Abstract
Objectives
To estimate radiation dose and the associated risk of secondary cancer risk related to percutaneous cryoablation (PCA) and follow-up imaging in a cohort of patients treated for small renal masses (SRMs).
Methods
A total of 149 patients underwent PCA for a SRM at our institution. Based on CT dose reports, we calculated the mean effective dose for a CT-guided PCA procedure and post-ablative follow-up CT. Applying follow-up recommendations by a multidisciplinary expert panel, we calculated the total radiation dose for the PCA procedure and the CT surveillance program corresponding to a minimal and preferable follow-up regime (5-year vs 10-year). Estimates of the lifetime attributable cancer risk for different age groups were calculated based on the cumulative effective dose based on the latest BEIR VII report.
Results
Total dose for the PCA treatment and follow-up CTs amounted to 174 and 294 mSv for a minimal and preferable protocol, respectively. Follow-up CTs accounted for the majority of the total effective dose for the minimal and preferable protocol (89% vs 94%). CT fluoroscopy contributed only to a limited amount of the total radiation dose for the minimal and preferable protocol (1.8% vs 1.1%). A 70-year-old male undergoing PCA treatment has a lifetime attributable cancer risk of 0.8% (1 in 131) when completing the preferable follow-up protocol. The same regimen in a 30-year-old female results in a lifetime attributable risk of cancer of 3.4% (1 in 29).
Conclusion
Radiation dose and the associated risk of secondary cancer are high for patients with SRMs undergoing PCA and post-ablative follow-up imaging in particular in younger patients. Radiation exposure in the PCA procedure itself accounts for only a limited amount of the total radiation. Radiologists and clinicians must strive to implement radiation dose saving measures especially with respect to the follow-up regime.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The widespread utilization of cross-sectional imaging has contributed to a greater detection of incidental small renal masses (SRMs), defined as a renal neoplasm 4 cm or less in greatest dimension, corresponding to WHO stage of T1a [1]. Hence, more SRMs are diagnosed at an earlier stage, and consequently the treatment strategy in many patients has shifted from radical nephrectomy to a nephron-sparing approach such as partial nephrectomy or image-guided percutaneous thermal ablation (PTA).
Additionally, active surveillance (AS) for select patients has increasingly been utilized.
Until recently PTA was reserved to mainly elderly patients who due to significant comorbidities were poor surgical candidates or had a short life expectancy. Recent studies reporting on outcomes after percutaneous cryoablation (PCA) for cT1 renal cell carcinomas find PCA to be competitive with surgical resection and with a lower complication rate [2, 3]. Thus, PCA is expected to play an important role in the future management of SRMs, and guidelines are likely to include PCA as a viable treatment modality for SRMs. In contrast to surgical resection, where the initial success of the treatment can be assessed by evaluating the surgical margins, the success of PCA is based on the appearance of the ablation zone on initial follow-up imaging [4]. Imaging surveillance plays a critical role not only for ascertaining residual/persistent disease, but also for detecting recurrent disease where salvage PCA often can be performed with good results [5].
Currently, there are no well-established guidelines across radiological and urological associations in terms of follow-up regime or biomarkers for PTA-treated SRMs. Nonetheless, an international multidisciplinary consensus project based on the Delphi method has provided recommendations for follow-up of focal therapy in renal masses (RMs) [6]. CT is the first-choice modality as well as the number one option for PCA procedural image-guidance. However, serial use of CT remains contentious because of the radiation-induced risk of secondary cancer [7]. Secondary malignancy due to ionizing radiation incurred as part of a PCA regime for SRMs has only been scarcely investigated and is becoming increasingly relevant with broadening PCA indication.
Thus, the present study aims to estimate the total radiation dose, as well as the size of its subcomponents, in patients with SRMs undergoing PCA and follow-up according to aforementioned recommendations; moreover, to estimate the risk of secondary malignancy.
Materials and methods
This study was approved by the hospital Institutional Review Board and because electronic medical patient records were not assessed, requirements for formal patient informed consent were waived.
