Abstract
Background
Acute appendicitis, especially if perforated at presentation, is often complicated by postoperative abscess formation. The detection of a postoperative abscess relies primarily on imaging. This has traditionally been done with contrast-enhanced computed tomography. Non-contrast magnetic resonance imaging (MRI) has the potential to accurately detect intra-abdominal abscesses, especially with the use of diffusion-weighted imaging (DWI).
Objective
To evaluate our single-center experience with a rapid non-contrast MRI protocol evaluating post-appendectomy abscesses in children with persistent postsurgical symptoms.
Materials and methods
In this retrospective, institutional review board-approved study, all patients underwent a clinically indicated non-contrast 1.5- or 3-Tesla abdomen/pelvis MRI consisting of single-shot fast spin echo, inversion recovery and DWI sequences. All MRI studies were reviewed by two blinded pediatric radiologists to identify the presence of a drainable fluid collection. Each fluid collection was further characterized as accessible or not accessible for percutaneous or transrectal drainage. Imaging findings were compared to clinical outcome.
Results
Seven of the 15 patients had a clinically significant fluid collection, and 5 of these patients were treated with percutaneous drain placement or exploratory laparotomy. The other patients had a phlegmon or a clinically insignificant fluid collection and were discharged home within 48 h.
Conclusion
Rapid non-contrast MRI utilizing fluid-sensitive and DWI sequences can be used to identify drainable fluid collections in post-appendectomy patients. This protocol can be used to triage patients between conservative management vs. abscess drainage without oral/intravenous contrast or exposure to ionizing radiation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis is the most common acute surgical condition in children [1]. Large population studies in the United States and Canada have shown that approximately one-quarter of children with appendicitis present with perforation [2]. Postoperative intra-abdominal abscess is the most common complication of perforated appendicitis with an incidence of 3% to 25% in most recent large series [3,4,5]. An intra-abdominal abscess has been shown to double the duration of the hospital stay and cost of perforated appendicitis [4]. Imaging plays a crucial role in detecting intra-abdominal abscess in post-appendectomy patients. This has traditionally been performed with contrast-enhanced computed tomography (CT) with intraluminal bowel contrast to help differentiate between fluid-filled bowel loops and inter-loop abscesses. Ultrasound is also useful, though this modality can be challenging due to ileus and abdominal tenderness in the acute abdomen, limiting the evaluation of deep and inter-loop abscesses. Though the imaging algorithms for diagnosis of pediatric appendicitis are evolving with the incorporation of magnetic resonance imaging (MRI), the use of MRI for postoperative evaluation of this patient population remains in its infancy. A few publications have discussed the use of MRI with diffusion-weighted imaging (DWI) for evaluating intra-abdominal abscesses in children and adults [6, 7].
The purpose of our study was to evaluate and report our single institutional experience with a rapid non-contrast MRI protocol for evaluating post-appendectomy patients with clinical concern for abscess.
Materials and methods
This is a retrospective, institutional review board-approved and HIPAA (Health Information Portability and Accountability Act) compliant study.
All patients underwent a clinically indicated non-contrast MRI abdomen and pelvis exam on a 1.5- or 3-Tesla scanner. Our MRI protocol is shown in Table 1. These studies were performed during a 10-month period, October 2015 to August 2016. The field of view extended from the diaphragm to the bladder base. All MRI studies were reviewed by one of three radiologists, 2 with certificates of added qualification (CAQ) in pediatric radiology (11 and 2 years’ post fellowship) and 1 CAQ eligible (1 year post fellowship). For this retrospective review, consensus reads were performed by two pediatric radiologists (E.P.E. and E.F.S.) blinded to all patient information. The DWI sequences and apparent diffusion coefficient (ADC) map were reviewed to identify foci of diffusion restriction (subjective assessment of hypointensity compared to skeletal muscle as well as ADC value measurement). If the foci of diffusion restriction showed fluid signal on the T2-weighted images, they were considered to represent infected fluid collections, and if there was no corresponding fluid signal they were considered to represent a phlegmon (Figs. 1 and 2). Each collection was measured in the longest dimension in the axial plane x orthogonal maximum diameter in the axial plane x maximum craniocaudad dimension. Using the formula for an ellipse, the volume of each collection was estimated as the product of the 3 diameters × 0.52. The fluid collections were considered clinically significant if the smallest dimension was at least 2 cm. Each drainable fluid collection was further characterized as accessible or not accessible for percutaneous (no overlying bowel loops) or transrectal drainage (location in the cul-de-sac). A radiology resident (M.H.L.) reviewed all patient charts to review the clinical characteristics of the patient population, indications for MRI, outcome after MRI and clinical follow-up.
