Abstract
Purpose
To present radiological aspects of jejunoileal diverticulosis and its complications.
Results
Jejunoileal diverticulosis is a relatively rare and underestimated condition, which mostly affects the elderly. It is frequently asymptomatic but it can lead to significant complications requiring surgical treatment. Jejunoileal diverticulosis is far less common than colonic diverticulosis. Acquired small bowel diverticula are often numerous but the complication rate is low. Acute diverticulitis is the most frequent complication; its classic presentation involves the jejunum and is often non-severe. Diverticular hemorrhage is the second most common complication; CT scan examination is essential to determine the accurate topography of the pathological diverticula. Small bowel obstruction can occur through several mechanisms: adhesions, enterolith, and intussusception. Extra-intestinal gas without perforation and “pseudo-ischemic” appearance are non-pathological conditions that are important to diagnose in order to avoid surgery.
Conclusion
Jejunoileal diverticulosis usually does not show any symptoms but can lead to diagnostic challenges requiring evaluation by CT. CT scan signs of these complications and some pitfalls must be known.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Jejunoileal diverticulosis is not newly discovered, since the first report was published by Sir Astley Cooper in 1807. However it remains a rare and underestimated condition, involving mostly the elderly [1,2,3]. It is frequently asymptomatic but it can lead to life-threatening complications requiring surgical treatment [2,3,4]. The clinical diagnosis is difficult because the symptoms lack specificity [1], and in the past the diagnosis was performed intra-operatively only [1, 5]. Even surgical diagnosis could be challenging, due to the mesenteric location of the diverticula [6]. The technological advances and the increased availability of computed tomography (CT) have improved the diagnosis of small bowel diseases [7, 8]. Radiologists therefore play a major role in assessment of the acquired jejunoileal diverticular disease [9, 10]. The aim of this pictorial essay is to present the radiological features of jejunoileal diverticulosis, its complications, and its pitfalls.
Jejunoileal diverticulosis
Acquired diverticula of the jejunum and the ileum have a reported incidence of 0.3–2.3% [1, 5, 11]. These are far less frequent than duodenal diverticula (6–20%) [11] and colonic diverticula (ranging from 5% to 65% depending on the age) [12]. 80–90% of the patients involved are older than 40 [1, 11], without any gender predominance [5].
Jejunoileal diverticulosis is usually asymptomatic, but 15–20% of patients show minimal chronic symptoms [1, 4, 5, 13, 14], which may be related to pseudo obstruction or bacterial overgrowth (such as abdominal discomfort or pain, diarrhea, weight loss, and asthenia). Serious complications requiring surgery are rare (6–15%) [5].
Like in colonic diverticular disease, acquired small bowel diverticula are pseudodiverticula, which are herniations of the mucosa and the submucosa through the musculosa [2, 15, 16]. These are considered to be a type of pulsion diverticula, occurring in small weakened localized areas due to smooth muscle abnormalities, close to the penetrating mesenteric vascular branches [15,16,17]. This explains the topography of these diverticula, which usually occur at the mesenteric side of the small bowel wall (Fig. 1).
Jejunoileal diverticulosis in an 87-year-old male. The intraoperative view (a) and the CT scan coronal plane show multiple diverticula (stars) arising from the mesenteric edge of the bowel, close to the points of the vasa recta penetration (arrowheads). A thin diverticular wall is visible on this CT scan (b)
The physiopathology of the jejunoileal diverticulosis is unknown. Current hypotheses are focusing on abnormalities of the smooth muscle or myenteric plexus, on intestinal dyskinesis and on high intraluminal pressures [18].
Many rare diseases have been associated with small bowel diverticulosis (including Fabry’s disease, Cronkhite–Canada syndrome, and familial visceral myopathy) [19]. Some authors described familial cohorts of jejunoileal diverticulosis that could be consistent with a genetic predisposition [20].
