Abstract
Objectives
The present article provides an overview of the spectrum of abdominal findings of histiocytic disorders that may be observed in multimodality imaging illustrated by clinical cases from our Imaging Center.
Methods
We will review abdominal findings of Langerhans cell histiocytosis, Rosai–Dorfman disease, Erdheim–Chester disease, and hemophagocytic syndrome illustrated by clinical cases from our imaging department with histologic correlation.
Results
Abdominal involvement of histiocytic disorders is rare and may occur in the liver, biliary tract, kidney, retroperitoneum, kidney, gastrointestinal tract, and lymph nodes.
Conclusion
Histiocytic disorders encompass a group of rare diseases with a wide range of manifestations in which the abdominal involvement is quite infrequent. The role of the radiologist is to report the major imaging findings and the differential diagnosis; however, the imaging features are unspecific and biopsy usually is necessary to establish the definitive diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Histiocytosis is a complex and heterogeneous group of disorders of unknown etiology, more common among children and characterized by a proliferation of histiocytes. Differentiating each type of histiocytosis can be quite challenging and requires a combination of clinical, radiological, histological, and immunohistochemical features [1].
Histiocytes are a group of immune cells that include macrophages and dendritic cells. Although their origin is not completely understood, it is believed that these cells originate from the same bone marrow hematopoietic precursor. This progenitor cell develops monocytes that, after maturing in the bone marrow, are released in the peripheral blood and ultimately transferred to almost every organ as tissue macrophages. These cells are designated according to the tissue in which they are found, such as the Küpffer cells in the liver, the alveolar macrophages in the lung, and osteoclasts in the bone, and are responsible for the phagocytosis of elements that are strange to the organism. This same hematopoietic progenitor may originate dendritic cells, which have antigen-presenting functions, like the Langerhans cells and the interdigitating dendritic cells. Under specific circumstances, there is local induction toward the differentiation of these cells into the most suitable phenotype to meet the demands of the organism [1, 2].
Histiocytosis was first classified into three groups according to the type of histiocyte: (1) class I [Langerhans cell histiocytosis (LCH)]; (2) class II (histiocytosis of mononuclear phagocytes other than Langerhans cell); and (3) class III (malignant histiocytic disorders) [3].
As the knowledge on the biology of these disorders evolved, the necessity of a new classification that comprised those new information emerged. This novel classification was developed in 1997 by a joint of pathologists and pediatric hematologists/oncologists of the World Health Organization’s Committee on Histiocytic/Reticulum Cell Proliferations and the Reclassification Working Group of the Histiocyte Society [1], and is summarized in Table 1. Histiocytosis is a multisystemic disorder and may produce a broad range of imaging manifestations. The present article provides an overview of the spectrum of abdominal findings of histiocytic disorders that may be observed on multimodality imaging.
Langerhans cell histiocytosis
LCH is the most common type of histiocytosis and is characterized by a clonal proliferation of histiocytes with Langerhans cell phenotype [2].
Clinical aspects
LCH is nearly twice as common in males as in females and have the peak age of diagnosis between 1 and 3 years of age, yet the disease can develop at any age [4–6]. The disorder has a broad spectrum of systemic involvement, ranging from unicentric to multicentric disease [7–10].
The most common manifestations of the LCH are bone lesions, but extraosseous disease has been reported in many organs [11, 12]. Extraosseous manifestations of LCH are less frequent and more difficult to be diagnosed than osseous LCH. Furthermore, the extraosseous manifestations usually appear as multicentric disease and may demonstrate a more aggressive behavior [13, 14].
Pathologic findings
The pathogenesis of LCH remains poorly understood and controversial despite various epidemiological studies [4–9]. The most likely theory is based on primarily reactive and immunologically mediated process [15] but the controversy on it being a clonal vs. a reactive immunologic response is still unsettled [16].
The diagnosis depends on the recognition of abnormal Langerhans cell, which has indistinct cytoplasmic borders, oval nuclei, nuclear grooves, pale and abundant cytoplasm with fine granules arranged in sheets or clusters. These Langerhans cells are frequently admixed with inflammatory cells, like eosinophils, neutrophils, lymphocytes, and plasma cells. Multinucleated osteoclast-like giant cells may be found. Necrosis is common and the cells may exhibit frequent mitosis. Atypical mitosis is not found [2, 15]. At ultrastructural studies, Birbeck granules in the cytoplasm are typical, which appear to be related with endosomal traffic. At immunohistochemistry, Langerhans cells have a characteristic CD68, S100 protein, CD1a, and langerin positivity [2] (Figs. 1, 2).