Cul-de-sac fluid collection in a 6-year-old boy (case 9) 10 days post appendectomy with persistent leukocytosis. Axial diffusion-weighted image b-value 800 mm/s2 (a) and axial apparent diffusion coefficient map (b) show a focus of diffusion restriction in the cul-de-sac (arrows) that corresponds to fluid signal on the T2-weighted axial (c) and coronal (d) images (arrows) compatible with a cul-de-sac abscess. The boy underwent transrectal drainage of the abscess. The drainage catheter was removed after 4 days, and he was discharged home on intravenous antibiotics
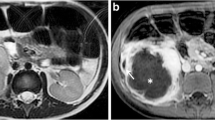
Phlegmon in the right lower quadrant in a 7-year-old girl with a history of perforated appendicitis 5 days post appendectomy with persistent leukocytosis (case 8). Axial diffusion-weighted image b-value 800 mm/s2 (a) and axial apparent diffusion coefficient map (b) show a focus of diffusion restriction (arrows) in the right lower quadrant with no corresponding fluid signal on the T2-weighted axial (c) image (arrow) compatible with a phlegmon. The patient was discharged home 2 days later on oral antibiotics
Results
Patient characteristics
There were 15 patients in the study cohort (8 girls and 7 boys). Patient characteristics are summarized in Table 2. The age range of the cohort was 6–17 years (median: 12.6 years). Fourteen of the patients had perforated appendicitis, while one had surgically proven non-perforated appendicitis. Initial intervention for appendicitis was as follows: laparoscopic appendectomy in 12 patients, laparotomy in 1, conservative management with antibiotics in 1 and percutaneous abscess drainage in 1. The median time interval between initial intervention to MRI was 8 days (range: 5–31 days). Indications for imaging to evaluate for possible abscess were as follows: persistent leukocytosis (10 patients), follow-up abscess after prior drainage (4 patients), persistent fever (3 patients) and persistent abdominal pain (3 patients). In addition, Some patients had multiple indications for imaging.
Imaging findings
All patients successfully completed the MRI scan without sedation. Ten patients underwent scanning on 1.5-T scanners and 5 on 3-T scanners. The average duration of the MRI scan as determined from the time of the localizer sequence to the time of the last sequence was 18 min (range: 11–31 min). The ideal scan time for each of the sequences is shown in Table 1. The total ideal scan time including the localizers (0:21 min) is 3 min and 46 s.
The MRI findings and patient management/clinical outcome are summarized in Table 2. In our series, all abscesses and phlegmons had an ADC value of <1 × 10−3 mm2/s. Thirteen of the 15 patients were found to have foci of diffusion restriction on MRI, while 2/15 had postsurgical inflammatory stranding without foci of diffusion restriction. These 2 patients were discharged home in <48 h. Of the 13 who had areas of diffusion restriction, 3 had no corresponding fluid signal on the T2-weighted sequences and were deemed as having phlegmons. All 3 were discharged home in <48 h. Ten of the 13 had corresponding T2 fluid signal and were classified as having an infected fluid collection, volume 0.5–395 cm3 (median: 13 cm3, mean: 57 cm3). Using a size criterion of a minimum diameter of 2 cm, 7/10 were considered to have a clinically significant fluid collection, while in the other 3, the fluid collection was considered to be too small to be clinically significant. Those 3 were discharged home in 24 h or less. Five of the seven clinically significant fluid collections were considered to be accessible for drainage by interventional radiology based on the location of the collection (all in the cul-de-sac) while two were determined to be non-accessible (one located in the mesenteric root and one located medial to the descending colon with overlying bowel). Transrectal drainage of the diffusion-restricting cul-de-sac collections was performed in four of five patients, while one was managed medically with intravenous antibiotics at the discretion of the treating surgeon. Of the two patients with non-accessible collections, one underwent exploratory laparotomy with drainage of a large abscess, volume 395 cm3, (Fig. 3) and was discharged from the hospital 10 days later, while the other was managed with intravenous antibiotics and discharged home the next day as there were multiple overlying bowel loops and the collection had a maximum diameter of 2.5 cm (volume 8 cm3).
