Abstract
Purpose
To compare dual-energy computed tomography (DECT) aortography using a 70% reduced iodine dose to single-energy CT (SECT) aortography using a standard iodine dose in the same patient.
Methods
Twenty-one patients with a prior SECT aortography using standard iodine dose had DECT aortography using 70% reduced iodine dose. Section 120 kVp images were compared to DECT images reconstructed at both 50 and 77 keV. Reviewers measured image noise and attenuation in the aorta at eight locations from proximal to distal and subjectively scored vascular enhancement on a four-point scale. Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were calculated. The volume CT dose index (CTDIvol) for each exam was recorded.
Results
Mean iodine dose was 50 g for SECT and 15 g for DECT (70% reduction). Mean aortic attenuation was similar for section 120 kVp (350 ± 67 HU) and DECT 50 keV (338 ± 57 HU, p = 0.547) but was lower at 77 keV (152 ± 23 HU). Measured image noise was greatest at 50 keV (12 ± 5 HU) and was lowest at 77 keV (7 ± 2 HU, p > 0.001). There was no difference in SNR or CNR between 120 kVp and 50 keV (p > 0.05). Mean subjective vascular enhancement scores for SECT were between good and excellent (3.33–3.69), and for DECT at 50 keV were between moderate and good (2.54–2.93, p < 0.0001). CTDIvol was 13.6 mGy for SECT and 13.1 mGy for DECT (p = 0.637).
Conclusion
70% Reduced iodine DECT aortography may result in similar aortic attenuation, CNR, SNR, and lower although acceptable subjective image scores when compared to standard iodine SECT aortography in the same patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Patients with aortic pathology who need contrast-enhanced computed tomography (CT) often have pre-existing renal insufficiency with an associated increased risk for contrast-induced nephropathy (CIN) [1, 2]. The size of this CIN risk may be related to the size of the iodine dose, so a mechanism for lowering iodine dose which does not compromise aortic attenuation would be desirable [3–5]. Dual-energy CT (DECT) allows synthetic image reconstruction at monochromatic energy levels closer to the k-edge of iodine (33.2 keV) where iodine exhibits much higher attenuation compared to single-energy CT (SECT) at 120 kVp. This higher attenuation of iodine with DECT may result in acceptable CT aortography using less IV contrast than typically used with SECT which may be beneficial for patients at risk for CIN. The purpose of this prospective study was to evaluate image quality and feasibility of a DECT aortography protocol using 70% reduced iodine dose compared to SECT aortography in the same patient.
Methods
This HIPAA-compliant prospective study was approved by our Institutional Review Board.
Study population
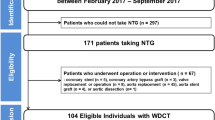
Patients were included if their age was over 18 and if they had a previous SECT aortogram at our institution performed with our standard clinical iodine dose and injection protocol. Patients were excluded if they were pregnant or if they had a known severe allergy to iodinated contrast, significant renal function compromise (creatinine clearance of less than 40 mL/min/1.73 m2), or a body mass index (BMI) above 35 kg/m2. We approached 48 patients over a 2-year period, who had a CT aortogram ordered for evaluation of aneurysm or for stent graft follow-up. Sixteen of the patients approached declined to participate, 32 agreed and signed written informed consent. For nine of these patients, DECT with reduced iodine dose was not performed as a research protocol exam because the anticipated radiation dose could not be matched to that of SECT (patient too large). Two of the DECT aortograms were technically inadequate (missed timing, contrast not injected) and were excluded. The study group thus consisted of 21 patients, 15 men and 6 women, with a mean age of 64 ± 8 years. Fifteen of these aortograms were performed for evaluation of aneurysm and six for stent graft follow-up. All 21 patients in the study group had a prior clinical SECT aortogram performed with a standard dose of iodine (Fig. 1).