Some authors mentioned the interest of MRI in the jejunoileal diverticulitis diagnosis [21], but the CT scan is the best type of imaging to detect complications such as pneumoperitoneum and acute bleeding. In most cases, imaging is performed under emergency conditions and contrast ingestion does not seem to be mandatory [9, 22, 23]. Conversely it could mask a bleeding point. Normal jejunoileal diverticula appear on a CT scan as round or ovoid outpouchings with a neck arising from the bowels, which can be better visualized on coronal or sagittal planes (Fig. 1) [7]. Their size is variable (ranging from a few millimeters to more than 5 cm), depending on the location (they tend to be smaller and fewer in the ileum) [5, 11, 16, 24, 25] and the intestinal repletion [21]. The diverticular wall is usually invisible without intestinal folds [1], but in some cases a thin wall may be visible (Fig. 1), probably due to asymptomatic minimal inflammatory episodes. Diverticula could be built up with a combination of fluid, gas, and feces [1]. Usually diverticula are numerous and diverticulosis is an extensive process over the small bowel [9].
Complications
The accurate prevalence of complications in jejunoileal diverticulosis is difficult to assess, ranging from 6 to 40% according to data from literature [5, 11, 24]. Its most frequent complication is diverticulitis, followed by hemorrhage and bowel obstruction [1]. Histological diagnosis of leiomyosarcoma has been reported in small bowel diverticula [26]. However, it was unclear whether these diverticula were acquired or Meckel’s diverticula.
Specific goals are required in the therapeutic strategy for elderly patients with multiple co-morbidities. For these patients, surgical indications should be cautiously analyzed and decided as a last resort in only the most severe cases.
Diverticulitis
Background
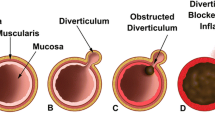
Diverticulitis is the most frequent complication of jejunoileal diverticulosis (2–6%) [11]. Infection could be explained by the stasis of the intestinal content inside the diverticulum and by the neck’s obstruction due to the mucosal edema [11, 16].
Most of the cases are mild [9], but perforations can also rarely occur (2–7% of the diverticulitis) because of a necrotizing inflammatory reaction or a progressive ulceration. The mortality is fairly high (ranging from 9 to 40%) [4, 9, 11, 27]. Poor prognostic factors are advanced age, associated co-morbidities, peritonitis, delayed diagnosis, and treatment [28, 29].
Symptoms are not specific such as acute abdominal pain (predominantly in the left flank in 39% of cases), abdominal guarding, and fever [9, 10]. Hyperleukocytosis and elevated levels of C-reactive protein are frequent [9, 10].
Acute uncomplicated diverticulitis is treated medically with success, while severe types with perforation require surgery [9]. The small bowel raises different therapeutic issues in comparison to the colon. One-stage resection and anastomosis of the small bowel is usually performed, without any need for stoma. Conservative treatment in cases of mesenteric abscesses could not be easy because of endoluminal bowel flow and difficult access via percutaneous procedures. Surgical treatment is not recommended to prevent recurrences, which are rare and rather seem to occur on different sites [9].
Imaging findings
The most reliable sign of uncomplicated diverticulitis is the direct visualization of the pathological diverticulum. It can be jejunal (87%), or less commonly ileal (13%) and present inflammatory changes (Fig. 2), such as a diverticular wall thickening and a mesenteric fat stranding [9, 21]. An association with a small bowel wall thickening is possible [9]. The other types of uncomplicated jejunal or ileal diverticula are most of the time visible and help in the diagnosis of the acquired type [9]. Diverticulitis of the terminal ileum is less common (Fig. 3), and is less frequently considered in diagnosis. It can be explained by the small size of the diverticula and challenging differential diagnoses at this site (cecal diverticulitis and acute appendicitis) [30].
Mild acute jejunal diverticulitis in an 87-year-old female. The coronal plane (a) shows a jejunal diverticulum (arrow), built up with gas and an enterolith, connected to the small bowel through a neck (star). Observe the fat stranding on the mesenteric edge (arrowheads) on the axial plane (b). A bowel wall thickening is also visible (a, b)
Marked mesenteric abnormalities (fluid and gas) are the most relevant features of perforation (Fig. 4). A diverticular wall defect could also be found in perforated diverticulitis (Fig. 5), but there is a low correlation of heterogeneous enhancement of the diverticular wall with the severity scale of the disease [9]. These findings could be explained by some pitfalls such as a spontaneous hyperdensity of the diverticular content, an asymmetrical diverticular inflammation or a fluid effusion close to the diverticulum [9]. The diagnosis can be challenging in severe types as marked local infiltration of fluid and gas makes the inflammatory diverticulum difficult to spot [9]. In such cases, the predominance of the peritoneal changes on the mesenteric edge of the small bowel as well as the presence of other jejunoileal diverticula on the CT scan suggest this diagnosis [9, 21].