Deep mesenteric abscess in a 10-year-old boy with a history of perforated appendicitis and persistent fever and abdominal pain. Axial diffusion-weighted image b-value 800 mm/s2 (a) and axial apparent diffusion coefficient map (b) show a large area of diffusion restriction in the mesenteric root (arrows), which corresponds to fluid signal on the T2-weighted axial (c) and coronal (d) images (arrows) compatible with a deep inter-loop abscess. The patient underwent exploratory laparotomy as the abscess was not amenable to image-guided drainage
Clinical course
The duration of abscess drainage in the four patients who had drains placed by interventional radiology was 2–7 days (median: 3.5 days). Cultures of the fluid collections were positive in four of the five patients who had percutaneous or surgical drainage. One culture had abundant polymorphonuclear leukocytes but no organisms. Fourteen of 15 patients presented to surgery clinic for a routine follow-up appointment while one followed up with endocrinology due to coexisting diabetes. The time interval for all patients from discharge to clinic follow-up visit was 6–40 days (median: 20 days). None of the patients had any residual symptoms or signs related to their appendicitis, and all were discharged from further care by pediatric surgery after their outpatient follow-up.
Discussion
Acute appendicitis is one of the most frequent indications for surgery in children. Although appendicitis was previously treated with laparotomy, laparoscopic appendectomy has now become the standard of care [1]. Both open appendectomy and laparoscopic appendectomy have associated complications, which include intra-abdominal abscesses, wound infection and bowel obstruction [1]. The rate of complications after appendectomy has been reported at approximately 13%, with the rate of intra-abdominal abscess at 7.5% [8]. In patients with perforated appendicitis, the rate of postoperative abscess is higher, around 14.8% [9]. Various clinical factors have been found to be associated with postoperative intra-abdominal abscess. These include white blood cell count >16,500/ml, C-reactive protein >3.1 mg/dl, presence of bowel obstruction or persistent peritonitis [9,10,11].
The diagnosis of post-appendectomy intra-abdominal abscess relies heavily on imaging. Sonography can be challenging due to overlying surgical dressings, abdominal pain/peritonitis and ileus that can limit visualization of inter-loop abscesses. Many centers utilize CT, often with intravenous and oral contrast, for evaluating an intra-abdominal abscess. Oral contrast can be very useful in this setting for differentiating inter-loop fluid collections from adjacent bowel loops. However, patients with complicated appendicitis and recent abdominal surgery have limited tolerance for oral contrast, and ileus can significantly prolong transit times, requiring a long prep time for CT with intraluminal contrast. Also, contrast-enhanced CT has limited diagnostic accuracy in differentiating a non-infected fluid collection from an abscess. If a fluid collection is identified on contrast-enhanced CT, the child typically undergoes image-guided intervention and may require additional follow-up imaging studies. This often requires multiple scans that result in repeated exposure to ionizing radiation.
We have been performing a rapid MRI protocol with DWI in this patient population for the last 2 years with good clinical success. This protocol has the advantage of not requiring intravenous or oral contrast or exposing the child to ionizing radiation. The free-breathing technique is particularly helpful in the postoperative period as sick children may not be able to cooperate with breath-holding instructions. Furthermore, the limited protocol with a short scan time is favorable in children. Although the average scan time in our study was 18 min due to variability in patient size and cooperation, the ideal scan time according to our protocol is 3 min 46 s. Since these studies are typically requested on an urgent basis, the short scan time also makes it feasible to accommodate these studies in the midst of a busy MRI schedule. In our single-center experience, this has been an accurate, efficient and safe way to evaluate abscess in post-appendectomy patients. Limitations of this rapid MRI protocol include the inability to detect retained appendicoliths and the potential need for sedation in children younger than 7 years. Also, indwelling drains in patients who have already undergone prior drainage are more difficult to see by MRI as compared to a CT.
