Abstract
Purpose
In this pilot trial, we investigate the safety of CT-guided high-dose-rate brachytherapy (HDR-BT) as a local ablative treatment for renal masses not eligible for resection or nephrectomy.
Methods
We investigated renal function after irradiation by HDR-BT in 16 patients (11 male, 5 female, mean age 76 years) with 20 renal lesions (renal cell carcinoma n = 18; renal metastases n = 2). Two patients had previous contralateral nephrectomy and two had ipsilateral partial nephrectomy. Six lesions had a hilar localization with proximity to the renal pelvis and would have not been favorable for thermal ablation. Renal function loss was determined within 1 year after HDR-BT by renal scintigraphy and laboratory parameters. Further investigations included CT and MRI every 3 months to observe procedural safety and local tumor control. Renal function tests were analyzed by Wilcoxon’s signed rank test with Bonferroni–Holm correction of p-values. Survival and local tumor control underwent a Kaplan–Meier estimation.
Results
Median follow-up was 22.5 months. One patient required permanent hemodialysis 32 months after repeated HDR-BT and contralateral radiofrequency ablation of multifocal renal cell carcinoma. No other patient developed a significant worsening in global renal function and no gastrointestinal or urogenital side effects were observed. Only one patient died of renal tumor progression. Local control rate was 95% including repeated HDR-BT of two recurrences.
Conclusion
HDR-BT is a feasible and safe technique for the local ablation of renal masses. A phase II study is recruiting to evaluate the efficacy of this novel local ablative treatment in a larger study population.
Zusammenfassung
Ziel
In dieser Pilotstudie wurde die Sicherheit der computertomographie-(CT-)geführten „High-dose-rate“-Brachytherapie (HDR-BT) bei der lokalablativen Behandlung von nichtresektablen Nierenraumforderungen untersucht.
Methoden
Es wurde die Nierenfunktion von 16 Patienten (11 männlich, 5 weiblich, mittleres Alter 76 Jahre) mit 20 Nierenläsionen (Nierenzellkarzinom n = 18; Nierenmetastasen n = 2) nach Bestrahlung mittels HDR-BT untersucht. Jeweils 2 Patienten hatten eine vorangegangene kontralaterale Nephrektomie bzw. ipsilaterale Teilresektion. Sechs Läsionen lagen zentral am Nierenbecken und waren technisch nicht suffizient durch eine thermische Ablation behandelbar. Die Nierenfunktion wurde innerhalb eines Jahres nach HDR-BT durch Nierensequenzszintigraphien sowie Laborwerte bestimmt. Weitere Untersuchungen beinhalteten CT und Magnetresonanztomographie (MRT) alle 3 Monate zur Beobachtung der Sicherheit und Tumorkontrolle. Die Nierenfunktionstests wurden mit dem Wilcoxon-Test mit Bonferroni-Holm-Korrektur der p-Werte analysiert. Überleben und lokale Tumorkontrolle wurden mit der Kaplan-Meier-Schätzung ausgewertet.
Ergebnisse
Das mediane Follow-up betrug 22,5 Monate. Ein Patient benötigte permanente Hämodialyse 32 Monate nach wiederholter HDR-BT und kontralateraler Radiofrequenzablation bei multifokalem Nierenzellkarzinom. Keine weiteren Patienten zeigten eine signifikante Verschlechterung der globalen Nierenfunktion. Es wurden keine gastrointestinalen oder urogenitalen Nebenwirkungen beobachtet. Ein Patient verstarb durch lokale Tumorprogression. Die lokale Kontrollrate betrug – einschließlich wiederholter HDR-BT von zwei Rezidiven – 95%.
Schlussfolgerung
Die HDR-BT ist eine technisch machbare und sichere Technik zur lokalen Ablation von Nierentumoren. Momentan rekrutiert eine Phase-II-Studie eine größere Patientenpopulation, um die Effektivität dieser neuen Anwendung genauer zu untersuchen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with locally confined renal masses will most likely undergo partial or total nephrectomy if clinically eligible [1]. However, up to 25% percent of patients might present with a contraindication to surgery [2]. In these cases, local therapies such as radiofrequency ablation (RFA), cryoablation (CA), or microwave ablation (MWA) are an alternative option with less treatment-associated morbidity [3, 4].
