Abstract
Pseudomyxoma peritonei (PMP) is a rare disease with neoplastic growth of mucin-secreting cells in the peritoneal cavity, resulting in mucinous ascites. The septum of intra-abdominal fluid collection is a key imaging finding characteristic to PMP. In magnetic resonance imaging (MRI), multi-b value diffusion-weighted imaging (DWI) is a method used to obtain an accurate apparent diffusion coefficient. The clinical utilities of DWI using lower b values as diagnostic imaging are rarely highlighted. This report describes a case of PMP in which DWI using b values of 100 and 500 s/mm2 exclusively visualized many thick septa with low signal intensity in peritoneal effusion. The septa could not be recognized in DWIs with b values of zero or 1000 s/mm2, as with ultrasonography, computed tomography, and conventional MRI. A discrepancy between DWI using lower b values and other MRI sequences or imaging modalities indicates a specific capability of DWI using low b values: the ability to visualize septa of intra-abdominal fluid collection much thicker than in real cases. Results for this case suggest that DWI using low b values might present clinical potential for the preoperative diagnosis of PMP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pseudomyxoma peritonei (PMP) is a rare disease, with incidence of one or two per million per year [1]. PMP clinically presents a characteristic pattern of tumor growth, with growth of neoplastic mucin-secreting cells in the peritoneal cavity resulting in gelatinous mucinous ascites [2]. Because PMP symptoms tend to be non-specific, it is difficult to diagnose it preoperatively. Imaging findings of PMP can also be non-specific, overlapping the findings of peritoneal carcinomatosis or peritonitis. The septum of intra-abdominal fluid collection on ultrasonography (US) or computed tomography (CT) is a key imaging finding that helps to produce a correct diagnosis [3–5].
For magnetic resonance imaging (MRI), diffusion-weighted images (DWI) using multiple b values have come to be used to obtain accurate apparent diffusion coefficient (ADC) values that are insensitive to perfusion effects [6]. This method with multiple b values provides DWI of respective b values. In clinical situations, however, we use only DWI with the highest b values (e.g., 1000 s/mm2). The clinical utilities of DWI with lower b values as diagnostic imaging have not been elucidated.
We present an impressive case of PMP with a novel imaging finding: lower b values exclusively visualized the septa of ascites, which CT or conventional MRI could not do. Based on this case, we discuss the clinical utility of DWI with lower b values.
Case report
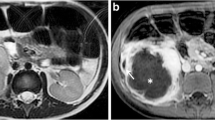
Because of massive ascites pointed out by a medical check-up, a woman in her 50s was referred to the Department of Gynecology of our institution on suspicion of ovarian or peritoneal cancer. The patient’s laboratory data revealed elevated concentrations of tumor markers: CEA 11.4 ng/ml (normal range 5.0 ng/ml), CA19-9 339.2 U/ml (normal range 37.0 U/ml), CA 125 236.2 U/ml (normal range 35.0 U/ml). Massive viscous ascites with echogenicity was observed from transvaginal ultrasonography (TVUS). On contrast-enhanced CT, diffuse peritoneal thickening and a fluid-filled distended appendix with the thickened wall were additionally observed (Fig. 1A). No septa were recognized from either TVUS or CT. Pelvic MRI examination was performed with a 1.5 T scanner (Avanto; Siemens Healthcare, Erlangen, Germany). No apparent ovarian lesion was found. Conventional sequences including T2-weighted (Fig. 1B)/T1-weighted images and contrast-enhanced T1-weighted images were unable to visualize septa. DWI with b values of 0 and 1000 s/mm2 and ADC map provided no additional findings (Fig. 2A, D, E). However, DWI with b values of 100 and 500 s/mm2 clearly visualized thick septa with low signal intensity in massive ascites with high signal intensity, which strongly suggested the diagnosis of PMP (Fig. 2B, C).
No septum of fluid collection was observable on contrast-enhanced CT (A), fast spin-echo T2-weighted images (B), or contrast-enhanced T1-weighted images (C). Massive fluid collection and the distended appendix were observed (A white circle), and pseudomyxoma peritonei was clinically suspected. No compression of abdominal structures was observed
Diffusion-weighted images (DWI) using multiple b values and apparent diffusion coefficient (ADC) map. A–D DWI with the b values of zero (A), 100 (B), 500 (C), and 1000 s/mm2 (D). E ADC map. DWI with the b values of 100 and 500 s/mm2 exclusively visualized thick septa with low intensity signal (B, C arrows)
Abdominocentesis was performed. The cytodiagnosis of ascites revealed mucinous adenocarcinoma. Based on the results of cytodiagnosis and findings of appendix, PMP/mucinous carcinoma peritonei was clinically suspected, rather than ovarian tumors/peritoneal cancer. She was transferred to the Department of Surgery. Surgical resection was performed. Massive ascites (3900 ml) were aspirated, and operative findings after the aspiration revealed diffuse peritoneal invasion: surface of liver and spleen, greater and lesser omentum, and Douglas pouch. Appendiceal tumor with clinical serosal invasion was found, which was regarded as an origin of PMP. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy with 100 mg of cisplatin and 4 mg of mitomycin C were performed.