Mesenteric or peritoneal abscesses can occur (Fig. 6) and should not be confused with normal diverticula. The non-surgical management of the mesenteric abscesses can be efficient, as the treatment depends on their size and on the clinical assessment [9]. Other complications such as portal vein thrombosis (Fig. 6), liver abscess, or fistula can be found.
Complicated ileal diverticulitis by abscess and portal venous thrombosis. The axial (a) and the coronal (c) planes show a loculated fluid collection (stars) close to a terminal ileum diverticulum. A portal venous thrombosis (arrowheads) is visible on the coronal (c) and another axial plane (b). The cecum (C), the appendix (A) and the terminal ileum (I) are marked
Other complications
Diverticular hemorrhage
Diverticular hemorrhage is the second most common complication of the jejunoileal diverticulosis (5–33%) [31, 32]. It can manifest as an acute or chronic bleeding [33]. Symptoms are rectal bleeding, hemorragic shock, or occasionally melena [6, 11, 31, 32]. Mechanisms are unknown and may be related to mesenteric vessels trauma from an enterolith, mucosal ulceration, or diverticulitis [31,32,33].
CT scan is the diagnostic imaging exam to perform in cases of acute bleeding because of the technical limitations of endoscopy in the small bowel [34]. Performing CT scan enables the exact location of the bleeding to be identified (Fig. 7), showing an extravasation of contrast material on arterial or portal phase from a diverticulum [31, 33]. The exact distance between the bleeding site and the angle of the Treitz or ileocecal valve is a crucial information to provide to the endoscopist or surgeon before the procedure [32, 34]. It can also aid surgical planning by percutaneous targeting of the pathologic diverticulum (Fig. 8) to allow a mini-laparotomy and a limited bowel resection.
Small bowel diverticular hemorrhage in an 89-year-old female. The axial plane (a) shows acute bleeding from within a small bowel diverticulum (arrowhead). The intraoperative image (b) does not show any external signs of abnormality of the pathological diverticulum (star). Another axial plane (c) shows a percutaneous targeting of this superficial diverticulum
Emergency surgery remains the gold standard treatment in case of massive acute bleeding, while conservative management can be performed in case of minimal bleeding [31, 32]. Yen et al. reported an overall mortality of 7.1% [32]. In cases without surgery, mortality is high, as is the risk of recurrences [4, 31, 32]. Reports showed that in some cases endoscopic management was efficient in stopping bleeding, particularly when new techniques are performed such as double-ballon endoscopy [34]. This strategy can be performed in hemodynamically stable patients with identified bleeding from the proximal jejunum or terminal ileum [31, 34]. Ultra-selective embolization can be performed if surgery is not possible in hemodynamically unstable patients [31, 34].
Bowel obstruction
Mechanical obstruction can occur through different mechanisms [4, 35,36,37,38]: enterolith ileus, diverticular adhesions (with or without volvulus), or compression by a large diverticulum. CT-scans are challenging to analyze (Fig. 9). Diverticular adhesive obstruction does not show any specific signs except diverticula on CT-scans [31, 37], but the transition zone can be unclear, therefore confusing the limit between the dilated bowel loops and the distended diverticula.