Computed tomography-guided interstitial high-dose-rate brachytherapy (HDR-BT) is an ablation technique utilizing single-fraction irradiation by an iridium-192 source which is inserted in the tumor via percutaneously applied catheters. In contrary to thermal ablation techniques, HDR-BT has no technical restriction in terms of tumor size or proximity to larger vessels or heat-vulnerable structures [5,6,7].
The most common application of CT-guided HDR-BT today is the radioablation of primary and secondary liver malignancies, especially hepatocellular carcinoma and colorectal liver metastases [8, 9]. A recent study also investigated the application of HDR-BT to adrenal gland malignancies [10].
To our knowledge, this new local ablative technique has not yet been thoroughly evaluated for the ablation of renal masses. Thus, we initiated a phase I trial to report the feasibility and safety of HDR-BT applied for renal masses in patients not eligible for surgery.
Patients and methods
Patient cohort
The institutional review board approved the study prior to recruitment and all patients gave oral and written informed consent.
Our study comprises 16 patients with 20 renal masses (11 male, 5 female, mean age 76 years) treated by HDR-BT at the Department of Radiology. Prior clinical evaluation was conducted by the Department of Urology and feasibility to undergo surgery was omitted in all patients (inadequate clinical performance status n = 6; imminent hemodialysis after surgery n = 5; metastatic disease n = 5). Tumor entities include renal cell carcinoma (RCC; n = 18) and metastases of colorectal carcinoma (CRC; n = 1) or hepatocellular carcinoma (HCC; n = 1). Bilateral and multifocal RCC were present in one patient. Two patients had prior contralateral nephrectomy and ipsilateral partial nephrectomy, respectively. Concomitant kidney diseases were polycystic kidney disease (n = 1) and horseshoe kidney (n = 1).
In summary, inclusion criteria were:
-
i.
renal masses with indication for local treatment (renal metastases and histologically proven or suspected renal cell cancer),
-
ii.
ineligibility to undergo surgical treatment (see above)
-
iii.
sufficient performance status to safely undergo interventional treatment under conscious sedation,
-
iv.
written informed consent,
Exclusion criteria included:
-
i.
life expectancy <6 months,
-
ii.
estimated dose exposure to organs at risk (OAR) above local clinical standards (see below)
-
iii.
insufficient laboratory parameters for interventional treatment (hemoglobin <6.0 mmol/l, thrombocyte count <50 Gpt/l, international normalized ratio >1.5, partial thromboplastin time >50 s)
The patient characteristics are displayed in Table 1.
Radioablation by HDR brachytherapy
To place brachytherapy catheters in a renal mass, the following procedure was performed under conscious sedation using midazolam and fentanyl: The tumor was punctured percutaneously by an 18 G coaxial needle under CT fluoroscopy (Aquillion, Canon Medical Systems, Neuss, Germany). Then, a 6F angiographic catheter sheath (Terumo Radifocus® Introducer II, Terumo Europe, Leuven, Belgium) was inserted through a guide wire (Amplatz SuperStiff™, Boston Scientific, Marlborough, USA). In a last step, a 6F irradiation catheter (afterloading catheter, Primed® medical GmbH, Halberstadt, Germany) was placed inside the catheter sheath. For the treatment of larger or complex-shaped lesions, multiple catheter placements were required for a sufficient geometry of the ablation zone while reducing the radiation exposure of adjacent organs. Twenty lesions were ablated in the study, requiring a total of 43 catheter placements in 16 patients and a median of 2 catheters per lesion (range 1–5). Typical time for the interventional procedure was 10 to 40 min depending on the complexity of the lesions and percutaneous access. Pretreatment medication included an antiemetic prophylaxis consisting of 8 mg dexamethasone and 8 mg odansetron administered intravenously. A routine antibiotic prophylaxis was not required.
