-treated RPMI-8226 or H929 at 1:1 Effector: Target (E:T) ratio for 16 h in 48-well plates. Culture supernatants were stored at − 80°C. Concentrations of IFN-γ and TNF-α were detected by ELISA according to the manufacturer's instructions (Supplementary Table S1).
In vivo bone marrow homing of NK cell lines
Female NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ mice were purchased and acclimated at the Maine Medical Center Research Institute animal facility. 6-week-old female mice were injected intravenously (tail-vein) with a total of 106 NK cells. KHYG1 and NK-92 cells were each stained separately with Calcein AM for 30 minutes. 100µL injection introduced 106 cells per mouse (n = 10 for KHYG1 and n = 10 for NK-92). Mice were sacrificed via exsanguination either at 1 h or 24 h post-NK cell injection to compare bone marrow homing. For exsanguination, mice were anaesthetised using 100 mg/kg ketamine and 15 mg/kg xylazine and blood (up to 1 ml) was collected into a sterile microcentrifuge tube from mice after surgical removal of their eye according to IACUC approved protocols. Bone marrow (BM) from both tibias and femurs were collected via dissection and centrifugation. Following red blood cell lysis, cells were analysed via flow cytometry. Data is presented as a double ratio: % fluorescent cells in the BM normalized to the % fluorescent cells in the blood. No adverse effects were observed during this study.
NK cell rolling assay under shear stress
Rolling assays under sheer stress on E-Selectin coated plates were performed as described previously [20]. Briefly, 80-channel microfluidic biochips (Cellix Limited) were coated with 15 µg/ml of recombinant E-selectin. Each channel was blocked with 1% BSA and incubated at 37°C for 1 h before the assay. 80µl of cell suspension were loaded onto the microchannels and the assay was run at 0.5 dyne/cm2 at room temperature using a Mirus Evo Nano Pump. Cells were monitored using an A-Plan 10×/0.25 objective of an AX10Vert.A1 Microscope. A rolling cell was defined as a cell travelling a distance corresponding to more than its diameter.
Statistics
Results were analysed using Prism v7.0. Comparisons between two groups were analysed by the Student’s paired t test. Comparisons between multiple groups were analysed by repeated measure one-way ANOVA.
Results
KHYG1 NK cells have low cell surface expression of killer inhibitory receptors and CD38
The interaction of Killer Inhibitory Receptor (KIR) and MHC Class I may have a small negative impact on ADCC mediated by daratumumab [6]. Therefore, we first investigated the expression of KIRs on primary expanded NK cells, NK-92, and KHYG1 NK cell lines. Flow cytometry-based analysis revealed that while primary expanded NK cells have high expression of KIR 2DL1, 2DL2/3, and 3DL1, both NK-92 and KHYG1 had significantly lower proportion of these inhibitory receptors (Fig. 1a, b). In contrast, KHYG1, like NK-92 had high expression of NKG2A which could be important for NK cell education (data not shown). Since high expression of CD38 can cause NK cell fratricide, we next analysed CD38 expression on the different NK cell platforms. We observed that while both primary expanded NK cells and NK-92 had very high expression of CD38, KHYG1 cells had significantly lower CD38 expression on the cell surface (Fig. 1c, d) (p = 0.0005, 0.0031). Therefore, we identified a NK cell platform with low CD38 expression, which can potentially survive daratumumab mediated fratricide upon infusion while still being able to mount a cytotoxic response against MM cells.
Expression of KIRs and CD38 on different NK cell platforms. a Representative FACS dot plot analysis of NK cell KIR inhibitory receptors (KIR2DL1, KIR2DL2/3, KIR3DL1) on primary expanded NK cells, NK-92 and KHYG1 cell line. b Expression level (MFI) of KIRs on different NK cell sources (n = 3), c representative FACS histograms of CD38 receptor on various NK cell surface; Grey histogram: FMO Control, Black Histogram: anti-CD38 staining, d MFI of CD38 expression in three NK cell platforms (n = 4) Bars represent Mean ± SEM, Results were analysed by one-way ANOVA, **p < 0.01, ***p < 0.001
CD16F158V mRNA can be efficiently electroporated in CD38low NK cells with high transgene expression and viability
Since KHYG1 cells express low levels of CD16 receptors, we next electroporated CD16F158V mRNA using the MaxCyte GT transfection system. 24-h post electroporation the viability of both Mock and CD16F158V mRNA electroporated KHYG1 cells was comparable and greater than 85% (Fig. 2a, b). Furthermore, there was a robust increase in the surface expression of CD16 in mRNA electroporated KHYG1 as compared to Mock electroporated KHYG1 (Fig. 2c) and this increased expression persisted for up to 120-h post-electroporation (Fig. 2d). Therefore, we concluded that CD38low KHYG1 cells can be very efficiently electroporated with CD16F158V mRNA to achieve high CD16F158V surface expression without any significant adverse impact on NK cell viability.
Flowcytometry based analysis of NK cell viability and CD16 receptor surface expression on electroporated KHYG1 cells. a Representative FACS dot plots analysis of KHYG1 cell viability as determined by Annexin V and Propidium Iodide staining 24 h post-electroporation. Data is representative of n = 3 independent experiments. b Summarized data for cell viability of n = 3 independent experiments. Bars represent the mean ± SEM. c Representative FACS histogram overlay of CD16 receptor surface expression on mRNA electroporated KHYG1 cells after electroporation at 24 h, 48 h, 72 h, 96 h and 120 h post electroporation. Data is representative of n = 5 independent experiments. d Summarized data CD16 expression of n = 5 independent experiments. Expression of CD16 on mock electroporated and mRNA electroporated KHYG1 cells was compared by Student’s paired t-test. Results were analysed by one-way ANOVA ****p < 0.0001
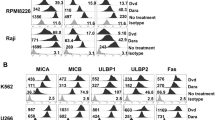
CD16F158V mRNA electroporated KHYG1 NK cells can eliminate CD38high and CD38low MM cell lines in vitro
MM patients undergoing daratumumab treatment have a downregulation of CD38 antigen, which can persist for up to 6 months post-therapy [15]. To investigate if CD16F158V expressing CD38low KHYG1 cells can target CD38high as well as CD38low MM cells, we first screened a panel of n = 5 MM cell lines. Based on CD38 immunophenotyping of MM cell lines, we selected n = 2 CD38high MM cell lines (RPMI-8226 and H929) and n = 2 CD38low MM cell lines (JJN3 and U266) for NK cell effector function assays in this study (Supplementary Fig. 1a, b). We next co-cultured the CD38high and CD38low MM cell lines with either mock electroporated KHYG1 or CD16F158V electroporated KHYG1 at an E:T ratio of 1:1 in the presence or absence of daratumumab. While daratumumab alone did not induce cell death in CD38high and CD38low MM cell lines, the addition of mock electroporated KHYG1 induced tumour cell death in both CD38high and CD38low MM cell lines. The NK cell induced tumour cell death was further increased upon co-culture with CD16F158V expressing KHYG1 (Fig. 3a).