Adhesive small bowel obstruction in a 33-year-old female complicating jejunoileal diverticulosis. The coronal planes (a, b) show dilated small bowel loops partially built up with a feces sign (arrows) upstream of a transition zone in the right iliac fossa (arrowhead), next to a jejunal diverticulum (point). Some small bowel diverticula (stars) are challenging to distinguish from dilated bowel loops. The intraoperative image (c) confirms the diagnosis of adhesive small bowel obstruction (arrows) and the presence of multiple jejunoileal diverticula (stars)
Enterolith ileus is one of the most specific mechanisms related to jejunoileal diverticulosis (Fig. 10). Enteroliths in jejunoileal diverticulosis are actual primary enteroliths, which build up within the gastrointestinal tract as a result of the precipitation of substances from the food chyme [39,40,41]. Concretions formed inside diverticula are choleic acid enteroliths, either de novo or around bezoar stones. Bacterial overgrowth resulting from small bowel dyskinesia can trigger a deconjugation of bile salts, which then precipitate into a stone leading to the formation of an enterolith [39,40,41]. The migration of an enterolith out of a diverticulum can lead to bowel obstruction [39,40,41]. Enterolith may exhibit a slight homogeneous hyperdensity or be similar to a bezoard on CT-scans [36, 41]. Surgery is often necessary, but enterotomy is not the only procedure. Manual fragmentation of the enterolith can be efficient enough.
Enterolith ileus in an 85-year-old male. The coronal plane (a) shows dilated small bowel loops (arrow) and diverticula (arrowheads) upstream of an endoluminal obstacle (star). The intraoperative image (b) confirms the diagnosis of small bowel obstruction. An enterotomy (c) confirms a endoluminal obstacle due to an enterolith (star)
Pitfalls
Extradigestive gas without perforation
Extra-intestinal gas has been reported in patients with asymptomatic jejunoileal diverticulosis (Fig. 11). Physiopathology remains unclear. The distended diverticular mucosa could function as a semipermeable membrane which could enable the transmural equilibration of gas [42]. Other authors explained the presence of the gas due to a microperforation in the diverticular wall [14, 25]. Histological findings close to pneumatosis cystoides intestinalis have been reported, such as subserosal cyst or gas dissection (Fig. 11) [14, 25, 31].
Extradigestive gas in a jejunoileal diverticulosis without perforation in a 79-year-old male. The initial axial plane (a) shows small gas bubbles (arrowheads) surrounding small bowel diverticula. The other initial axial plane (b) shows gas bubbles within the diverticular wall (arrow), which are associated with subserosal cysts. The diverticular wall is merely slightly thickened and the mesentery does not show any signs of fat stranding or of fluid effusion. A CT scan which was performed 3 months later for another indication (c) showed a regression of these abnormalities
On the CT scan, the most specific sign is the presence of thin gas bubbles all around the diverticula, and no inflammatory changes (Fig. 11). Gas bubbles could be rarely seen at a distance also in the pre-hepatic area.
An accurate clinical assessment is fundamental in order to prevent unnecessary surgery in these cases. Most of the time patients are asymptomatic or show non-severe symptoms (such as vague abdominal pain or discomfort) but without any abdominal guarding [25].
Pseudo-ischemic presentation
The diverticulum wall is virtual and usually invisible. In comparison to small bowel loops which are normally enhanced, uncomplicated diverticula can simulate a lack of enhancement of the small bowel wall. It can also contain enteroliths that can simulate a feces sign. The radiological diagnosis can be particularly challenging to perform when mesenteric ischemia (Fig. 12) or bowel obstruction are clinically suspected.
Uncomplicated jejunoileal diverticulosis simulating acute mesenteric ischemia in a 73-year-old female with a post-cholecystectomy hematoma. The axial plane (a) shows unenhanced bowel loops (arrows) and peritoneal fluid effusion. The coronal plane (b) shows that the unenhanced bowel loops correspond to multiple jejunal diverticula (stars) with a virtual wall. The initial diagnosis was acute mesenteric ischemia. The intraoperative image (c) does not show any signs of ischaemia of the small bowel (arrowheads) or of the diverticula (stars)
Conclusion
Jejunoileal diverticulosis can lead to diagnostic challenges requiring evaluation by CT. CT scan signs of these complications and some pitfalls must be known. With an accurate CT scan assessment it is possible to choose a conservative treatment in cases of diverticular disease of the small bowel. Radiologists must be aware that jejunoileal diverticulosis can simulate many types of emergencies.
References
Fintelmann F, Levine MS, Rubesin SE (2008) Jejunal diverticulosis: findings on CT in 28 patients. AJR Am J Roentgenol 190(5):1286–90.