CT exam
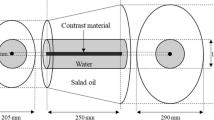
All DECT aortograms were performed on a 64-channel multi detector CT scanner with rapid-switch dual-energy technology (Discovery CT750 HD; GE Healthcare, Waukesha, WI). Initially, with the patient on the scanner, a SECT exam was simulated at the console by inputting our clinical aortography CT scan parameters: tube voltage of 120 kVp, and tube current based on body size. With this parameter information, the scanner displayed the estimated radiation dose of a simulated SECT exam. The technologist then used that dose information to select from several preset DECT protocol options, matching the estimated radiation dose of the DECT as closely as possible to the estimated radiation dose of the SECT. Additional scan parameters for both SECT and DECT exams are outlined in Table 1. Note that clinical SECT images were reconstructed using 40% ASIR, and DECT images were reconstructed using 70% ASIR. Study aortograms included the chest in 10 patients, the chest plus the abdomen and pelvis in 10 patients, and the abdomen and pelvis in 1 patient. For each DECT exam, gemstone spectral imaging software was utilized to create two series of virtual monochromatic images from the arterial phase: at 50 keV and at 77 keV using 2.5 mm slice thickness at 2.5 mm intervals in the axial plane (GSI Viewer; GE Healthcare, Waukesha, WI). These two series were sent to a post-processing workstation (GE Advantage Workstation 4.6) where they were de-identified and forwarded to a research folder on a picture archiving and communication system (PACS; Centricity, GE Healthcare, Chicago, IL). Prior section 120 kVp aortograms were also de-identified, and the arterial phase of the exam was sent to the same folder in PACS.
Contrast protocol
For SECT exams, our standard clinical contrast injection protocol employed iohexol 350 mg I/mL (Omnipaque 350; GE Healthcare, Princeton, NJ) with injection rates and volumes adjusted by weight (six categories between 55 and 105 kg) as well as by the Z-axis coverage length of the protocol. Rates of injection for prior SECT aortograms varied between 4 and 5 mL/s, while total volume of contrast varied between 100 and 150 mL. Contrast injection was followed by a 50 mL saline chaser injected at the same rate with a dual-head power injector (Medrad, Stellant D, Warrendale, PA). Injection start time was peak enhancement plus 4 s from a prior test bolus of 20 mL of contrast followed by 20 mL of saline injected at the same rate as the diagnostic study.
For the initial 10 patients in this series, we calculated the volume of iodixanol 270 mg I/mL (Visipaque 270; GE Healthcare, Princeton, NJ) that would result in a 70% iodine dose reduction from the prior SECT aortogram. That volume was injected at a rate which would result in the same injection duration for the DECT aortogram as had occurred during the prior SECT. For the remaining 11 patients, we utilized Omnipaque 350 at a volume that would achieve a 70% iodine dose reduction. That contrast volume was blended with saline in the dual-head power injector, so the total volume of saline plus contrast equaled the total volume of contrast in the prior SECT aortogram, injected at the same rate. The blended injection was followed immediately by a 50 mL saline flush. Injection start time for both DECT injection protocols was peak enhancement plus 4 s from a prior test bolus of 20 mL of contrast followed by 20 mL of saline injected at the same rate as the diagnostic study.
Image evaluation
The 42 exams (21 DECT and 21 SECT priors) were randomized using a random number generator and were presented to two reviewers working independently and at separate times on PACS workstations. For the DECT exams, each reviewer looked at the two DECT series at the same time. SECT exams were viewed separately from the DECT exams. Both reviewers were board-certified radiologists with fellowship training in body imaging, one with 5 years and the other with 32 years of experience. Both reviewers received standardized training on CT aortograms from three patients not included in this series.
Attenuation measurements (HU) were obtained by the senior reviewer in the psoas and at up to eight standardized locations along the aorta from proximal to distal depending on the degree of Z-axis coverage. A circular region of interest (ROI) was used to measure the central two-thirds of the vessel lumen on a magnified image at each location while avoiding plaque and artifact. This reviewer also measured and averaged image noise in adjacent air three times using an ROI of at least 4 cm2 placed away from blankets or artifacts. Aortic attenuation values at each location were recorded as being above or below a previously reported minimal acceptable intravascular density threshold for CT aortography (200 HU) [6]. Signal-to-noise (SNR) and contrast-to-noise (CNR) ratios were calculated using the following formulas: SNR = ROIaorta/Noiseair, CNR = (ROIaorta − ROIpsoas muscle/Noiseair). The volume CT dose index (CTDIvol) for the arterial phase was recorded.