ADCC assay against CD38high and CD38low MM cell lines using genetically modified transiently expressing CD16F158V KHYG1 NK cells. a Representative dot plot analysis of mock or mRNA electroporated KHYG1 co-cultured with MM cell lines in presence of daratumumab against MM target cell at 1:1 E:T ratio from n = 3 independent experiments. ADCC assays performed against (b) CD38high and (c) CD38low MM target cell lines using CD16+ KHYG1 effector cell alone (circle) or CD16F158V KHYG1 in combination with daratumumab (square) in a 16-h assay. Each data point represents mean of an independent experiment. Pooled data of n = 4 independent experiments for each cell line. Results were analysed by Student’s paired t test, *p < 0.05, **p < 0.01, ***p < 0.001
To further confirm our findings, we next co-cultured the CD16F158V KHYG1 cells with MM cells at multiple E:T ratios in presence or absence or daratumumab. Interestingly in the absence of daratumumab, CD38high RPMI-8226 was sensitive to CD16F158V KHYG1, and we observed an added benefit of daratumumab only at E:T ratio of 0.25:1 (p = 0.02) and 1:1 (p = 0.02) (Fig. 3b). In contrast, CD38high H929 was resistant to CD16F158V KHYG1, and the combination of daratumumab and CD16F158V KHYG1 was able to cause a significant increase in tumour cell death at an E:T ratio of 0.25:1 (p = 0.02), 0.5:1 (p = 0.01), 1:1 (p = 0.003), and 2:1 (p = 0.001) (Fig. 3b). This phenomenon was also consistent against CD38low JJN3 and the combination of daratumumab and CD16F158V KHYG1 were significantly more potent than CD16F158V KHYG1 alone at an E:T ratio of 0.5 (p = 0.04), 1:1 (p = 0.006), and 2:1 (p = 0.0004) (Fig. 3c). In the case of CD38low U266, the combination treatment elicited a significant cytotoxic response at an E:T ratio of 0.5:1 (p = 0.04) (Fig. 3c).
Collectively, the results illustrate that the combination of CD16F158V mRNA electroporated CD38low KHYG1 cells and daratumumab can therapeutically target MM cells in vitro (Fig. 3b). Towards safe cell therapy, we also tested the effect of γ-irradiation on CD16F158VKHYG1 cells and found complete elimination of KHYG1 cells within 120 h (Supplementary Fig. 2a) while still preserving CD16 expression and their cytotoxic potential 48 h post γ-irradiation (Supplementary Fig. 2b, c).
CD38low CD16F158V expressing KHYG1 NK cells in combination with daratumumab can eliminate primary MM cell in vitro with minimal NK cell fratricide
To determine the cytotoxic potential of CD16F158V expressing KHYG1 NK cells against primary MM cells, we next performed NK-MM co-culture cytotoxicity assays in vitro in the presence of daratumumab (Supplementary Fig. 3). As expected, daratumumab alone had no significant specific toxicity against primary MM cells. Next, we observed that at a low E:T ratio of 0.5:1, CD16F158V KHYG1 NK cells killed 39.2% while Mock electroporated KHYG1 eliminated only 5% of the primary MM cells in presence of daratumumab (p = 0.03) (Fig. 4a, b). This observation was also consistent and more significant at higher E:T ratios of 1:1 (p = 0.02), 2.5:1 (p = 0.01), and 5:1 (p = 0.01). KHYG1 cells also express low levels of CD38, and thus could be targeted by the CD16F158V-expressing KHYG1 cells in the presence of daratumumab, a phenomenon referred to as NK cell fratricide. During a 16-h assay we observed non-significant NK cell fratricide in the CD16F158V expressing KHYG1 in the presence of daratumumab (12.5%) as compared to CD16F158V expressing KHYG1 in absence of daratumumab (6.1%) (p = 0.29) (Fig. 4c). Since NK cell engagement with tumour cells and the ligation of CD16 receptor has been shown to promote NK cell death, we also monitored their cell death in our co-culture’s [21, 22]. At a lower E:T ratio of 0.5:1 we observed that 19.8% CD16F158V-expressing KHYG1 cells were dead upon co-culture with primary MM cells. This collateral NK cell damage was lower at higher E:T ratios of 1:1, 2.5:1 and 5:1 (Supplementary Fig. 4a, b). Of note, NK cell fratricide in CD16F158V mRNA electroporated CD38high NK-92 was higher (32%) in presence of daratumumab as compared to in absence of daratumumab (12%) (Supplementary Fig. 5). Overall, we observed potent elimination of primary patient-derived MM cells by CD16F158V expressing CD38low KHYG1 in the presence of daratumumab with minimal NK cell fratricide in vitro. Of note, the CD16F158V CD38low KHYG1 cells in the presence of daratumumab were also able to eliminate CD38low primary MM cells from a daratumumab relapsed-refractory patient ex vivo (Supplementary Fig. 6a, b).