Patient population
The study population consisted of consecutively enrolled patients (n = 149) undergoing PCA for a biopsy confirmed SRM at Aarhus University Hospital, Denmark in the period from 2016 to 2018. All patients were identified in a prospectively registered database. Patient demographics, tumor characteristics and procedural data are shown in detail in Table 1.
Follow-up recommendations after focal therapy of renal masses
A consensus project based on the Delphi method was conducted in 2015 and involved an international multidisciplinary panel of 76 experts which formulated recommendations for key topics regarding follow-up after focal therapy of renal masses (hereafter Delphi follow-up) [6]. These key topics addressed questions regarding imaging follow-up including intervals, imaging modality, and assessment of metastases (Table 2). Based on these recommendations, the number of CTs of the abdomen and thorax needed for a minimal and preferable follow-up protocol for focal therapy of RMs can be determined. This amounts to 5 and 7 vs 10 and 12 CTs of the abdomen and thorax for the minimal and preferable protocol, respectively.
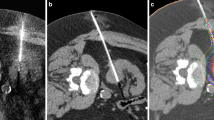
Percutaneous renal cryoablation procedure
A Siemens SOMATOM Definition AS CT system was used in the scanner suite alongside a BTG system (BTG, London, UK) for cryoablation. The procedure was performed by one of four radiologists with between 1 and 10 years of dedicated ablation experience. During the procedure, patients were in general anesthesia, and in a prone-oblique position.
For planning and target facilitation, a contrast-enhanced triple-phase CT scan of the kidneys was conducted. If needed, an intraprocedural coaxial biopsy of the tumor was performed using an 18-gauge semiautomatic needle prior to cryoprobe placement. Real-time CT fluoroscopy was used to guide needle placement. The number and type of cryoprobes were determined by the attending radiologist. If necessary, hydrodissection with sterile saline was carried out to displace thermally sensitive structures. At the discretion of the attending radiologist, truncated helical acquisitions covering the RM were acquired during placement of cryoprobes to confirm their position. In all cases truncated helical acquisitions for monitoring of the size and location of the ice ball were performed during two treatment cycles of freeze–thaw treatment (in general 10 min freeze, 8 min thaw, 10 min freeze) at 4-min intervals for a total of four acquisitions to confirm extension of the ice ball at least 5 mm beyond the tumor margin. The duration of each cycle and the power of each probe could be adjusted as to prevent adjacent vulnerable organ injury or inadequate ice ball coverage. Fluoroscopy was conducted as sequential scans at 5.0 mm slice thickness with 120 kV and a starting point of 40 mAs, which could be increased according to patient size. Images for the triple-phase CT were obtained as helical acquisitions at 2.0 mm slice thickness using standard CT technique (120 kV peak and approximately 200 mAs) with dose modulation using automatic exposure control. The same parameters were used in addition to a current of 150 mAs for the truncated CT acquisitions.
Post treatment follow-up
At the authors’ institution follow-up imaging after PCA is conducted with CT as first-choice modality. Residual/persistent disease is defined as the presence of any radiological enhancement at 3 months radiological follow-up, and recurrence as a new (after a period of non-enhancement) enhancing or growing lesion, inside or in the margin of the ablated zone [6]. Patients were scanned across four different CT scanners, each with at least 64 detector rows and with dose modulation using automatic exposure control provided by the vendor (Supplementary Table 1). The same scanning protocol for each CT scanner was consistently used in both the initial follow-up scan at three months as well as in all subsequent. All protocols consisted of helical acquisitions performed before, and after intravenous administration of low-osmolar iodinated contrast material injected at a rate of 4 mL/s to obtain images in the corticomedullary and nephrographic phase. Reconstructions with a 2.0 mm slice width were generated.
Thus scans were performed in accordance with Delphi recommendations with the notable exception that we employed a limited scan range covering the kidneys.
As part of the diagnostic workup at our institution a baseline CT of the thorax is performed. However, due to the low risk of metastatic disease we have not routinely performed CT thorax as part of the follow-up. Thus, for the purposes of this study, we used data from the US CT Dose Index Registry including diagnostic reference levels and achievable doses based on a CT thorax with IV contrast in 111,898 patients [8].