After catheter placement, a multi-slice CT visualized the catheter position(s) in the renal mass and the imaging data (axial slices with 3 mm thickness) was transferred to the irradiation planning system (Oncentra® Brachy, Elekta Instrument AB, Stockholm, Sweden). The gross tumor volume (GTV) was delineated in a 3D treatment plan by hand and an automated algorithm generated a 5 mm safety margin to define the clinical target volume (CTV). As the brachytherapy catheters were fixed within the tumor eliminating inaccuracy of respiratory movement, the CTV was directly adopted as the planning target volume (PTV). Radioablation was then achieved by a single fraction of 15 Gy prescribed to the PTV [11]. In local recurrences of a previously irradiated lesion, a dose escalation for the PTV with 20 Gy was applied [12]. Dose constraints for organs at risk (OAR) were D1CC ≤14 Gy for stomach and small bowel, D1CC ≤18 Gy for large bowel and V5Gy ≤66% for the liver, referring to contemporary literature [13,14,15].
After completion of the irradiation procedure, catheters and sheaths were removed, leaving a gelatin sponge in the catheter path to prevent bleeding. Patients continued fasting and bed rest for at least 4 h. To exclude early complications, ultrasonography of the treatment area was conducted 1 to 2 h after catheter removal. Scheduled hospitalization was 2 days after treatment. Post-treatment workup included standard laboratory evaluation prior to discharge. Interventional complications were recorded and assessed by the Clavien–Dindo classification [16], radiation-induced adverse events were classified by the Common Terminology Criteria for Adverse Events (CTCAE 4.02).
A typical imaging data set for HDR brachytherapy is depicted in Fig. 1.
Image data set of Computed tomography-guided brachytherapy for a renal cell carcinoma: a Computed tomography fluoroscopy, image-guided insertion of a coaxial needle for biopsy and subsequent catheter placement; b diagnostic computed tomography displaying the catheter sheath within the renal mass; c irradiation plan depicting the tip of the iridium-192 source (red line) and corresponding isodoses for radioablation
Imaging
Pretreatment planning was performed by magnetic resonance imaging (MRI) of the kidneys comprising high resolution T1 and T2 sequences (with and without fat saturation) as well as dynamic contrast-enhanced studies. Additional tumor sites were assessed by contrast-enhanced computed tomography (CT) of the thorax and abdomen.
During follow-up, all patients were scheduled for MRI of the kidneys every 3 months and additional CT if necessary. All imaging datasets were then reviewed for local and locoregional recurrences.
Renal function tests
Primary endpoint of the study was renal function loss within 1 year after HDR-BT.
Laboratory evaluations were conducted prior to CT-guided HDR-BT as well as 3 days, 3 months, 6 months, and 12 months after treatment, including creatinine serum levels with calculation of the estimated glomerular filtration rate (eGFR) according to the Chronic Kidney Disease Epidemiology Collaboration (CKI-EPI) formula. Furthermore, patients underwent dynamic renal scintigraphy with technetium-99 mercaptoacetyltriglycine (Tc99m-MAG3) for determination of the tubular extraction rate (TER) at baseline and 3 months, 6 months, and 12 months after HDR-BT. The tracer extraction was quantified separately for both kidneys to assess the ipsilateral and contralateral effects of radiation exposure by HDR-BT on renal function.
Statistical analysis
Statistical analysis of all data was performed using IBM SPSS Statistics 22.0® (IBM Corp., Armonk, NY, USA). Measures for safety (e.g., acute and chronic adverse events) and efficacy (e.g., technical success) underwent descriptive statistics. Survival and local tumor control were calculated by the Kaplan–Meier estimation. All renal function tests were processed as non-parametric variables and testing was performed utilizing Wilcoxon’s signed rank test with Bonferroni-Holm correction. All tests were carried out two-sided. In data interpretation, p ≤ 0.05 was determined as statistically significant.
Results
Treatment characteristics
Besides two renal metastases (CRC n = 1; HCC n = 1), all incidental lesions were proven histologically by prior or concomitant core needle biopsy as renal cell carcinomas (RCC n = 18). Local tumor stage was T1a (<4 cm) in 15 lesions and T1b and greater (>4 cm) in 5 lesions. Six lesions had a central localization in or close to the renal hilum and were not eligible for thermal ablation.