ADCC assay against primary MM cells ex vivo using genetically modified transiently expressing CD16F158V KHYG1 NK cells. a Primary cells from MM patients were co-cultured with mock electroporated or CD16F158V mRNA electroporated KHYG1 cells in presence of daratumumab (10µg/ml). Data represents pooled percentage specific cytotoxicity results from n = 5 independent experiments. Bars represent Mean ± SEM, *p < 0.05. b Representative FACS dot plot analysis of KHYG1-MM co-culture in presence of daratumumab against Primary Myeloma target cells at various E:T ratios. c Fratricide in KHYG1 cells as estimated by Propidium Iodide after a 16-h assay in presence or absence of daratumumab. Dot plots are representative of mock and mRNA electroporated KHYG1 cell death induced by daratumumab. Graph represent results from n = 3 experiments. Bars represent Mean ± SEM. Results were analysed by one-way ANOVA, *p < 0.05
CD16F158V mRNA electroporated KHYG1 NK cells secrete IFN-γ and TNF-α upon co-culture with CD38high and CD38low MM cells
NK cells secrete a wide variety of potent effector cytokines such as IFN-γ and TNF-α which contribute to shaping anti-tumour activity. Therefore, we next investigated the cytokine production effector function of CD16F158V mRNA electroporated CD38low KHYG1 cells upon target engagement with CD38high and CD38low MM cells in the presence of daratumumab. In the absence of any target tumour cell and daratumumab, electroporation of CD16F158V mRNA per se did not induce any production of IFN-γ and TNF-α. However, in the presence of daratumumab there was a modest but significant increase in both IFN-γ (p = 0.01) and TNF-α (p = 0.003) production by CD16F158V electroporated KHYG1 as compared to mock electroporated KHYG1, even in the absence of any target tumour cell (Fig. 5a, c). Upon co-culturing CD16F158V electroporated KHYG1 with CD38high H929 MM cells, we observed a significant increase in both IFN-γ (p = 0.0001) and TNF-α (p = 0.044) production as compared to mock electroporated KHYG1 (Fig. 5b, d). The increase in IFN-γ (p = 0.046) by CD16F158V electroporated KHYG1 was also observed upon co-culture with CD38low JJN3 MM cells, albeit to a significantly lower level than upon co-culture with CD38high H929 MM (p = 0.0002) (Fig. 5b, d). There was a modest but non-significant increase in TNF-α (p = 0.15) secretion by CD16F158V electroporated KHYG1 as compared to mock electroporated KHYG1 upon co-culture with CD38low JJN3 (Fig. 5d). Therefore, we demonstrate that in presence of daratumumab the transient CD16F158V expression on CD38low KHYG1 cells can induce IFN-γ and TNF-α cytokine secretion in these cells when co-cultured with MM cells.
Cytokine production by CD16F158V mRNA electroporated KHYG1 upon co-culture with MM cell lines in combination with daratumumab. a Bar chart represents IFN-γ production by mock electroporated KHYG1 cells or CD16F158V mRNA electroporated KHYG1 cells in absence or presence of daratumumab was analysed by ELISA. b IFN-γ production by mock or electroporated KHYG1 cells upon co-culture with MM cell line i.e. H929 or JJN3 in presence of daratumumab. c Bar chart analysis depicted TNF-α production by mock electroporated KHYG1 cells or CD16F158V mRNA electroporated KHYG1 cells alone with or without daratumumab. d TNF-α production by mock or electroporated KHYG1 cells upon co-culture with MM cell line i.e. H929 or JJN3 in presence of daratumumab. Bars represent Mean ± SEM. Data represents pooled results from n = 3 independent experiments. Results were analysed by one-way ANOVA, *p < 0.05, **p < 0.01, ***p < 0.001
In vivo bone marrow trafficking potential of KHYG1 cells. a 106 cells per cell line/mouse were labeled with Calcein AM and injected separately. Bone marrow was harvested from sacrificed mice and analyzed for presence of Calcein AMpositive (CAM+) cells by flowcytometry either after (b) 1-h in circulation, or (c) 24-h in circulation. Bars represent Mean ± SEM of the fluorescently labeled cells obtained from the bone-marrow normalized to total fluorescent cells detected in both the blood and bone marrow for each mouse. Results were analysed by Student’s paired t test, *p < 0.05, **p < 0.01
KHYG1 NK cells home to the bone marrow in vivo in immunodeficient mice
Cellular NK cell immunotherapy for MM could be more successful when the NK cell can home efficiently to the bone marrow [23]. To determine if KHYG1 NK cells can home to the bone marrow microenvironment, we next studied the in vivo homing potential of KHYG1 in immunodeficient NSG mice (Fig. 6a), and compared this to NK-92, an established NK cell line which is currently being tested in multiple human clinical trials. We observed that significantly more KHYG1 cells homed to the bone marrow of NSG mice 1-h post NK cell infusion than NK-92 (Fig. 6b). Bone marrow harvested at 24-h post-infusion demonstrated that KHYG1 and NK-92 had comparable bone marrow homing in NSG mice (Fig. 6c). While the relevance of rapidly bone-marrow homed NK cells in tumour control remains to be investigated, the results show the homing potential of KHYG1 is no less inferior to that of NK-92, a NK cell line which has been investigated in several clinical trials. To corroborate our in vivo observations, we subsequently performed NK cell rolling assays under shear stress on E-Selectin coated chips and observed that KHYG1 NK cells rolled on E-Selectin coated biochips under shear stress (Video S1), while NK-92 cells had poor rolling potential (Video S2), which could be explained by the high reactivity with the HECA-452 antibody on KHYG1 cells, indicative of the presence of E-Selectin ligands (Supplementary Fig. 7a, 7b).
Discussion
The introduction of daratumumab has been a major advance in the treatment of MM and CD38 MoAb’s are likely to become a core component of MM treatment regimes in the future [12, 24, 25]. However, an undesirable consequence of the use of CD38 MoAb is the profound depletion of NK cells. Since CD38 is strongly expressed on the surface of NK cells, daratumumab induced ADCC leads to fratricide and a massive depletion of NK cells in vivo [19, 26, 27]. Nevertheless, CD38low NK cells, which constitute a minor proportion (15%) of circulating NK cells, are spared. These CD38low NK cells appear to be more proliferative and have greater cytolytic functions than their CD38high NK counterparts [19]. Moreover following ex vivo expansion CD38low NK cells isolated from daratumumab-treated patients showed synergistic anti-MM activity when combined with daratumumab in in vivo mouse models [19]. Although this a very attractive approach, the clinical processes of isolating and expanding CD38low NK cells from daratumumab-treated patients is challenging. Furthermore, blood derived primary CD38low NK cells acquire significant expression of CD38 antigen upon expansion on feeder cells (m-IL-21 K562) [19]. To overcome some of these challenges, in the present study we demonstrate the feasibility of using the CD38low NK cell line KHYG1 electroporated with CD16F158V mRNA in combination with daratumumab for treatment of MM. This strategy could provide a novel “off-the-shelf” approach of co-administering multiple infusions of CD16F158V CD38low NK cells during daratumumab therapy.