Maglinte DD, Chernish SM, DeWeese R, Kelvin FM, Brunelle RL (1986) Acquired jejunoileal diverticular disease: subject review. Radiology 158(3):577–80.
Baskin Jr RH, Mayo CW (1952) Jejunal diverticulosis: a clinical study of 87 cases. Surg Clin North Am 1185.
Longo WE, Vernava III AM (1992) Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum 35(4):381–8.
Liu C-Y, Chang W-H, Lin S-C, Chu C-H, Wang T-E, Shih S-C (2005) Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol 11(35):5557.
Lempinen M, Salmela K, Kemppainen E (2004) Jejunal diverticulosis: a potentially dangerous entity. Scand J Gastroenterol 39(9):905–9.
Lacalamita MC, Moschetta M, Mancini ME, Scardapane A, Angelelli G (2014) Role of CT in the diagnosis of jejunal-ileal perforations. Radiol Med (Torino) 119(9):651–7.
Ghekiere O, Lesnik A, Millet I, Hoa D, Guillon F, Taourel P (2007) Direct visualization of perforation sites in patients with a non-traumatic free pneumoperitoneum: added diagnostic value of thin transverse slices and coronal and sagittal reformations for multi-detector CT. Eur Radiol 17(9):2302–9.
Lebert P, Millet I, Ernst O, Boulay-Coletta I, Corno L, Taourel P, Zins M (2018) Acute Jejunoileal Diverticulitis: Multicenter Descriptive Study of 33 Patients. AJR Am J Roentgenol 210(6):1245–51.
Horesh N, Klang E, Gravetz A, et al. (2016) Jejunal diverticulitis. J Laparoendosc Adv Surg Tech A 26(8):596–599
Transue DL, Hanna TN, Shekhani H, Rohatgi S, Khosa F, Johnson J-O (2017) Small bowel diverticulitis: an imaging review of an uncommon entity. Emerg Radiol 24(2):195–205.
Ambrosetti P (2016) Acute left-sided colonic diverticulitis: clinical expressions, therapeutic insights, and role of computed tomography. Clin Exp Gastroenterol 9:249–57.
Kouraklis G, Glinavou A, Mantas D, Kouskos E, Karatzas G (2002) Clinical implications of small bowel diverticula. Isr Med Assoc J IMAJ 4(6):431–3.
Hanna C, Mullinax J, Friedman MS, Sanchez J (2016) Jejunal diverticulosis found in a patient with long-standing pneumoperitoneum and pseudo-obstruction on imaging: a case report. Gastroenterol Rep 4(4):337–40.
Edwards HC (1936) Diverticulosis of the small intestine. Ann Surg 103(2):230–54.
Coulier B, Maldague P, Bourgeois A, Broze B (2007) Diverticulitis of the small bowel: CT diagnosis. Abdom Imaging 32(2):228–33.
Kassir R, Boueil-Bourlier A, Baccot S, Abboud K, Dubois J, Petcu CA, Boutet C, Chevalier U, Montveneur M, Cano M-I, Ferreira R, Debs T, Tiffet O (2015) Jejuno-ileal diverticulitis: Etiopathogenicity, diagnosis and management. Int J Surg Case Rep 10:151–3.
Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD (1983) Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology 85(3):538–47.
Meagher AP, Porter AJ, Rowland R, Ma G, Hoffmann DC (1993) Jejunal diverticulosis. Aust N Z J Surg 63(5):360–6.
Barton JS, Karmur AB, Preston JF, Sheppard BC (2014) Familial jejuno-ileal diverticulitis: A case report and review of the literature. Int J Surg Case Rep 5(12):1038–40.
Mansoori B, Delaney CP, Willis JE, Paspulati RM, Ros PR, Schmid-Tannwald C, Herrmann K (2016) Magnetic resonance enterography/enteroclysis in acquired small bowel diverticulitis and small bowel diverticulosis. Eur Radiol 26(9):2881–91.
Stoker J, van Randen A, Laméris W, Boermeester MA (2009). Imaging patients with acute abdominal pain. Radiology 253(1):31–46.