Mean tumor size was 3.5 cm (range 1.2–9.4 cm), requiring a mean number of 2 catheters for sufficient dose application (range 1–5). Including a 5 mm safety margin, a mean effective tumor-surrounding dose (CTV/D100) of 16.37 ± 2.18 Gy was achieved. Mean irradiation time was 1325 ± 858 s (22.1 ± 14.3 min).
Concomitant treatments were Y90 radioembolization for liver-dominant metastatic colorectal cancer (n = 1) or synchronous liver metastases of RCC (n = 1). One patient underwent prior HDR-BT for multifocal hepatocellular carcinoma in liver cirrhosis.
A summary of patient and treatment characteristics is given in Table 1.
Renal function analysis
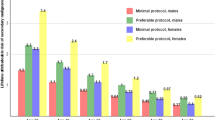
The glomerular filtration rate was assessed by laboratory evaluation of serum creatinine (eGFR, estimated GFR according to the CKI-EPI formula) at baseline and 3 days after CT-guided brachytherapy, as well as every 3 months during follow-up. Medians of eGFR demonstrated a decrease from 71 ml/min (range 26–125 ml/min) at baseline to 58 ml/min (23–88 ml/min) after 12 months as demonstrated by the boxplot in Fig. 2. The reduction of eGFR after HDR-BT did not meet statistical significance at any time point (Wilcoxon signed rank test with Bonferroni–Holm correction). The corresponding KDOQI stages had a median of 2 from baseline to 9 months follow. At 12 months, the median KDOQI stage decreased to 3 without statistical significance (p = 0.315). An overview of eGFR and KDOQI stages is given in Fig. 2.
Tubular excretion rate was determined by renal scintigraphy (TER) at baseline and 3 months, 6 months, and 12 months after HDR-BT. Medians for TER decreased from 156 ml/min (range 97–340 ml/min) at baseline to a minimum of 108 ml/min (range 108–142 ml/min) at 12 months follow-up. Correspondingly, median ipsilateral TER was reduced from 52 ml/min (range 37–100 ml/min) at baseline to 33 ml/min (range 5–100 ml/min) at 12 months follow-up (p = 0.285). The median contralateral TER demonstrated an increase from 51 ml/min (range 38–63 ml/min) to a maximum of 95 ml/min (range 57–95 ml/min) 12 months after HDR-BT (p = 0.285). A summary of ipsilateral and contralateral TER measurements is depicted in Fig. 3.
Boxplots representing TER (ml/min) at baseline (TER pre), 3 months (TER 3M), 6 months (TER 6M), and 12 months (GFR 12M) after HDR-BT separated by ipsilateral (HDR-BT of renal mass) and contralateral kidney. Reference line represents 50 ml/min to visualize the stepwise decrease in ipsilateral kidney function after HDR-BT and compensatory increase of contralateral kidney function
Clinical risk assessment
In our cohort, one puncture-related adverse event was observed in a patient suffering hematothorax from bleeding of an intercostal artery. The patient underwent subsequent ligation and was monitored for 24 h at the intensive care unit (ICU). The patient received 600 ml of packed red blood cells during surgery and antibiotic prophylaxis with ampicillin/sulbactam for 7 days. This single event was rated as grade IIIb according to the Clavien–Dindo classification and results in a patient-based risk of 6.3% and lesion-based risk of 5% for 30-day morbidity. No 30-day mortality or re-hospitalization was observed. Median duration of hospitalization was 2 days (range 2–9 days). Chronic adverse events occurred in one patient requiring permanent hemodialysis 32 months after HDR-BT with prior RFA of the contralateral kidney and a baseline eGFR of 26 ml/min. All other patients retained sufficient renal function and did not require hemodialysis during follow-up. Furthermore, no significant gastrointestinal or urogenital side effects (CTCAE grade 3/4 events) or infectious complications were observed after treatment. Overall, the patient-based risk of chronic adverse events was 6.3%.
Survival and local tumor control
Median overall survival was 27.0 months. Censoring extrarenal causes of death (malignant disease in other organs n = 4; aftermath of a fall in elderly patients n = 2; cardiopulmonary events n = 1; intracranial bleeding n = 1), the median of overall survival was not reached and mean overall survival accounted for 65.6 months. The Kaplan–Meier chart for survival is displayed in Fig. 4.