Antibody mediated CD16 receptor engagement on NK cells triggers ADCC against target tumour cells [28]. Interestingly, CD16 expression on circulating NK cells from MM patients has been shown to be downregulated [29]. MM bone marrow microenvironmental factors, such as hypoxia and TGF-β have been shown to dampen the cell surface expression of CD16 and subsequent ADCC by human NK cells [30, 31]. Furthermore, ADAM-17 dependent ectodomain shedding upon target cell antibody cross-linking can also downregulate CD16 cell surface expression on NK cells [32]. Previous studies have shown the feasibility of electroporating CD16 mRNA in primary expanded NK cells, and their subsequent ability to target Rituximab-treated lymphoma cells [33]. In this study, we used a similar mRNA electroporation-based approach to achieve high expression levels of the CD16 receptor. The steady pool availability of mRNA in the electroporated NK cells would mitigate any risks associated with downregulation of CD16 in situ, apart from addressing safety concerns related to insertion mutagenesis associated with viral transduction [34]. The CD16F158V CD38low NK cells were subsequently able to eliminate primary patient derived CD38+ MM cells with minimal fratricide of effector CD38low NK cells. A previous study demonstrating potent ADCC against a range of tumour target cells by KHYG1 NK cells virally transduced with the CD16 receptor gene supports our present observations [35].Therefore we envision the use of a mRNA based therapeutics on a GMP compliant electroporation device, such as MaxCyte system would entail a logistically less challenging production of up to 1012 CD16F158V CD38low NK cells equivalent of 1000 doses for patients when dosed at 107/kg of body weight.
Although daratumumab targets the CD38 antigen, MM patients undergoing daratumumab treatment rapidly downregulate cell surface CD38 antigen on their tumour cells within hours of their first infusion [17, 36]. Therefore, a combination of cellular therapy with daratumumab would need to be capable of targeting CD38low MM clones in vivo. In contrast to a previous study with IL-2 activated non-expanded donor-derived NK cells, which showed that daratumumab can augment alloreactive NK cell cytotoxicity only towards CD38high MM cell lines, we showed that CD16F158V CD38low NK cells in combination with daratumumab triggers a cytolytic response against both CD38high and CD38low MM cell lines in vitro [6]. One explanation for these differences could be our use of the CD16 receptor variant encoding the F158V polymorphism, which has been shown to significantly enhance response rates following treatment with the anti-CD20 antibody Rituximab [37]. However, this polymorphic variant was not shown to influence overall survival (OS) in MM patients undergoing daratumumab monotherapy in the GEN-501 and SIRUS studies [38]. In contrast, a pre-clinical study investigating the effect of F158V polymorphism in the context of a combination therapy of daratumumab and IPH-2102, a human anti-KIR MoAb, found that ex vivo IPH-2102 synergistically improved daratumumab-dependent lysis of primary myeloma cells in patients carrying the F158 allele while such a synergy was not observed in patients carrying the V158 allele [39]. Therefore, further research is necessary to better define the role of allelic variants in triggering effector functions of CD38low NK cells in the presence of daratumumab [38].
The maintenance of a high level of CD38 expression on MM cells would seem desirable to maximize the clinical success of combination therapy with CD16F158V CD38low NK cells and daratumumab as those patients with higher pre-treatment levels of CD38 expression on MM cells have had the best responses to daratumumab monotherapy [15]. Potentially, pre-treatment with clinically relevant agents such as ATRA or Panobinostat could be used to enhance CD38 expression. Pre-treatment with both agents has been shown to enhance the efficacy of daratumumab in preclinical studies and is currently under evaluation in a Phase I trial [NCT02751255] [40, 41].
IFN-γ plays an important role in mediating NK induced anti-tumour responses [42]. In our experiments, we observed that daratumumab could trigger the production of both IFN-γ and TNF-α in CD16F158V mRNA electroporated NK cells, even in the absence of target tumour cell engagement, but not in mock electroporated CD16negative KHYG1 cells. It has previously been shown that the ligation of CD38 by a MoAb can induce multiple cytokine mRNA expression in cultured peripheral blood mononuclear cells including TNF-α and IFN-γ [43]. Conceivably cross-linking and ligation of daratumumab to the CD38 antigen and CD16 receptor, both on CD38low NK cells, could trigger cytokine production. Furthermore, as IFN-γ and TNF-α production was significantly increased upon co-culture with CD38high and CD38low MM cells, the production of these immunomodulatory cytokines could be beneficial in shaping the adaptive immune response in MM patients.
NK cell homing to the bone-marrow after adoptive NK cell transfer has been shown to correlate with leukemia disease control in refractory AML patients [44]. However, similar correlative clinical data is lacking for NK cell homing and anti-MM clinical activity. The homing capacity of NK cell assumes greater importance as MM bone-marrow milieu impairs the bone marrow localization of effector NK cells [23]. In our study we demonstrate that the parental KHYG1 NK cell line can home to the bone marrow within 24 h post-infusion, at levels similar to the more clinically investigated NK cell line NK-92. This in our opinion is an observation which reflects another important facet of genetically modified cytotoxic cellular therapies which is often overlooked and ignored. Nevertheless, since CXCL12 (SDF-1) production in bone marrow is significantly down-modulated as patients progress from MGUS to MM disease onset [23], future studies with CD16F158V CD38low KHYG1 cells overexpressing the CXCR4R334X receptor could significantly enhance the bone marrow homing and therapeutic potential of these engineered cells [45].