Reviewers each subjectively scored aortic enhancement, brachiocephalic vascular enhancement, and abdominal aortic side-branch enhancement (celiac, superior mesenteric artery, and renal arteries) separately on the same four-point scale: (1) poor, barely perceptible, variable enhancement, non-diagnostic, (2) moderate, suboptimal enhancement, (3) good, typical clinical enhancement, (4) excellent, dense and uniform enhancement. Reviewers also subjectively scored overall image noise as: (1) major, impedes confidence in diagnosis, non-diagnostic, (2) moderate, diagnosis possible, (3) minor, typical clinical scan, (4) excellent, minimal noise.
Statistical analysis
Analysis was performed using statistical software SAS 9.4 (SAS Institute, Inc., Cary, NC). Attenuation and noise was compared across energies using one-way analysis of variance with Tukey post hoc pairwise comparisons. Continuous measures were summarized using means and standard deviations. Categorical data were summarized using counts and percentages. A p value <0.05 was considered statistically significant.
Results
The average time between the SECT prior exam and the DECT study exam was 11 months (range 4–22 months). Body weight did not change significantly between the two exams: BMI 28.26 kg/m2 for SECT and 28.15 kg/m2 for DECT (p = 0.57). The average iodine dose for SECT was 50 ± 4 g and for DECT was 15 ± 1 g, a 70% reduction. Injection rate of contrast ranged from 4 to 5 mL/s for the prior SECT exams (mean 4.6 mL/s) and from 1.5 to 5 mL/s for the DECT study exams. There was no significant difference in estimated radiation exposure; mean CTDIvol was 13.6 ± 4 mGy for the SECT exams and 13.1 ± 2 mGy for DECT exams (p = 0.637).
Mean attenuation of the aorta, CNR, and SNR for the SECT standard iodine 120 kVp exams was statistically similar to DECT reduced iodine exams reconstructed at 50 keV (Table 2; Figs. 2, 3, 4). Image noise between the three energy levels was statistically different, highest at 50 keV, and lowest at 77 keV (p < 0.001). When mean attenuation of the aorta at each ROI was compared to a threshold of 200 HU, 98% of measurements were above that threshold for section 120 kVp, 99% of HU were above for 50 keV, and 5% were above for 77 keV (Table 3).
Sixty-six-year-old woman with a history of ascending aortic aneurysm a 2.5 mm DECT performed with 13 g of iodine reconstructed at 50 keV (W/L 960/171, ascending aorta attenuation 576 HU, noise 8 HU), b the same DECT examination reconstructed at 77 keV (W/L 436/93, ascending aorta attenuation 217 HU, noise 5 HU), and c a prior SECT on the same patient performed with 44 g of iodine at 120 kVp (W/L 736/66, ascending aorta attenuation 466, noise 7 HU)
Sixty-nine-year-old man with a history of ascending aortic aneurysm a 2.5 mm DECT performed with 13 g of iodine reconstructed at 50 keV (W/L 509/74, attenuation of the aorta at the level of the renal arteries 352 HU, noise 8 HU), b the same DECT examination reconstructed at 77 keV (W/L 378/54, attenuation of the aorta at the level of the renal arteries 146 HU, noise 5 HU), and c a prior SECT on the same patient performed with 44 g of iodine at 120 kVp (W/L 720/197, attenuation of the aorta at the level of the renal arteries 396 HU, noise 7 HU)
Graph displaying the mean attenuation of the aorta in eight proximal to distal locations for reduced iodine DECT reconstructed at 50 and 77 keV and for standard iodine SECT reconstructed at 120 kVp. ROI 1 at the level of the right pulmonary artery in the ascending aorta, ROI 2 at the mid-aortic arch, ROI 3 at the level of the right inferior pulmonary vein in the descending aorta, ROI 4 at the level of the diaphragmatic hiatus, ROI 5 at the level of the renal arteries, ROI 6 above the bifurcation of the aorta, ROI 7 at the level of the right mid-common iliac artery, and ROI 8 at the level of the left mid-common iliac artery
Mean subjective enhancement scores for both reviewers are presented in Table 4. Subjective enhancement scores of the aorta and side branches were lower for DECT at 50 keV (mean between moderate and good) than for SECT at 120 kVp (mean between good and excellent). Mean overall image noise scores were statistically lower (higher noise) for DECT at both 50 and 77 keV than for SECT at 120 kVp with a mean noise score between minor and moderate (p < 0.0001).