Dose estimations
Dose-length product (DLP) from the dose protocol page stored in our PACS system was retrieved for all 149 patients.
Radiation dose data registered as part of the CT scan performed during the cryoablation procedure were divided into three components: triple-phase planning CT, truncated helical acquisitions, and CT fluoroscopy.
Average DLP for patients was calculated for the three components for the PCA procedure and the follow-up CT. The DLP (= 374 mGy cm) for the 50th percentile for achievable dose of a thorax CT with IV contrast from the US CT Dose Index Registry was used as an estimate of average patient DLP for this analysis. Effective dose was estimated by multiplying the DLP with a conversion factor of 0.018 mSv/mGy cm [9]. Assuming that patients are compliant with postprocedural follow-up estimations were made of the cumulative radiation exposure of each theoretical follow-up protocol.
Furthermore, the association between patient BMI and DLP of the CT upper abdomen was assessed by Pearson correlation analysis.
Estimating radiation-induced cancer risk
The BEIR VII model is a method to estimate the risk of radiation exposure-associated solid organ malignancy or leukemia secondary due to CT scans. It is based primarily on epidemiologic studies of survivors of the atomic bombings in Hiroshima and Nagasaki, and on studies of individuals with occupational and medical exposures to radiation. The number of additional cases of cancer attributable to a single dose of 0.1 Gy (100 mSv) is estimated for different age groups, and data are based on the incidence of all cancer types. As a non-threshold model it allows estimation of a quantitative risk of cancer that is directly proportional to the dose received and is additive [10].
For assessment of lifetime attributable risk (LAR) of contracting a cancer due to CT radiation exposure, we used a calculator endorsed by the American College of Radiology [11]. This calculator is based on the BEIR VII report model incorporating age- and sex adjusted risk factors to estimate the risk for different age groups of patients undergoing PCA of a SRM.
Results
The patients evaluated (n = 149) were on average 65.3 (SD 10.9) years and had a mean BMI of 27.9 (SD 5.6). The mean DLP and effective dose from the PCA procedure, follow-up CT of the upper abdomen and thorax CT data are listed in Table 3. Table 3 also shows the dose incurred by the follow-up CTs as well as the total dose conforming to a minimal and preferable protocol.
The mean effective dose estimated for the PCA procedure, follow-up CT of the upper abdomen and thorax CT was 18.1 (SD 7.8), 17.4 (SD 9.9) and 6.7 (SD unavailable) mSv, respectively. Marked difference in the mean cumulative grand total effective dose was seen between the minimal and preferable protocol as the dose came close to doubling (69%) from 174 to 294 mSv. Furthermore, the follow-up CTs accounted for the majority of the total effective dose for the minimal and preferable protocol (89% vs 94%). In addition, CT fluoroscopy contributed to a small part (18%) of the radiation due to the PCA procedure seen in isolation as well as a limited amount of the total radiation dose for the minimal and preferable protocol (1.8% vs 1.1%).
The additional cancer risks for different age groups are illustrated in Fig. 1. For a 70-year-old male a LAR for the minimal and preferable follow-up protocol was 0.5% (1 in 208) and 0.8% (1 in 131), respectively, whereas the LAR for a 40-year-old male was 1.1% (1 in 91) and 1.7% (1 in 57), respectively. Thus, the LAR more than doubled for a 40-year-old man undergoing PCA compared to a 70-year-old. As expected, women had a higher LAR of cancer compared with men according to the BEIR VII model where a 30-year-old female had a LAR of 3.4% for the preferable protocol in comparison to 2.3% for a male, respectively. Moreover, as expected from the linear-quadratic BEIR VII model the LAR is seen approaching a linear decrease beyond the age of 40 years.
Estimated lifetime attributable risk of secondary malignancy when conducting PCA of a SRM in combination with each theoretical follow-up protocol stratified according to age. Red and green; minimal and preferable protocol for males, respectively. Blue and yellow; minimal and preferable protocol for females, respectively
As anticipated, the Pearson correlation between BMI and DLP of the CT upper abdomen was strong (r = 0.78, p < 0.05).