There are several limitations to our study. We chose to use the KHYG1 NK cell line given its inherently low CD38 expression, relative to expanded primary NK cells and NK-92 cell line. CD38 is a multifunctional ectoenzyme [9], and has been described to have important roles in NK cell signalling, activation, and cellular cytotoxicity [46]. Furthermore, in murine models, CD38 has been shown to be important for granule polarization and degranulation, with NK cells from CD38knockout mice secreting lower amounts of Granzyme B upon target engagement ex vivo [16]. However, the low CD38 expression on KHYG1 cells is a “dual-edged” sword in our study, and in our opinion the high expression of the other NK cell activating receptors, such as NKG2D on KHYG1 cells would be able to compensate for this lack of CD38 mediated effector functions [47]. Presumably, as KHYG1 is not a CD38null NK cell, the low CD38 expression is enough to activate intracellular NK signalling pathways. Another drawback of our study is the limited data on the efficacy of CD16F158V CD38low NK cells against primary MM cells from daratumumab relapsed-refractory (RR) patients. While an in vitro assay with CD16F158V CD38low NK cells and daratumumab eliminated a significant proportion of primary MM cells from a daratumumab RR patient, future studies with a larger daratumumab RR patient cohort derived primary cells is imperative. The tumour microenvironment also consists of CD38pos immunosuppressive cells, such as myeloid-derived suppressor cells (MDSC) and T reg’s. Future research is necessary to investigate if the combination of CD16F158V CD38low NK cells and daratumumab can eliminate CD38pos immunosuppressive cells [48].
In conclusion, although the use of daratumumab has revolutionized the treatment of MM in the past few years, an increasing number of patients are now refractory to daratumumab [49, 50]. Moreover, as daratumumab is moved into frontline combination therapy for newly diagnosed MM patients [12], there is an unmet need to arm this “biologic” with potent “cellular armies” which are otherwise depleted in vivo. To address these therapeutic challenges, we propose the use of an “off-the-shelf” CD38low NK cell platform KHYG1, which upon electroporation with CD16F158V mRNA can be irradiated and infused in MM patients as combination therapy with daratumumab on a weekly basis. We envision that this combination of cellular therapy and daratumumab would allow potent therapeutic anti-Myeloma responses in patients in vivo.
Abbreviations
- ADCC:
-
Antibody dependent cellular cytotoxicity
- ADCP:
-
Antibody dependent cellular phagocytosis
- ADRP:
-
ADP-ribose pyrophosphate
- CDC:
-
Complement-dependent cytotoxicity
- E: T:
-
Effector: target
- IMiDs:
-
Immunomodulatory drugs
- KIR:
-
Killer inhibitory receptor
- MM:
-
Multiple myeloma
- MoAb:
-
Monoclonal antibody
- NDMM:
-
Newly diagnosed multiple myeloma
- NK:
-
Natural killer
- PI:
-
Propidium iodide
References
Sarkar S, Chauhan S, Stikvoort A, Natoni A, Daly J, Henderson R, Mutis T, O'Dwyer ME (2018) CD38(low) natural killer cells transiently expressing CD16(F158V) m-RNA potentiates the therapeutic activity of daratumumab against multiple myeloma with minimal effector NK cell fratricide. Blood. https://doi.org/10.1182/blood-2018-99-118926
Palumbo A, Anderson K (2011) Multiple myeloma. N Engl J Med 364(11):1046–1060. https://doi.org/10.1056/NEJMra1011442
van de Donk N, Richardson PG, Malavasi F (2018) CD38 antibodies in multiple myeloma: back to the future. Blood 131(1):13–29. https://doi.org/10.1182/blood-2017-06-740944
van de Donk N, Yong K (2019) Oral proteasome inhibitor maintenance for multiple myeloma. Lancet 393(10168):204–205. https://doi.org/10.1016/S0140-6736(18)33128-3
Fast LD, Hansen JA, Newman W (1981) Evidence for T cell nature and heterogeneity within natural killer (NK) and antibody-dependent cellular cytotoxicity (ADCC) effectors: a comparison with cytolytic T lymphocytes (CTL). J Immunol 127(2):448–452
Mahaweni NM, Bos GMJ, Mitsiades CS, Tilanus MGJ, Wieten L (2018) Daratumumab augments alloreactive natural killer cell cytotoxicity towards CD38+ multiple myeloma cell lines in a biochemical context mimicking tumour microenvironment conditions. Cancer Immunol Immunother 67(6):861–872. https://doi.org/10.1007/s00262-018-2140-1
Hatjiharissi E, Xu L, Santos DD, Hunter ZR, Ciccarelli BT, Verselis S, Modica M, Cao Y, Manning RJ, Leleu X, Dimmock EA, Kortsaris A, Mitsiades C, Anderson KC, Fox EA, Treon SP (2007) Increased natural killer cell expression of CD16, augmented binding and ADCC activity to rituximab among individuals expressing the Fc{gamma}RIIIa-158 V/V and V/F polymorphism. Blood 110(7):2561–2564. https://doi.org/10.1182/blood-2007-01-070656
Leo R, Boeker M, Peest D, Hein R, Bartl R, Gessner JE, Selbach J, Wacker G, Deicher H (1992) Multiparameter analyses of normal and malignant human plasma cells: CD38++, CD56+, CD54+, cIg+ is the common phenotype of myeloma cells. Ann Hematol 64(3):132–139
Funaro A, Malavasi F (1999) Human CD38, a surface receptor, an enzyme, an adhesion molecule and not a simple marker. J Biol Regul Homeost Agents 13(1):54–61
Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, Spicka I, Hungria V, Munder M, Mateos MV, Mark TM, Qi M, Schecter J, Amin H, Qin X, Deraedt W, Ahmadi T, Spencer A, Sonneveld P, Investigators C (2016) Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med 375(8):754–766. https://doi.org/10.1056/NEJMoa1606038