Kaplan–Meier estimation for overall survival; lines represent any causes of death: dotted line including extra-renal causes, e.g., cardiovascular events, versus kidney-related causes of death (solid line), e.g., tumor progression of renal cell carcinoma. Median follow-up for survival was 22.5 months
Local tumor control after CT-guided HDR-BT was reviewed throughout a median imaging follow-up of 14.5 months. Local recurrence was defined as tumor growth from baseline imaging. We observed a total of 3 local recurrences in 20 tumors, equaling a primary tumor control rate (pLTC) of 85%. Two of these recurrences were successfully treated by repeated HDR-BT, with dose escalation from 15 to 20 Gy yielding a secondary local tumor control rate of 95% (sLTC).
Figure 5 depicts the Kaplan–Meier estimation for local tumor control.
Discussion
The primary endpoint of this prospective observational trial was to assess renal function loss after CT-guided HDR-BT as a local ablative treatment for renal masses. As a secondary endpoint, we investigated procedural safety and local tumor control in HDR-BT.
Early and late adverse events
Neither acute radiation-induced effects on renal function nor any gastrointestinal side effects were observed within 30 days after HDR-BT. One heavily pretreated patient with known risk factors (treatment of bilateral tumors and severe kidney dysfunction at baseline [17]) required hemodialysis more than 2.5 years after brachytherapy. All other patients retained renal function without requiring hemodialysis during follow-up and without significant deterioration of eGFR—a benefit previously described for thermal ablation techniques [18]. In contrast, a decline in global kidney function of approximately 10% is commonly seen after partial nephrectomy and typically attributed to perioperative ischemia and nephron loss [19]. In the surgical setting, an ipsilateral decrease in renal function of up to 24.4% was reported, while contralateral compensation accounted for only 2.3% after partial nephrectomy. Correspondingly, the increase in contralateral volume was marginal [20, 21]. Our results suggest a functional hypertrophy in the contralateral kidney after CT-guided HDR-BT of ipsilateral renal masses as indicated by scintigraphic measurement of the tubular excretion rate (Fig. 3). Although these changes obviously originate from ipsilateral function loss, little is known about the specific etiology of radiation-induced nephropathy especially in single-fraction brachytherapy [22]. However, we hypothesize that the underlying mechanisms may contribute to a favorable safety profile of radioablation by HDR-BT in the kidney and our clinical follow-up implies that HDR-BT is safe in terms of global renal function.
Procedural complication rates in percutaneous radiofrequency ablation or cryoablation range from 13.0 to 23.0%, while major complications are reported in 4.3 and 4.5% of patients in larger cohorts, respectively [3, 23, 24]. Acute morbidity by CT-guided catheter placement was comparably low, including one case of puncture-associated bleeding (Clavien–Dindo grade IIIb; 6.3%).
HDR-BT compared to other ablation techniques
In our study population, one quarter of all renal masses exceeded the recommendations for thermal ablation (T1b; >4 cm) according to the recent guideline of the European Association of Urology (EAU) and nearly one third had a hilar localization that would prohibit radiofrequency ablation. Including these cases not favorable for thermal ablation techniques due to size or location, HDR-BT could demonstrate a primary local tumor control (pLTC) of 85%, and secondary tumor control (sLTC) increased to 95% after treatment of recurrences by repeated HDR-BT. In summary, local recurrence was comparable to radiofrequency ablation and cryoablation, as meta-analyses report local tumor control of 87.1 to 94.8% in small renal masses (T1a; <4 cm) and thermal ablation techniques [2, 25]. Inferior outcomes in radiofrequency ablation or cryoablation are reported for larger or central lesions [24, 26]. The LTC achieved in our study is also consistent with results of phase I/II trials investigating stereotactic body radiotherapy (SBRT) as another form of high-dose conformal irradiation in renal cell cancer (LTC ranging from 83 to 98%) [27]. Excellent results in SBRT were seen in T1a as well as T1b tumors, while toxicities were limited to grade 1 or 2 events in 18 to 78% of patients [28,29,30].