DWI has become standard of care in pediatric abdominal MRI, especially in evaluating inflammatory bowel disease and solid tumors [12, 13]. Though the role of DWI in detecting intracranial abscesses is well established, there is limited literature on its use for detecting intra-abdominal abscesses in children [6, 7]. Oto et al. [7] have shown that non-infected ascites have a higher ADC value than abscesses in adults, and they suggested a threshold value of 2.0 × 10−3 mm2/s for differentiating non-infected fluid from abscess. However, other studies have shown the mean ADC value of an abdominal abscess to be 0.8 × 10−3 mm2/s [6]. In our series, all abscesses and phlegmons had an ADC value of <1 × 10−3 mm2/s. Correlation with fluid-sensitive sequences was needed to differentiate infected fluid collections that would require intervention from phlegmons that would not require drainage.
Limitations of our study include its retrospective design, the relatively small number of patients and some variation in patient management based on the subjective assessment of the treating physician. Although the sample size in this study is small, the results suggest that the MRI findings may help guide clinical management. Four of the five patients with clinically significant and accessible fluid collections had a drain placed. One of the two patients with clinically significant but inaccessible fluid collections had surgical intervention. In contrast, the patients with phlegmon or clinically insignificant fluid collections were all discharged within 48 h. Although managing fluid collections is sometimes variable depending on the treating physician, accurate characterization of the collection may aid in standardizing treatment approaches. Given the small sample size of this study and low rate of postoperative intra-abdominal abscess formation, further prospective work encompassing a long duration and large sample size is needed to further validate these findings.
Conclusion
A rapid non-contrast MRI protocol can be used to triage pediatric post-appendectomy patients with clinical signs and symptoms concerning for intra-abdominal fluid collections/abscesses between drainage vs. conservative management. Our clinical experience shows that rapid non-contrast MRI is a valuable alternative to conventional contrast-enhanced CT for detecting drainable fluid collections in post-appendectomy patients.
References
Gasior AC, St Peter SD, Knott EM et al (2012) National trends in approach and outcomes with appendicitis in children. J Pediatr Surg 47:2264–2267
Cheong LH, Emil S (2014) Outcomes of pediatric appendicitis: an international comparison of the United States and Canada. JAMA Surg 149:50–55
Emil S, Laberge JM, Mikhail P et al (2003) Appendicitis in children: a ten-year update of therapeutic recommendations. J Pediatr Surg 38:236–242
Fike FB, Mortellaro VE, Juang D et al (2011) The impact of postoperative abscess formation in perforated appendicitis. J Surg Res 170:24–26
Fishman SJ, Pelosi L, Klavon SL et al (2000) Perforated appendicitis: prospective outcome analysis for 150 children. J Pediatr Surg 35:923–926
Neubauer H, Platzer I, Mueller VR et al (2012) Diffusion-weighted MRI of abscess formations in children and young adults. World J Pediatr 8:229–234
Oto A, Schmid-Tannwald C, Agrawal G et al (2011) Diffusion-weighted MR imaging of abdominopelvic abscesses. Emerg Radiol 18:515–524
Ikeda H, Ishimaru Y, Takayasu H et al (2004) Laparoscopic versus open appendectomy in children with uncomplicated and complicated appendicitis. J Pediatr Surg 39:1680–1685
Emil S, Elkady S, Shbat L et al (2014) Determinants of postoperative abscess occurrence and percutaneous drainage in children with perforated appendicitis. Pediatr Surg Int 30:1265–1271
Fraser JD, Aguayo P, Sharp SW et al (2010) Physiologic predictors of postoperative abscess in children with perforated appendicitis: subset analysis from a prospective randomized trial. Surgery 147:729–732
Obayashi J, Ohyama K, Manabe S et al (2015) Are there reliable indicators predicting post-operative complications in acute appendicitis? Pediatr Surg Int 31:1189–1193
Chavhan GB, Caro-Dominguez P (2016) Diffusion-weighted imaging in pediatric body magnetic resonance imaging. Pediatr Radiol 46:847–857
Ream JM, Dillman JR, Adler J et al (2013) MRI diffusion-weighted imaging (DWI) in pediatric small bowel Crohn disease: correlation with MRI findings of active bowel wall inflammation. Pediatr Radiol 43:1077–1085
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Lee, M.H., Eutsler, E.P., Sheybani, E.F. et al. Rapid non-contrast magnetic resonance imaging for post appendectomy intra-abdominal abscess in children. Pediatr Radiol 47, 935–941 (2017). https://doi.org/10.1007/s00247-017-3860-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3860-7