Discussion
Based on in-house data and a well-recognized CT Dose registry we estimated the mean total radiation dose, as well as the size of its subcomponents, incurred in PCA treatment of SRMs including surveillance imaging using Delphi follow-up recommendations. Our population had a BMI comparable to the US population [12], and we found a high effective dose of 294 mSv for the preferable follow-up regime. Radiation exposure owing to the PCA procedure itself accounts for only a limited amount of the total radiation incurred for both the minimal and the more extended preferable protocol.
To put things into perspective the average effective dose from a chest X-ray, abdominal X-ray, CT chest, CT abdomen, and CT abdomen (dedicated liver) amounts to 0.1, 0.7, 7, 8, and 15 mSv, respectively. Moreover, an individual is exposed to 3 mSv of background radiation per year, and as such the total radiation for the preferable protocol amounts to more than a lifetime exposure to background radiation [13].
Based on the BEIR VII model an effective dose of 294 mSv translates into a 1:57 (1.7%) and 1:41 (2.4%) risk for a 40-year-old male and female, respectively, of developing cancer as a result of PCA treatment according to a preferable follow-up protocol. Besides imaging surveillance, there are currently no available biomarkers that would be able to detect treatment failure or disease recurrence. The rationality in offering follow-up imaging surveillance is predicated on the assumption that early detection of recurrence provides greater opportunities for potentially curative interventions and/or allows delivery of systemic therapies that may be more effective in the context of low-volume disease. Available treatment regimes in RCC accommodates these assumptions [14]. However, as shown in the present study the relative high radiation dose and risk of secondary cancer for patients undergoing PCA treatment questions the appropriateness of exposing especially younger patients to that magnitude of radiation. Especially in the light of the constant refinement of the PCA procedure where recent reports find the rate of recurrent disease as low as 3.2% following PCA of T1 RCC [3]. In the case of testicular cancer, which like T1a RCC has a highly favorable primary cancer prognosis, a prior study found that CT surveillance incurred a median cumulative effective dose of 125.1 mSv, which is well below our dose estimates for a preferable protocol. This prompted the recommendation that every effort should be made to develop low-dose CT or alternatives to limiting ionizing radiation in this patient group [15].
The benefits of primary surgery in terms of overall survival in the treatment of SRMs in younger patients (< 75 years) has been firmly established [16]. When counseling the patient with respect to the optimal treatment strategy there are a number of parameters that must be taken into account, including radiation dose. As highlighted, a well-recognized advantage of thermal ablation compared to surgery is the low complication rate. In a study that estimated 10-year cumulative radiation exposure incurred during different kidney cancer surveillance protocols after surgery found the mean cumulative incurred radiation exposure to be 33.6 mSv, which is close to 1/10 of the dose of the preferable follow-up regime presented in this study [17]. Thus, when evaluating the safety and overall survival of thermal ablation vs. surgery, the high radiation dose incurred in follow-up imaging in the former is a concern. Regarding active surveillance in SRMs, as with follow-up imaging after thermal ablation, there exists no clear consensus with respect to imaging protocol. In both cases serial imaging is needed, and when employing CT a single-phase scan is sufficient for active surveillance which isn’t the case following thermal ablation. Based on the recommendations from a recent review of imaging protocols for active surveillance in SRMs [18] and extrapolation of data from the present study the estimated mean dose for patients adhering to active surveillance for 10 years amounts to 75 mSv.
AS is primarily an option in the group of elderly and infirm patients with a limited expected lifespan for whom comorbidity risks outweigh oncologic risks. Since it has been established that many radiation-induced cancers will not appear until more than 20 years after exposure the above estimated radiation dose incurred in AS seems to be of minor concern [19]. The evidence to support AS for SRMs in the young with a long-life expectancy is lacking. Nevertheless it has been argued that in a well-informed and reliable young patient with a low-risk mass for whom a period of AS presents significant value, an interval of close clinical monitoring can be a safe and reasonable approach [20]. However, the burden of life-long annual imaging follow-up also needs to be taken into consideration which further questions the appropriateness of AS in younger patient groups.