Advantages of SBRT include its noninvasiveness compared to the interventional approach in thermal ablation and interstitial brachytherapy, unless fiducial markers need to be placed for tumor tracking. Although procedural morbidity in interventional techniques is generally low, most reports of ablative treatments are restricted to lesions in favorable localizations, as complication rates rise with proximity to the renal pelvis [31,32,33]. Comparing both irradiation techniques, dose fall-off and elimination of respiratory motion by catheter fixation in single-fraction HDR-BT might reduce the impairment of healthy renal tissue while fractionating and dose distribution in SBRT might decrease radiation damage to adjacent bowel structures (comparative data only available for treatment planning in other abdominal organs) [34,35,36]. As HDR-BT and SBRT are not standardized in terms of dosage and fractionation, evaluation of study results is difficult.
In summery, these findings underline the potential of HDR-BT, as many technical restrictions known for thermal ablation techniques (e.g., heat-sink effect) do not apply for radioablation and no radiation-induced side effects on the renal pelvis and ureter were observed in our study. Given these technical restrictions of thermal ablation, irradiation by HDR-BT (as well as SBRT) might not only be a substitute for the ablation of small renal masses (T1a), but may present a favorable treatment for the local ablation of central or large renal tumors (T1b) compared to radiofrequency ablation or cryoablation [37, 38].
Limitations
Our study comprises only a small cohort of patients with predominantly higher age and pre-existing renal morbidity in more than one third. Furthermore, two patients underwent treatment for renal metastases as a part of systemic dissemination in advanced tumors. Hence, our study population might have been more susceptible to adverse events. Thus, safety seems to be favorable in CT-guided HDR-BT based on the presented clinical data. As tumor control might not last in all patients and statistical analysis of cofactors (e.g., tumor stage) cannot be conducted in our small cohort, upcoming investigations should focus on long-term follow-up and a dedicated analysis of efficacy depending on tumor size (T1a vs. T1b).
Conclusion
CT-guided HDR-BT is a feasible technique for the local ablation of renal masses with encouraging results for safety and local tumor control, even in masses not eligible for thermal ablation. A phase II study is currently recruiting to evaluate the efficacy of this novel local ablative treatment in a larger study population.
References
Kim DY, Wood CG, Karam JA (2014) Treating the two extremes in renal cell carcinoma: management of small renal masses and cytoreductive nephrectomy in metastatic disease. Am Soc Clin Oncol Educ Book e214–21. https://doi.org/10.14694/EdBook_AM.2014.34.e214
Thompson RH, Atwell T, Schmit G, Lohse CM, Kurup AN, Weisbrod A et al (2015) Comparison of partial nephrectomy and percutaneous ablation for cT1 renal masses. Eur Urol 67:252–259
Rivero JR, De La Cerda J 3rd, Wang H, Liss MA, Farrell AM, Rodriguez R et al (2018) Partial nephrectomy versus thermal ablation for clinical stage T1 renal masses: systematic review and meta-analysis of more than 3,900 patients. J Vasc Interv Radiol 29:18–29
Sung HH, Park BK, Kim CK, Choi HY, Lee HM (2012) Comparison of percutaneous radiofrequency ablation and open partial nephrectomy for the treatment of size- and location-matched renal masses. Int J Hyperthermia 28:227–234
Collettini F, Schnapauff D, Poellinger A, Denecke T, Schott E, Berg T et al (2012) Hepatocellular carcinoma: computed-tomography-guided high-dose-rate brachytherapy (CT-HDRBT) ablation of large (5–7 cm) and very large (〉7 cm) tumours. Eur Radiol 22:1101–1109
Collettini F, Singh A, Schnapauff D, Powerski MJ, Denecke T, Wust P et al (2013) Computed-tomography-guided high-dose-rate brachytherapy (CT-HDRBT) ablation of metastases adjacent to the liver hilum. Eur J Radiol 82:e509–14