Discussion
CT aortography may require a relatively large volume of iodinated contrast to achieve adequate vascular enhancement over a long Z-axis scan. DECT aortography is a promising tool for reducing iodine dose in patients with renal insufficiency. A prior study reported using DECT to reduce iodine dose by 50% in CT aortography achieving 60% higher attenuation of the aorta at 50 keV compared to standard iodine SECT at 120 kVp [7]. This result suggests the possibility of even further iodine dose reduction with DECT aortography.
In the current investigation, we hypothesized that a DECT aortography protocol performed with a 70% iodine dose reduction reconstructed at 50 and 77 keV would result in an acceptable exam for both intravascular attenuation and image noise when compared to full iodine dose SECT at 120 kVp in the same patient. We found that a DECT reduced iodine protocol at 50 keV resulted in acceptable vascular assessment with a mean aortic attenuation of 338 HU, similar to the aortic attenuation of SECT at 120 kVp with a standard iodine dose. Further, for both DECT and SECT aortograms, attenuation of the aorta was uniform from proximal to distal. Noise was lowest at 77 keV and highest at 50 keV, while CNR and SNR at 50 keV were similar to section 120 kVp. Although mean subjective enhancement scores were best at 120 kVp, they scored between moderate and good at 50 keV. Mean subjective image noise was best at 120 kVp but was between moderate and minor for 77 keV. This suggests it is important to view both 55 and 77 keV images together when using DECT to decrease iodine dose.
Several features of this investigation should be mentioned. First, we chose to evaluate only two synthetic monochromatic energy levels: 50 keV because it has been reported to have optimal CNR ratio in abdominal tissues and 77 keV because it results in an image tissue contrast appearance similar to that of polychromatic 120 kVp SECT [8–10]. We believed that this combination of synthetic monochromatic energy levels could provide good intravascular attenuation plus good images for non-vascular structures. Second, for DECT we arbitrarily chose a relatively high ASIR blend percentage (70%) in order to reduce the higher intrinsic noise in images displayed at lower energy levels. We did not attempt to evaluate the impact of this higher ASIR blend percentage as a separate variable, although some authors have described a waxy or blotchy appearance at higher ASIR levels. Third, we chose to match the radiation dose between the two protocols in order to reduce the number of variables in this study.
While other authors have investigated the use of DECT to decrease iodine dose [11–14], only a few studies have prospectively compared to SECT in the same patient [7, 15]. Agrawal et al. performed DECT using a 30–40% iodine dose reduction on patients who had previously undergone SECT aortography. They found up to a 185% increase in attenuation and up to 25% higher CNR with monochromatic energy levels reconstructed at 40–70 keV and concluded that further iodine dose reduction would be possible. Shuman et al. performed DECT aortography with a 50% iodine dose reduction and compared results to prior SECT exams performed in the same patient using standard iodine dose. They found that DECT images reconstructed at 50 keV resulted in 60% greater aortic attenuation than SECT with comparable SNR and CNR. They also speculated that further iodine dose reduction might be possible. Based on these reports, we arbitrarily chose to investigate a 70% reduction of iodine for DECT aortography.
This study has several important limitations. First, we limited this investigation to analysis of intravascular attenuation, image noise measurements, and subjective scoring, comparing SECT and DECT when imaging parameters were selected to match radiation dose. We did not attempt to assess diagnostic accuracy or to assess the impact of different patient radiation dose levels. Second, we analyzed results from only two synthetic monochromatic energy levels for in order to keep clinical workflow efficient. The impact of adding other energy levels to such an analysis is unknown. Third, we looked at only one level of iodine dose reduction with DECT. Other contrast dosing schema may produce different results. Fourth, we limited this investigation to patients with BMI under 35 kg/m2 because of the known impact of larger body size on DECT image quality. Fifth, we used 40% ASIR for SECT and 70% ASIR for DECT. Finally, our choice for 70% reduction in iodine dose was based on our prior work. Our method of achieving a 70% reduction of iodine dose changed midway through this series. The first method used a lower iodine concentration contrast (270 mg I/mL) coupled with a lower volume and injection rate compared to the prior SECT aortogram. This approach resulted in a few cases with some non-uniform enhancement from proximal to distal, likely because of the low volume and injection rate. The second method used a higher iodine concentration contrast (350 mg I/mL) blended with saline in a dual-head power injector, so that both the total injected volume and the injection rate for DECT were the same as for prior SECT. We observed that this second method of contrast injection to achieve iodine dose reduction resulted in a more consistent uniform aortic enhancement from proximal to distal.