Prior studies have evaluated the radiation dose incurred as part of the procedural part of PCA of RMs and found an effective radiation dose using CT-guided targeting in the range of 30–40 mSv; this is in line with the results of the present study [21]. Kim et al. demonstrated how PCA can be managed using ultrasound-guided targeting (instead of CT fluoroscopy) and CT-guided ice ball monitoring in combination to reduce radiation. The study found acceptable short-term (mean 10.1 months) local tumor control for RCC with a mean procedural dose of 12.1 mSv [21].
Only one previous study has evaluated the radiation exposure of CT-guided ablation procedure as well as CT surveillance [22]. Prior to the publication of the Delphi follow-up recommendations Eisenberg et al. identified 30 in-house CT-guided RFA cases performed for a RM and estimated average per-case effective dose. For estimating the effective dose in surveillance CT, prior data on effective doses for single-phase abdomino-pelvic CT scans in patients with testicular cancer were extrapolated to gauge the dose incurred in an average triple-phase post-RFA follow-up CT scan. The institutional follow-up CT regime of Eisenberg et al. encompassed 13 triple-phase CT scans over a 10-year-period which is similar to the preferable protocol in the Delphi follow-up, but the authors did not incorporate thorax CT for assessment of lung metastases as recommended. Eisenberg et al. found that the mean RFA procedural effective dose of 27.7 mSv and the mean cumulative effective dose due to RFA of one tumor and follow-up CTs added up to 305 mSv in total.
The ratio between procedural and dose of follow-up CTs where the latter make up the bulk of the effective dose is comparable with our results. The similar dose shown for the preferable follow-up regime in our study can at least in part be explained by the inclusion of thorax CT, as the average dose of the CT of the abdomen was lower consistent with our limited scan range covering the kidneys.
In terms of the PCA procedure itself our data have shown that fluoroscopy for cryoprobe targeting constitutes a minor part of the total effective dose. Taking into consideration that ultrasound for cryoprobe targeting is not as precise as CT in delineating tumor and determining the position the cryoprobe tip we believe that in terms of diminishing the dose it is more prudent to focus on reducing the number of phases of the planning scan as well as the number and scan range of truncated helical acquisitions during freezing. Furthermore, Leng et al. demonstrated that it is feasible to use images obtained from CT acquisitions at 50% of the original dose level in CT monitoring of PCA [23].
The above options for dose reduction are certainly important to consider pertaining to the “as low as reasonably achievable” (ALARA) principle advocated by radiological societies, especially for RCC patients with conditions such as Birt–Hogg–Dubé syndrome and von Hippel-Lindau disease who are likely to need multiple PCAs. However, our results show that the greatest potential impact on the grand total dose for a PCA treatment for both a minimal and preferable protocol can be achieved by altering the follow-up regime.
For dose reduction purposes, beyond reducing the number of contrast phases and frequency of CT imaging, it is prudent to optimize scanning parameters such as automatic tube current modulation. In general, larger patients require the use of more X-ray photons than do smaller patients to achieve similar levels of image quality in CT. With regards to some CT systems it is important that the operator-selected image quality settings in relation to automatic tube current modulation be adjusted to the patient’s habitus to avoid a very high dose in larger patients [24]. Additionally, it should be emphasized that follow-up imaging can be performed without ionizing radiation by employing MRI. MRI should be considered as a substitute for CT, at least in younger patients. Nonetheless, it is important to note that the use of MRI is limited by the lack of available equipment, expertise and the relative high cost, and consequently may not be a viable option at many institutions. Conversely CT is more available, and CT equipment and protocols are continually being refined to reduce the radiation dose received by patients while aiming to maintain or improve image quality where especially iterative reconstruction techniques have shown promise [25]. In fact, even without iterative reconstruction CT with an approximate fivefold dose reduction has been shown to be non-inferior in the detection of metastatic pulmonary nodules compared to standard dose CT [26]. Thus, switching to a low-dose protocol for post-ablation follow-up for pulmonary metastasis can readily be implemented at no greater cost and with a resulting substantial total dose reduction. Interestingly, no studies have investigated whether low-dose CT can be used interchangeably with standard dose CT in the detection of post-ablation RCC recurrence. On the basis of our data, we believe there is a pressing need for studies clarifying this issue. If low-dose CT is feasible for this purpose it would have a major impact on the radiation dose incurred in SRM post-ablation follow-up.