Vollherbst D, Bertheau R, Kauczor HU, Radeleff BA, Pereira PL, Sommer CM (2017) Treatment failure after image-guided percutaneous radiofrequency ablation (RFA) of renal tumors—a systematic review with description of type, frequency, risk factors and management. Rofo 189:219–227
Mohnike K, Wieners G, Schwartz F, Seidensticker M, Pech M, Ruehl R et al (2010) Computed tomography-guided high-dose-rate brachytherapy in hepatocellular carcinoma: safety, efficacy, and effect on survival. Int J Radiat Oncol Biol Phys 78:172–179
Ricke J, Mohnike K, Pech M, Seidensticker M, Ruhl R, Wieners G et al (2010) Local response and impact on survival after local ablation of liver metastases from colorectal carcinoma by computed tomography-guided high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 78:479–485
Mohnike K, Neumann K, Hass P, Seidensticker M, Seidensticker R, Pech M et al (2017) Radioablation of adrenal gland malignomas with interstitial high-dose-rate brachytherapy: Efficacy and outcome. Strahlenther Onkol 193:612–619
Wieners G, Pech M, Rudzinska M, Lehmkuhl L, Wlodarczyk W, Miersch A et al (2006) CT-guided interstitial brachytherapy in the local treatment of extrahepatic, extrapulmonary secondary malignancies. Eur Radiol 16:2586–2593
Geisel D, Collettini F, Denecke T, Grieser C, Florcken A, Wust P et al (2013) Treatment for liver metastasis from renal cell carcinoma with computed-tomography-guided high-dose-rate brachytherapy (CT-HDRBT): a case series. World J Urol 31:1525–1530
Mohnike K, Wolf S, Damm R, Seidensticker M, Seidensticker R, Fischbach F et al (2016) Radioablation of liver malignancies with interstitial high-dose-rate brachytherapy: Complications and risk factors. Strahlenther Onkol 192:288–296
Streitparth F, Pech M, Bohmig M, Ruehl R, Peters N, Wieners G et al (2006) In vivo assessment of the gastric mucosal tolerance dose after single fraction, small volume irradiation of liver malignancies by computed tomography-guided, high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 65:1479–1486
Wieners G, Mohnike K, Peters N, Bischoff J, Kleine-Tebbe A, Seidensticker R et al (2011) Treatment of hepatic metastases of breast cancer with CT-guided interstitial brachytherapy—a phase II-study. Radiother Oncol 100:314–319
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7:735–740
Raman JD, Jafri SM, Qi D (2016) Kidney function outcomes following thermal ablation of small renal masses. World J Nephrol 5:283–287
Mir MC, Ercole C, Takagi T, Zhang Z, Velet L, Remer EM et al (2015) Decline in renal function after partial nephrectomy: etiology and prevention. J Urol 193:1889–1898
Choi KH, Yoon YE, Kim KH, Han WK (2015) Contralateral kidney volume change as a consequence of ipsilateral parenchymal atrophy promotes overall renal function recovery after partial nephrectomy. Int Urol Nephrol 47:25–32
Takagi T, Mir MC, Sharma N, Remer EM, Li J, Demirjian S et al (2014) Compensatory hypertrophy after partial and radical nephrectomy in adults. J Urol 192:1612–1618
Stewart FA, Te Poele JA, Van der Wal AF, Oussoren YG, Van Kleef EM, Kuin A et al (2001) Radiation nephropathy—the link between functional damage and vascular mediated inflammatory and thrombotic changes. Acta Oncol 40:952–957
Atwell TD, Schmit GD, Boorjian SA, Mandrekar J, Kurup AN, Weisbrod AJ et al (2013) Percutaneous ablation of renal masses measuring 3.0 cm and smaller: comparative local control and complications after radiofrequency ablation and cryoablation. Ajr Am J Roentgenol 200:461–466
Caputo PA, Zargar H, Ramirez D, Andrade HS, Akca O, Gao T et al (2017) Cryoablation versus partial nephrectomy for clinical T1b renal tumors: a matched group comparative analysis. Eur Urol 71:111–117
Kunkle DA, Uzzo RG (2008) Cryoablation or radiofrequency ablation of the small renal mass: a meta-analysis. Cancer 113:2671–2680
Psutka SP, Feldman AS, McDougal WS, McGovern FJ, Mueller P, Gervais DA (2013) Long-term oncologic outcomes after radiofrequency ablation for T1 renal cell carcinoma. Eur Urol 63:486–492