Dimopoulos MA, San-Miguel J, Belch A, White D, Benboubker L, Cook G, Leiba M, Morton J, Ho PJ, Kim K, Takezako N, Moreau P, Kaufman JL, Sutherland HJ, Lalancette M, Magen H, Iida S, Kim JS, Prince HM, Cochrane T, Oriol A, Bahlis NJ, Chari A, O'Rourke L, Wu K, Schecter JM, Casneuf T, Chiu C, Soong D, Sasser AK, Khokhar NZ, Avet-Loiseau H, Usmani SZ (2018) Daratumumab plus lenalidomide and dexamethasone versus lenalidomide and dexamethasone in relapsed or refractory multiple myeloma: updated analysis of POLLUX. Haematologica 103(12):2088–2096. https://doi.org/10.3324/haematol.2018.194282
Mateos MV, Dimopoulos MA, Cavo M, Suzuki K, Jakubowiak A, Knop S, Doyen C, Lucio P, Nagy Z, Kaplan P, Pour L, Cook M, Grosicki S, Crepaldi A, Liberati AM, Campbell P, Shelekhova T, Yoon SS, Iosava G, Fujisaki T, Garg M, Chiu C, Wang J, Carson R, Crist W, Deraedt W, Nguyen H, Qi M, San-Miguel J, Investigators AT (2018) Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med 378(6):518–528. https://doi.org/10.1056/NEJMoa1714678
Facon T, Kumar S, Plesner T, Orlowski RZ, Moreau P, Bahlis N, Basu S, Nahi H, Hulin C, Quach H, Goldschmidt H, O'Dwyer M, Perrot A, Venner CP, Weisel K, Mace JR, Raje N, Attal M, Tiab M, Macro M, Frenzel L, Leleu X, Ahmadi T, Chiu C, Wang J, Van Rampelbergh R, Uhlar CM, Kobos R, Qi M, Usmani SZ, Investigators MT (2019) Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med 380(22):2104–2115. https://doi.org/10.1056/NEJMoa1817249
van de Donk N, Usmani SZ (2018) CD38 antibodies in multiple myeloma: mechanisms of action and modes of resistance. Front Immunol 9:2134. https://doi.org/10.3389/fimmu.2018.02134
Nijhof IS, Casneuf T, van Velzen J, van Kessel B, Axel AE, Syed K, Groen RW, van Duin M, Sonneveld P, Minnema MC, Zweegman S, Chiu C, Bloem AC, Mutis T, Lokhorst HM, Sasser AK, van de Donk NW (2016) CD38 expression and complement inhibitors affect response and resistance to daratumumab therapy in myeloma. Blood 128(7):959–970. https://doi.org/10.1182/blood-2016-03-703439
Rah SY, Kwak JY, Chung YJ, Kim UH (2015) ADP-ribose/TRPM2-mediated Ca2+ signaling is essential for cytolytic degranulation and antitumor activity of natural killer cells. Sci Rep 5:9482. https://doi.org/10.1038/srep09482
Krejcik J, van de Donk N (2018) Trogocytosis represents a novel mechanism of action of daratumumab in multiple myeloma. Oncotarget 9(72):33621–33622. https://doi.org/10.18632/oncotarget.26098
Usmani SZ, Khan I, Chiu C, Foureau D, Druhan LJ, Rigby K, Casneuf T, Sasser AK (2018) Deep sustained response to daratumumab monotherapy associated with T cell expansion in triple refractory myeloma. Exp Hematol Oncol 7:3. https://doi.org/10.1186/s40164-018-0096-7
Wang Y, Zhang Y, Hughes T, Zhang J, Caligiuri MA, Benson DM, Yu J (2018) Fratricide of NK cells in daratumumab therapy for multiple myeloma overcome by ex vivo-expanded autologous NK cells. Clin Cancer Res 24(16):4006–4017. https://doi.org/10.1158/1078-0432.CCR-17-3117
Natoni A, Farrell ML, Harris S, Falank C, Kirkham-McCarthy L, Macauley MS, Reagan MR, O'Dwyer M (2019) Sialyltransferase inhibition leads to inhibition of tumor cell interactions with E-selectin, VCAM1, and MADCAM1, and improves survival in a human multiple myeloma mouse model. Haematologica. https://doi.org/10.3324/haematol.2018.212266
Srpan K, Ambrose A, Karampatzakis A, Saeed M, Cartwright ANR, Guldevall K, De Matos G, Onfelt B, Davis DM (2018) Shedding of CD16 disassembles the NK cell immune synapse and boosts serial engagement of target cells. J Cell Biol 217(9):3267–3283. https://doi.org/10.1083/jcb.201712085
Warren HS, Kinnear BF (1999) Quantitative analysis of the effect of CD16 ligation on human NK cell proliferation. J Immunol 162(2):735–742
Ponzetta A, Benigni G, Antonangeli F, Sciume G, Sanseviero E, Zingoni A, Ricciardi MR, Petrucci MT, Santoni A, Bernardini G (2015) Multiple myeloma impairs bone marrow localization of effector natural killer cells by altering the chemokine microenvironment. Cancer Res 75(22):4766–4777. https://doi.org/10.1158/0008-5472.CAN-15-1320
Lokhorst HM, Plesner T, Laubach JP, Nahi H, Gimsing P, Hansson M, Minnema MC, Lassen U, Krejcik J, Palumbo A, van de Donk NW, Ahmadi T, Khan I, Uhlar CM, Wang J, Sasser AK, Losic N, Lisby S, Basse L, Brun N, Richardson PG (2015) Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med 373(13):1207–1219. https://doi.org/10.1056/NEJMoa1506348
Usmani SZ, Weiss BM, Plesner T, Bahlis NJ, Belch A, Lonial S, Lokhorst HM, Voorhees PM, Richardson PG, Chari A, Sasser AK, Axel A, Feng H, Uhlar CM, Wang J, Khan I, Ahmadi T, Nahi H (2016) Clinical efficacy of daratumumab monotherapy in patients with heavily pretreated relapsed or refractory multiple myeloma. Blood 128(1):37–44. https://doi.org/10.1182/blood-2016-03-705210
Casneuf T, Xu XS, Adams HC 3rd, Axel AE, Chiu C, Khan I, Ahmadi T, Yan X, Lonial S, Plesner T, Lokhorst HM, van de Donk N, Clemens PL, Sasser AK (2017) Effects of daratumumab on natural killer cells and impact on clinical outcomes in relapsed or refractory multiple myeloma. Blood Adv 1(23):2105–2114. https://doi.org/10.1182/bloodadvances.2017006866
Nahi H, Chrobok M, Gran C, Lund J, Gruber A, Gahrton G, Ljungman P, Wagner AK, Alici E (2019) Infectious complications and NK cell depletion following daratumumab treatment of multiple myeloma. PLoS One 14(2):e0211927. https://doi.org/10.1371/journal.pone.0211927
Wang W, Erbe AK, Hank JA, Morris ZS, Sondel PM (2015) NK cell-mediated antibody-dependent cellular cytotoxicity in cancer immunotherapy. Front Immunol 6:368. https://doi.org/10.3389/fimmu.2015.00368
Fauriat C, Mallet F, Olive D, Costello RT (2006) Impaired activating receptor expression pattern in natural killer cells from patients with multiple myeloma. Leukemia 20(4):732–733. https://doi.org/10.1038/sj.leu.2404096