There are limitations to this study. Our single-institution study may not reflect the patient populations and PCA practice in other institutions. Moreover, the follow-up CT protocols applied in our institution may not reflect practice elsewhere as we used follow-up CTs for estimation with a limited scan range covering only the kidneys. Nevertheless, employing scan data of abdomino-pelvic CTs would only have increased the mean total effective dose estimates. The risk calculations of secondary malignancy in the BEIR VII model are extrapolated from follow-up of atomic bomb survivors, and those exposed to occupational radiation which may not be generalizable to medical imaging. In addition, it is not universally accepted that the linear no-threshold model holds for low doses (less than 100 mSv). However, the estimated radiation doses in our study for both the minimal and preferable protocol are well above the 100 mSv threshold, which is generally considered significant for cancer risk by the American Association of Physicists in Medicine [27, 28]. Despite the limitations of the BEIR VII model, it currently represents the longest follow-up of patients exposed to low levels of radiation and is currently the favored model available [29].
In conclusion, the present study demonstrated that the mean total effective radiation dose and the associated risk of secondary cancer are significantly elevated for patients with SRMs undergoing PCA and post-ablative follow-up in particular in younger patients. Radiologists and clinicians must strive to implement radiation dose saving measures in the treatment and in particular the follow-up regime.
Abbreviations
- SRM:
-
Small renal mass
- PTA:
-
Percutaneous thermal ablation
- PCA:
-
Percutaneous cryoablation
- RM:
-
Renal mass
- DLP:
-
Dose-length product
- LAR:
-
Lifetime attributable risk
- ALARA:
-
As low as reasonably achievable
- AS:
-
Active surveillance
References
Gill, I. S., Aron, M., Gervais, D. A. & Jewett, M. A. S. Clinical practice. Small renal mass. N. Engl. J. Med. 362, 624–634 (2010).
Breen, D. J., King, A. J., Patel, N., Lockyer, R. & Hayes, M. Image-guided Cryoablation for Sporadic Renal Cell Carcinoma: Three- and 5-year Outcomes in 220 Patients with Biopsy-proven Renal Cell Carcinoma. Radiology 289, 554–561 (2018).
Aoun, H. D. et al. Percutaneous Cryoablation of Renal Tumors: Is It Time for a New Paradigm Shift? J. Vasc. Interv. Radiol. 28, 1363–1370 (2017).
Grand, D., Dupuy, D., Mayo-Smith, W. & Iannuccilli, J. Percutaneous Ablation for Small Renal Masses—Imaging Follow-Up. Seminars in Interventional Radiology vol. 31 050–063 (2014).
Okhunov, Z. et al. Salvage Percutaneous Cryoablation for Locally Recurrent Renal-Cell Carcinoma After Primary Cryoablation. J. Endourol. 30, 632–637 (2016).
Zondervan, P. J. et al. Follow-up after focal therapy in renal masses: an international multidisciplinary Delphi consensus project. World Journal of Urology vol. 34 1657–1665 (2016).
Brenner, D. J. Slowing the increase in the population dose resulting from CT scans. Radiat. Res. 174, 809–815 (2010).
Kanal, K. M. et al. U.S. Diagnostic Reference Levels and Achievable Doses for 10 Adult CT Examinations. Radiology 284, 120–133 (2017).
Huda, W., Ogden, K. M. & Khorasani, M. R. Converting dose-length product to effective dose at CT. Radiology 248, 995–1003 (2008).
Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation & National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII _ Phase 2. (National Academies Press, 2006).
X-Ray Risk. https://www.xrayrisk.com. Accessed Dec 2019.