Panje C, Andratschke N, Brunner TB, Niyazi M, Guckenberger M (2016) Stereotactic body radiotherapy for renal cell cancer and pancreatic cancer: literature review and practice recommendations of the DEGRO working group on stereotactic radiotherapy. Strahlenther Onkol 192:875–885
Pham D, Thompson A, Kron T, Foroudi F, Kolsky MS, Devereux T et al (2014) Stereotactic ablative body radiation therapy for primary kidney cancer: a 3-dimensional conformal technique associated with low rates of early toxicity. Int J Radiat Oncol Biol Phys 90:1061–1068
Siva S, Pham D, Kron T, Bressel M, Lam J, Tan TH et al (2017) Stereotactic ablative body radiotherapy for inoperable primary kidney cancer: a prospective clinical trial. BJU Int 120:623–630
Staehler M, Bader M, Schlenker B, Casuscelli J, Karl A, Roosen A et al (2015) Single fraction radiosurgery for the treatment of renal tumors. J Urol 193:771–775
Filippiadis DK, Gkizas C, Chrysofos M, Siatelis A, Velonakis G, Alexopoulou E et al (2018) Percutaneous microwave ablation of renal cell carcinoma using a high power microwave system: focus upon safety and efficacy. Int J Hyperthermia 34:1077–1081
Su MZ, Memon F, Lau HM, Brooks AJ, Patel MI, Woo HH et al (2016) Safety, efficacy and predictors of local recurrence after percutaneous radiofrequency ablation of biopsy-proven renal cell carcinoma. Int Urol Nephrol 48:1609–1616
Dai Y, Covarrubias D, Uppot R, Arellano RS (2017) Image-guided percutaneous radiofrequency ablation of central renal cell carcinoma: assessment of clinical efficacy and safety in 31 tumors. J Vasc Interv Radiol 28:1643–1650
Fukuda S, Seo Y, Shiomi H, Yamada Y, Ogata T, Morimoto M et al (2014) Dosimetry analyses comparing high-dose-rate brachytherapy, administered as monotherapy for localized prostate cancer, with stereotactic body radiation therapy simulated using CyberKnife. J Radiat Res 55:1114–1121
Pennington JD, Park SJ, Abgaryan N, Banerjee R, Lee PP, Loh C et al (2015) Dosimetric comparison of brachyablation and stereotactic ablative body radiotherapy in the treatment of liver metastasis. Brachytherapy 14:537–542
Siva S, Pham D, Gill S, Bressel M, Dang K, Devereux T et al (2013) An analysis of respiratory induced kidney motion on four-dimensional computed tomography and its implications for stereotactic kidney radiotherapy. Radiat Oncol 8:248
Dib RE, Touma NJ, Kapoor A (2009) Review of the efficacy and safety of radiofrequency ablation for the treatment of small renal masses. Can Urol Assoc J 3:143–149
Kapoor A, Touma NJ, Dib RE (2013) Review of the efficacy and safety of cryoablation for the treatment of small renal masses. Can Urol Assoc J 7:E38–44
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Damm, T. Streitparth, P. Hass, M. Seidensticker, C. Heinze, M. Powerski, J.J. Wendler, U.B. Liehr, K. Mohnike, M. Pech, and J. Ricke state that there are no competing interests and that this work has not received any funding.
Ethical standards
The study was conducted in accordance with the Declaration of Helsinki. All patients included were treated at a single institution, prospective data collection and analysis was approved by the local ethics committee. All patients gave written informed consent for the collection of their medical data for scientific purposes. No personal information is included in the publication, thus no dedicated approval was required.
Additional information
Availability of data and materials
All relevant data regarding the study conclusion are displayed in the publication. Raw data used and/or analyzed during the study are available from the corresponding author on reasonable request.
Rights and permissions
About this article
Cite this article
Damm, R., Streitparth, T., Hass, P. et al. Prospective evaluation of CT-guided HDR brachytherapy as a local ablative treatment for renal masses: a single-arm pilot trial. Strahlenther Onkol 195, 982–990 (2019). https://doi.org/10.1007/s00066-019-01501-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01501-1