Conclusion
DECT aortography using 70% reduced iodine dose and reconstructed at 50 and 77 keV may result in similar aortic attenuation, CNR, and SNR, and lower but acceptable subjective image scores compared to standard iodine SECT aortography in the same patient. This technique may be useful in patients with renal insufficiency who are at risk for CIN.
References
Hagiwara S, Saima S, Negishi K, et al. (2007) High incidence of renal failure in patients with aortic aneurysms. Nephrol Dial Transplant 22:1361–1368
Parmer SS, Fairman RM, Karmacharya J, et al. (2006) A comparison of renal function between open and endovascular aneurysm repair in patients with baseline chronic renal insufficiency. J Vasc Surg 44:706–711
Chang CF, Lin CC (2013) Current concepts of contrast-induced nephropathy: a brief review. J Chin Med Assoc 76:673–681
Laville M, Juillard L (2010) Contrast-induced acute kidney injury: How should at-risk patients be identified and managed? J Nephrol 23:387–398
Nyman U, Almen T, Aspelin P, et al. (2005) Contrast-medium-induced nephropathy correlated to the ratio between dose in gram iodine and estimated GFR in ml/min. Acta Radiol 46:830–842
Schoellnast H, Tillich M, Deutschmann MJ, et al. (2004) Aortoiliac enhancement during computed tomography angiography with reduced contrast material dose and saline solution flush: influence on magnitude and uniformity of the contrast column. Investig Radiol 39:20–26
Shuman WP, Chan KT, Busey JM, Mitsumori LM, Koprowicz KM (2016) Dual-energy CT aortography with 50% reduced iodine dose versus single-energy CT aortography with standard iodine dose. Acad Radiol 23:611–618
Kulkarni NM, Sahani DV, Desai GS, Kalva SP (2012) Indirect computed tomography venography of the lower extremities using single-source dual-energy computed tomography: advantage of low-kiloelectron volt monochromatic images. J Vasc Interv Radiol 23:879–886
Beeres M, Trommer J, Frellesen C, et al. (2016) Evaluation of different keV-settings in dual-energy CT angiography of the aorta using advanced image-based virtual monoenergetic imaging. Int J Cardiovasc Imaging 32:137–144
Pinho DF, Kulkarni NM, Krishnaraj A, Kalva SP, Sahani DV (2013) Initial experience with single-source dual-energy CT abdominal angiography and comparison with single-energy CT angiography: image quality, enhancement, diagnosis and radiation dose. Eur Radiol 23:351–359
Carrascosa P, Capunay C, Rodriguez-Granillo GA, et al. (2014) Substantial iodine volume load reduction in CT angiography with dual-energy imaging: insights from a pilot randomized study. Int J Cardiovasc Imaging 30:1613–1620
He J, Wang Q, Ma X, Sun Z (2015) Dual-energy CT angiography of abdomen with routine concentration contrast agent in comparison with conventional single-energy CT with high concentration contrast agent. Eur J Radiol 84:221–227
Yuan R, Shuman WP, Earls JP, et al. (2012) Reduced iodine load at CT pulmonary angiography with dual-energy monochromatic imaging: comparison with standard CT pulmonary angiography—a prospective randomized trial. Radiology 262:290–297
Godoy MC, Heller SL, Naidich DP, et al. (2009) Dual-energy MDCT: comparison of pulmonary artery enhancement on dedicated CT pulmonary angiography, routine and low contrast volume studies. Eur J Radiol 79:e11–e17
Agrawal MD, Oliveira GR, Kalva SP, Pinho DF, Arellano RS, et al. (2016) Prospective comparison of reduced-iodine-dose virtual monochromatic imaging dataset from dual-energy CT angiography with standard-iodine-dose single-energy CT angiography for abdominal aortic aneurysm. Am J Roentgenol 207:W125–W132
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by GE Healthcare.
Conflict of interest
William P. Shuman received research grants from GE Healthcare. The other authors declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shuman, W.P., O’Malley, R.B., Busey, J.M. et al. Prospective comparison of dual-energy CT aortography using 70% reduced iodine dose versus single-energy CT aortography using standard iodine dose in the same patient. Abdom Radiol 42, 759–765 (2017). https://doi.org/10.1007/s00261-016-1041-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-1041-z