Sarkar S, Germeraad WT, Rouschop KM, Steeghs EM, van Gelder M, Bos GM, Wieten L (2013) Hypoxia induced impairment of NK cell cytotoxicity against multiple myeloma can be overcome by IL-2 activation of the NK cells. PLoS One 8(5):e64835. https://doi.org/10.1371/journal.pone.0064835
Trotta R, Dal Col J, Yu J, Ciarlariello D, Thomas B, Zhang X, Allard J 2nd, Wei M, Mao H, Byrd JC, Perrotti D, Caligiuri MA (2008) TGF-beta utilizes SMAD3 to inhibit CD16-mediated IFN-gamma production and antibody-dependent cellular cytotoxicity in human NK cells. J Immunol 181(6):3784–3792. https://doi.org/10.4049/jimmunol.181.6.3784
Romee R, Foley B, Lenvik T, Wang Y, Zhang B, Ankarlo D, Luo X, Cooley S, Verneris M, Walcheck B, Miller J (2013) NK cell CD16 surface expression and function is regulated by a disintegrin and metalloprotease-17 (ADAM17). Blood 121(18):3599–3608. https://doi.org/10.1182/blood-2012-04-425397
Carlsten M, Levy E, Karambelkar A, Li L, Reger R, Berg M, Peshwa MV, Childs RW (2016) Efficient mRNA-based genetic engineering of human NK cells with high-affinity CD16 and CCR7 augments rituximab-induced ADCC against lymphoma and targets NK cell migration toward the lymph node-associated chemokine CCL19. Front Immunol 7:105. https://doi.org/10.3389/fimmu.2016.00105
Hacein-Bey-Abina S, Garrigue A, Wang GP, Soulier J, Lim A, Morillon E, Clappier E, Caccavelli L, Delabesse E, Beldjord K, Asnafi V, MacIntyre E, Dal Cortivo L, Radford I, Brousse N, Sigaux F, Moshous D, Hauer J, Borkhardt A, Belohradsky BH, Wintergerst U, Velez MC, Leiva L, Sorensen R, Wulffraat N, Blanche S, Bushman FD, Fischer A, Cavazzana-Calvo M (2008) Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest 118(9):3132–3142. https://doi.org/10.1172/JCI35700
Kobayashi E, Motoi S, Sugiura M, Kajikawa M, Kojima S, Kohroki J, Masuho Y (2014) Antibody-dependent cellular cytotoxicity and cytokine/chemokine secretion by KHYG-1 cells stably expressing FcgammaRIIIA. Immunol Lett 161(1):59–64. https://doi.org/10.1016/j.imlet.2014.05.004
Krejcik J, Frerichs KA, Nijhof IS, van Kessel B, van Velzen JF, Bloem AC, Broekmans MEC, Zweegman S, van Meerloo J, Musters RJP, Poddighe PJ, Groen RWJ, Chiu C, Plesner T, Lokhorst HM, Sasser AK, Mutis T, van de Donk N (2017) Monocytes and granulocytes reduce CD38 expression levels on myeloma cells in patients treated with daratumumab. Clin Cancer Res 23(24):7498–7511. https://doi.org/10.1158/1078-0432.CCR-17-2027
Weng WK, Levy R (2003) Two immunoglobulin G fragment C receptor polymorphisms independently predict response to rituximab in patients with follicular lymphoma. J Clin Oncol 21(21):3940–3947. https://doi.org/10.1200/JCO.2003.05.013
van de Donk N, Casneuf T, Di Cara A, Parren PW, Zweegman S, van Kessel B, Lokhorst HM, Usmani SZ, Lonial S, Richardson PG, Chiu C, Mutis T, Nijhof IS, Sasser AK (2019) Impact of Fc gamma receptor polymorphisms on efficacy and safety of daratumumab in relapsed/refractory multiple myeloma. Br J Haematol 184(3):475–479. https://doi.org/10.1111/bjh.15122
Nijhof IS, Lammerts van Bueren JJ, van Kessel B, Andre P, Morel Y, Lokhorst HM, van de Donk NW, Parren PW, Mutis T (2015) Daratumumab-mediated lysis of primary multiple myeloma cells is enhanced in combination with the human anti-KIR antibody IPH2102 and lenalidomide. Haematologica 100(2):263–268. https://doi.org/10.3324/haematol.2014.117531
Garcia-Guerrero E, Gogishvili T, Danhof S, Schreder M, Pallaud C, Perez-Simon JA, Einsele H, Hudecek M (2017) Panobinostat induces CD38 upregulation and augments the antimyeloma efficacy of daratumumab. Blood 129(25):3386–3388. https://doi.org/10.1182/blood-2017-03-770776
Nijhof IS, Groen RW, Lokhorst HM, van Kessel B, Bloem AC, van Velzen J, de Jong-Korlaar R, Yuan H, Noort WA, Klein SK, Martens AC, Doshi P, Sasser K, Mutis T, van de Donk NW (2015) Upregulation of CD38 expression on multiple myeloma cells by all-trans retinoic acid improves the efficacy of daratumumab. Leukemia 29(10):2039–2049. https://doi.org/10.1038/leu.2015.123
Wang R, Jaw JJ, Stutzman NC, Zou Z, Sun PD (2012) Natural killer cell-produced IFN-gamma and TNF-alpha induce target cell cytolysis through up-regulation of ICAM-1. J Leukoc Biol 91(2):299–309. https://doi.org/10.1189/jlb.0611308
Ausiello CM, Urbani F, la Sala A, Funaro A, Malavasi F (1995) CD38 ligation induces discrete cytokine mRNA expression in human cultured lymphocytes. Eur J Immunol 25(5):1477–1480. https://doi.org/10.1002/eji.1830250554
Grzywacz B, Moench L, McKenna D Jr, Tessier KM, Bachanova V, Cooley S, Miller JS, Courville EL (2019) Natural killer cell homing and persistence in the bone marrow after adoptive immunotherapy correlates with better leukemia control. J Immunother 42(2):65–72. https://doi.org/10.1097/CJI.0000000000000250
Levy E, Reger R, Segerberg F, Lambert M, Leijonhufvud C, Baumer Y, Carlsten M, Childs R (2019) Enhanced bone marrow homing of natural killer cells following mRNA transfection with gain-of-function variant CXCR4(R334X). Front Immunol 10:1262. https://doi.org/10.3389/fimmu.2019.01262
Sconocchia G, Titus JA, Mazzoni A, Visintin A, Pericle F, Hicks SW, Malavasi F, Segal DM (1999) CD38 triggers cytotoxic responses in activated human natural killer cells. Blood 94(11):3864–3871
Suck G, Branch DR, Smyth MJ, Miller RG, Vergidis J, Fahim S, Keating A (2005) KHYG-1, a model for the study of enhanced natural killer cell cytotoxicity. Exp Hematol 33(10):1160–1171. https://doi.org/10.1016/j.exphem.2005.06.024
Krejcik J, Casneuf T, Nijhof IS, Verbist B, Bald J, Plesner T, Syed K, Liu K, van de Donk NW, Weiss BM, Ahmadi T, Lokhorst HM, Mutis T, Sasser AK (2016) Daratumumab depletes CD38+ immune regulatory cells, promotes T cell expansion, and skews T cell repertoire in multiple myeloma. Blood 128(3):384–394. https://doi.org/10.1182/blood-2015-12-687749