Fryar, C. D., Kruszon-Moran, D., Gu, Q. & Ogden, C. L. Mean Body Weight, Height, Waist Circumference, and Body Mass Index Among Adults: United States, 1999–2000 Through 2015–2016. Natl. Health Stat. Report. 1–16 (2018).
Elster, A. D. Effective Doses in Radiology and Diagnostic Nuclear Medicine: A Catalog. Yearbook of Diagnostic Radiology vol. 2010 214–217 (2010).
Atkins, M. B. & Tannir, N. M. Current and emerging therapies for first-line treatment of metastatic clear cell renal cell carcinoma. Cancer Treat. Rev. 70, 127–137 (2018).
Sullivan, C. J. et al. Radiation exposure from diagnostic imaging in young patients with testicular cancer. Eur. Radiol. 25, 1005–1013 (2015).
Sun, M. et al. Management of localized kidney cancer: calculating cancer-specific mortality and competing risks of death for surgery and nonsurgical management. Eur. Urol. 65, 235–241 (2014).
Lin, Y.-K., Gettle, L. & Raman, J. D. Significant variability in 10-year cumulative radiation exposure incurred on different surveillance regimens after surgery for pT1 renal cancers: yet another reason to standardize protocols? BJU Int. 111, 891–896 (2013).
Liaw, C. W., Winoker, J. S. & Mehrazin, R. Imaging Protocols for Active Surveillance in Renal Cell Carcinoma. Curr. Urol. Rep. 19, 81 (2018).
Brenner, D. J. & Hall, E. J. Cancer risks from CT scans: now we have data, what next? Radiology 265, 330–331 (2012).
Cacciamani, G., Fay, C., Park, D., Alotaibi, M. & Gill, I. S. Active Surveillance for Small Renal Masses in Young Patients. Eur Urol Focus 2, 569–571 (2016).
Kim, D. K., Won, J. Y. & Park, S. Y. Percutaneous cryoablation for renal cell carcinoma using ultrasound-guided targeting and computed tomography-guided ice-ball monitoring: radiation dose and short-term outcomes. Acta Radiologica 028418511879817 (2018) doi:10.1177/0284185118798175.
Eisenberg, J. D. et al. Radiation Exposure From CT-Guided Ablation of Renal Masses: Effects on Life Expectancy. American Journal of Roentgenology vol. 204 335–342 (2015).
Leng, S. et al. Radiation dose reduction for CT-guided renal tumor cryoablation. AJR Am. J. Roentgenol. 196, W586–91 (2011).
Martin, C. J. & Sookpeng, S. Setting up computed tomography automatic tube current modulation systems. J. Radiol. Prot. 36, R74–R95 (2016).
Willemink, M. J. & Noël, P. B. The evolution of image reconstruction for CT—from filtered back projection to artificial intelligence. European Radiology vol. 29 2185–2195 (2019).
Muangman, N., Maitreesorrasan, N. & Totanarungroj, K. Comparison of low dose and standard dose MDCT in detection of metastatic pulmonary nodules. J. Med. Assoc. Thai. 94, 215–223 (2011).
AAPM Position Statements, Policies and Procedures - Details. https://www.aapm.org/org/policies/details.asp?id=439&type=PP.
Dauer, L. T. et al. Review and evaluation of updated research on the health effects associated with low-dose ionising radiation. Radiat. Prot. Dosimetry 140, 103–136 (2010).
Shah, D. J., Sachs, R. K. & Wilson, D. J. Radiation-induced cancer: a modern view. Br. J. Radiol. 85, e1166–73 (2012).
Funding
Funding was provided by Sundhed, Region Midtjylland, Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The scientific guarantor of this publication is Tommy K. Nielsen. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The present study was in part funded by the Health Research Fund of Central Denmark Region. No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board. Institutional Review Board approval was obtained. Methodology: retrospective study performed at one institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borgbjerg, J., Bylling, T., Andersen, G. et al. CT-guided cryoablation of renal cancer: radiation burden and the associated risk of secondary cancer from procedural- and follow-up imaging. Abdom Radiol 45, 3581–3588 (2020). https://doi.org/10.1007/s00261-020-02527-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02527-1