Huynh LN, Coughlin BF, Wolfe J, Blank F, Lee SY, Smithline HA (2004) Patient encounter time intervals in the evaluation of emergency department patients requiring abdominopelvic CT: oral contrast versus no contrast. Emerg Radiol 10(6):310–3.
Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM (1997) Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg 184(4):383–8.
Kwak JY, Park EH, Park CS, Kim JH, Han MS, Kwak JH (2016) Uncomplicated jejunal diverticulosis with pneumoperitoneum. Ann Surg Treat Res 90(6):346–9.
Fiori E, Ansali A, Galati G, Graziano P, Drudi FM, Maccioni F, Cangemi V (1996) Leiomyosarcoma in jejunal diverticulum. A case report and review of the literature. Il G Chir 17(5):269–75.
Spasojevic M, Naesgaard JM, Ignjatovic D (2012) Perforated midgut diverticulitis: revisited. World J Gastroenterol WJG 18(34):4714.
Englund R, Jensen M (1986) Acquired diverticulosis of the small intestine: case reports and literature review. Aust N Z J Surg 56(1):51–4.
Eckhauser FE, Zelenock GB, Freier DT (1979) Acute complications of jejuno-ileal pseudodiverticulosis: surgical implications and management. Am J Surg 138(2):320–3.
Park H-C, Lee BH (2009) The management of terminal ileum diverticulitis. Am Surg 75(12):1199–202.
Makris K, Tsiotos GG, Stafyla V, Sakorafas GH (2009) Small intestinal nonmeckelian diverticulosis. J Clin Gastroenterol 43(3):201–7.
Yen HH, Chen YY, Yang CW, Soon MS (2012) Diagnosis and management of jejunoileal diverticular hemorrhage: a decade of experience. J Dig Dis 13(6):316–20.
Harbi H, Kardoun N, Fendri S, Dammak N, Toumi N, Guirat A, Mzali R (2017) Jejunal diverticulitis. Review and treatment algorithm. Presse Med.
Iwamuro M, Hanada M, Kominami Y, Higashi R, Mizuno M, Yamamoto K (2011) Endoscopic hemostasis for hemorrhage from an ileal diverticulum. World J Gastrointest Endosc 16;3(7):154–6.
Garnet DJ, Scalcione LR, Barkan A, Katz DS (2011) Enterolith ileus: liberated large jejunal diverticulum enterolith causing small bowel obstruction in the setting of jejunal diverticulitis. Br J Radiol 84(1004):e154–7.
Fourneau H, Coulier B, Afshin Rezazadeh A (2018) Small Bowel Obstruction Due to Enterolith in a Patient with Diffuse Jejuno-Ileal Diverticulosis. J Belg Soc Radiol 102(1):10.
Ghrissi R, Harbi H, Elghali MA, Belhajkhlifa MH, Letaief MR (2016) Jejunal diverticulosis: a rare case of intestinal obstruction. J Surg Case Rep 2016(2).
Mohi RS, Moudgil A, Bhatia SK, Seth K, Kaur T (2016) Complicated Jejunal Diverticulosis: Small Bowel Volvulus with Obstruction. Iran J Med Sci 41(6):548–51.
Gurvits GE, Lan G (2014) Enterolithiasis. World J Gastroenterol 21;20(47):17819–29.
Bewes PC, Haslewood GA, Roxburgh RA (1966) Bile-acid enteroliths and jejunal diverticulosis. Br J Surg 53(8):709–11.
Chugay P, Choi J, Dong XD (2010) Jejunal diverticular disease complicated by enteroliths: Report of two different presentations. World J Gastrointest Surg 27;2(1):26–9.
Dunn V, Nelson JA (1979) Jejunal diverticulosis and chronic pneumoperitoneum. Gastrointest Radiol 15;4(2):165–8.
Acknowledgements
We thank Dr. Paul Borde, Dr. Antonin Lereuil, Dr. Chritophe Leroy and Dr. Arturo Ze Roberto for their assistance with this study.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lebert, P., Ernst, O. & Zins, M. Acquired diverticular disease of the jejunum and ileum: imaging features and pitfalls. Abdom Radiol 44, 1734–1743 (2019). https://doi.org/10.1007/s00261-019-01928-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-01928-1