Pick M, Vainstein V, Goldschmidt N, Lavie D, Libster D, Gural A, Grisariu S, Avni B, Ben Yehuda D, Gatt ME (2018) Daratumumab resistance is frequent in advanced-stage multiple myeloma patients irrespective of CD38 expression and is related to dismal prognosis. Eur J Haematol 100(5):494–501. https://doi.org/10.1111/ejh.13046
Minarik J, Novak M, Flodr P, Balcarkova J, Mlynarcikova M, Krhovska P, Pika T, Pikalova Z, Bacovsky J, Scudla V (2017) CD38-negative relapse in multiple myeloma after daratumumab-based chemotherapy. Eur J Haematol 99(2):186–189. https://doi.org/10.1111/ejh.12902
Acknowledgements
The authors would like to thank the Flowcytometry Core Facility at National University of Ireland Galway (NUIG), Ireland.
Funding
This research was supported by a Sponsored Research Agreement from ONK Therapeutics Ltd., Ireland to National University of Ireland Galway. Subhashis Sarkar received a Post-doctoral Fellowship from ONK Therapeutics Ltd. Michaela R. Reagan is supported in part by a Research Scholar Grant, RSG-19-037-01-LIB from the American Cancer Society, and the NIH, P20GM121301.
Author information
Authors and Affiliations
Contributions
SS, SKSC, JD, HF and MRR performed experiments. SS, SKSC, JD and HF analysed data. AN, RH, EN, DS, JH, and MRR assisted with experiments. SS and MOD designed the project. SS and MOD wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Subhashis Sarkar: ONK Therapeutics Ltd.: Research funding; Michael O'Dwyer: Abbvie: Membership on advisory committee; Celgene: Membership on advisory committee, and research funding; Bristol Myers Squibb (BMS): Research funding; Glycomimetics: Research funding; ONK Therapeutics Ltd.: Equity Ownership, Membership on Board of Directors, and research funding; Janssen: Membership on advisory committees, and research funding; Michaela R. Reagan: ONK Therapeutics Ltd.: Research funding. A provisional patent application was filed by Subhashis Sarkar and Michael O'Dwyer regarding the CD16 work described in the paper. All other authors declare no conflict of interest.
Ethical approval
All experiments utilizing primary cells from MM patients were conducted in accordance with the ethical standards of the Clinical Research Ethics Committee University Hospital Galway and the 1964 Declaration of Helsinki. The collection of bone marrow samples from MM patients was approved by Clinical Research Ethics Committee University Hospital Galway on June 14, 2017 (Study no. C.A.1519) All experiments utilizing blood samples from healthy donors were conducted in accordance with the ethical standards of the Clinical Research Ethics Committee University Hospital Galway and the 1964 Declaration of Helsinki. The collection of blood samples from healthy volunteers was approved by Clinical Research Ethics Committee University Hospital Galway on August 4, 2017 (Study no. C.A.1805) Animal research experiments to examine in vivo bone marrow homing were performed at the Maine Medical Center Research Institute with approval from the institutional animal care and use committee (IACUC); (Protocol #MR1508), an (Association for assessment and accrediation of laboratory animal care) AAALAC international accredited program. Approval for the experiments in this manuscript was issued by the Maine Medical Center Research Institute (MMCRI) Institutional Animal care and use committee (IACUC) on September 2, 2016.
Informed consent
NK cells were freshly isolated from peripheral blood samples of anonymous volunteer healthy donors at the University Hospital Galway, Ireland. Oral informed consent was obtained from all blood donors to the use of their blood for scientific purposes. Bone Marrow samples were provided by the Haematology Unit of University Hospital Galway, Galway from MM patients who had provided written consent for remaining samples to be used for immunology related research.
Animal source
Female NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ mice (Stock# 005557) were purchased at 4-weeks of age from Jackson Laboratory (Bar Harbor, ME) and acclimated at the Maine Medical Center Research Institute animal facility for at least two weeks prior being randomly assigned to each group for experiments.
Cell line authentication
KHYG1 was a kind gift from Dr. Armand Keating, University of Toronto (Canada) and the cell line was authenticated by STR profiling on 06/06/2017. MM1S, RPMI-8226, JJN3, H929, and U266, were obtained from American Type Culture Collection (ATCC) (Manassas, VA, USA). NK-92 was purchased from Deutsche Sammlung von Mikcroorganismen and Zellkulturen (DSMZ) (Braunschweig, Germany) The cell lines were initially grown and cryopreserved into multiple aliquots of master cell bank (MCB). All the experiments were performed with cells at low passage numbers (≤ 10). Mycoplasma was routinely tested.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Note on previous publication: Part of this work was presented as a poster at the annual conference of the American Society of Haematology (ASH) 1–4 December 2018, San Diego, USA (Session-Myeloma: Pathophysiology and Pre-Clinical Studies, excluding Therapy: Poster II). The accompanying abstract was published in a special edition of Blood [1].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sarkar, S., Chauhan, S.K.S., Daly, J. et al. The CD38low natural killer cell line KHYG1 transiently expressing CD16F158V in combination with daratumumab targets multiple myeloma cells with minimal effector NK cell fratricide. Cancer Immunol Immunother 69, 421–434 (2020). https://doi.org/10.1007/s00262-019-02477-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-019-02477-8