Pathological examination revealed mucinous adenocarcinoma, high-grade, of appendix with diffuse peritoneal invasion. Final diagnosis was PMP/mucinous carcinoma peritonei, high-grade, arising from mucinous adenocarcinoma of appendix.
Discussion
We experienced an impressive PMP case suggesting the diagnostic utility of DWI using lower b values, which exclusively visualized septa of intra-abdominal fluid collection. DWI using lower b values might help to make a correct diagnosis of PMP preoperatively.
The septa visualized by DWI using lower b values should be the septa of mucinous ascites, representing walls of mucinous lesions or fibrous tissue between lesions, known as a key imaging finding of PMP, along with the compression of other abdominal structures such as the liver [7]. Although the possibility that there were no septa in the ascites is undeniable, it may be less likely because the septa were depicted at the same position on DWI with b values of 100 and 500. The presence of septa was not recognized in the operative examination because the septa had already been ruptured by the aspiration of ascites, thus becoming unrecognizable. The septa could not be observed on CT or conventional MRI. The reason for the lack of visibility of septa in these images might be that the septa were too thin. Regarding TVUS, the small field of view and the echogenicity of ascites might impair the ability of visualization. Detailed assessment for ascites by US might have visualized the septa.
The clinical utility of DWI using an intermediate b value (400–500 s/mm2) was reported by Low et al. in the detection of peritoneal tumors when added to conventional MRI [8]. They also mentioned the superiority of DWI with intermediate b values in the anatomical localization and signal-to-noise ratio, in comparison with DWI with high b values. In our case, DWI with b values of 100 and 500 exclusively visualized clear thick septa with low signal intensity, which might add a new clinical value of DWI with lower b values. If the septa had been sufficiently simple as visualized on DWI with lower b values, the septa could have been visualized easily using CT and other MR sequences including T2-weighted and contrast-enhanced T1-weighted images. The discrepancy between DWIs using lower b values and other methods indicates the ability of DWI using lower b values to show septa of intra-abdominal fluid collection much thicker than in reality.
Based on this case, we suggest the clinical potential of DWI using low b values in the visualization of septa of fluid collection in the peritoneal cavity. The mechanism of this phenomenon remains unknown yet. One hypothesis is that this phenomenon is a kind of motion artifact along the septa, induced by MRI scanner table vibration. Reportedly, the table vibration caused by motion probing gradient of DWI increased ADC values of the gelatinous phantom [9]. Because of the secondary increase of ADC values along the septa of mucinous ascites, DWI might visualize thick septa with a very low signal intensity. The mechanism of this phenomenon should be examined further using phantom studies with and without isolation from the MRI scanner table.
In conclusion, DWI using multiple b values has sufficient clinical potential to visualize the septa of PMP in the peritoneal cavity.
References
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA (2008) Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol 34(2):196–201. doi:10.1016/j.ejso.2007.04.002
Bosman FC, Hruban RH, Neil D (2009) Tumors of the appendix. In: Fred T (ed) WHO classification of tumors of the digestive system, 4th edn. Lyon: International Agency for Research on Cancer, pp 122–125
Li Y, Guo A, Tang J, et al. (2013) Role of preoperative sonography in the diagnosis and pathologic staging of pseudomyxoma peritonei. J Ultrasound Med 32(9):1565–1570. doi:10.7863/ultra.32.9.1565
Sulkin TV, O’Neill H, Amin AI, Moran B (2002) CT in pseudomyxoma peritonei: a review of 17 cases. Clin Radiol 57(7):608–613
Diop AD, Fontarensky M, Montoriol PF, Da Ines D (2014) CT imaging of peritoneal carcinomatosis and its mimics. Diagn Interv Imaging 95(9):861–872. doi:10.1016/j.diii.2014.02.009
Padhani AR, Liu G, Koh DM, et al. (2009) Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia 11(2):102–125
Tirumani SH, Fraser-Hill M, Auer R, et al. (2013) Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging 13:14–25. doi:10.1102/1470-7330.2013.0003
Low RN, Sebrechts CP, Barone RM, Muller W (2009) Diffusion-weighted MRI of peritoneal tumors: comparison with conventional MRI and surgical and histopathologic findings—a feasibility study. Am J Roentgenol 193(2):461–470
Ogura A, Maeda F, Miyai A, Hayashi K, Hongoh T (2006) Effect of vibration caused by time-varying magnetic fields on diffusion-weighted MRI. Nihon Hoshasen Gijutsu Gakkai zasshi 62(4):565–569
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there are no conflicts of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived in this case report.
Rights and permissions
About this article
Cite this article
Himoto, Y., Kido, A., Fujimoto, K. et al. A case of pseudomyxoma peritonei: visualization of septa using diffusion-weighted images with low b values. Abdom Radiol 41, 1713–1717 (2016). https://doi.org/10.1007/s00261-016-0697-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0697-8