Langerhans cell histiocytosis in an 18-year-old girl with abdominal pain and jaundice. A Axial contrast-enhanced T1WI GRE with fat saturation demonstrating hepatomegaly, infiltrative lesion in the left hepatic lobe (arrow), and focal mild intrahepatic biliary duct dilatation with wall thickening (arrowheads). B Histological examination of liver biopsy shows diffuse proliferation of histiocytes. C Immunochemistry positive for S100. D Immunochemistry positive for CD1a.
Langerhans cell histiocytosis in a 3-year-old boy who underwent liver transplant. A, B Axial pre- and postcontrast T1WI GRE with fat saturation demonstrating hepatosplenomegaly and solid tissue in the hepatic hillum and periportal space (arrowheads). C Histological examination of liver explant shows sheets of cells with dark nuclei and pale cytoplasm aroud bile ducts (asterix), a few scattered eosinophils and macrophages (black circle) are also present. D Immunochemistry positive for CD1a.
Abdominal imaging features
The most common manifestations of LCH are bone lesions. Extraosseous disease is less prevalent. Abdominal involvement corresponds to approximately 40% of overall extraosseous disease [11]. The main abdominal manifestations are hepatobiliary and gastrointestinal.
Hepatobiliary
The hepatobiliary involvement is observed usually in multicentric disease, but it is present in less than 20% of patients with LCH [17, 18].
The Langerhans cells infiltrate the periportal space of the liver and the bile ducts (Fig. 1). There are 4 histopathologic stages of hepatobiliary involvement: (1) proliferative; (2) granulomatous; (3) xanthomatous, and (4) fibrous. The main imaging findings in proliferative and granulomatous phases are periportal tissue with contrast enhancement on CT and MRI and periportal edema represented by periportal hyperintensity on T2-weighted MRI [19] (Fig. 2). Lipid-laden nodules in the liver appear on the xanthomatous phase. These nodules appear hyperechoic on US, hypoattenuating on CT, and hyperintense on unenhanced T1-weighted MRI without fat suppression [20, 21]. The final fibrous stage results in diffuse liver disease, biliary cirrhosis, and secondary portal hypertension.
The direct histiocytic infiltration of bile ducts results in secondary sclerosing cholangitis with consequent intra- and extrahepatic biliary irregularities and areas of focal narrowing and dilatation [22].
The main differential diagnosis is adverse effects of chemotherapy, lymphoma, leukemia, hepatitis, and cholangiopathies (infectious, ischemic, or mechanical) [12, 17].
Gastrointestinal
The involvement of the gastrointestinal tract is rare and may be primary or a part of a systemic disease [12, 23, 24]. It may affect any part of the gastrointestinal tract from the oral mucosa to the anal canal. The main clinical symptoms are abdominal pain, vomiting, diarrhea, malabsorption, intestinal obstruction, and bloody stools. Those symptoms may be preceded by or be associated with rash in most patients [25]. Considering that the gastrointestinal symptoms are nonspecific, its frequency is probably underestimated.
The histiocytic infiltration of the gastrointestinal wall may be continuous or discontinuous and results in mucosal erosion, wall thickening, mucosal atrophy, and glandular destruction.
The main imaging features in gastrointestinal LCH are loss of mucosal pattern, wall thickening, mucosal hyperenhancement, luminal narrowing with dilated segments, proliferation of mesenteric fat, mesenteric fat stranding, free fluid [12, 23–25], and rarely perforation [26].
The differential diagnosis includes inflammatory bowel disease, lymphoma, infection, and drug reaction [12, 23–25].
Rosai–Dorfman disease (sinus histiocytosis with massive lymphadenopathy)
Rosai–Dorfman disease (RDD) also known as sinus histiocytosis with massive lymphadenopathy is a rare benign disease and was established as a clinicopathologic entity by Rosai and Dorfman in 1969 [27]. It is much more frequent among children and young adults and the median age at diagnosis is 20 years. There is a slight predilection for males (58%), and for individuals of African descent [28].
Although the etiology remains unknown, the RDD is thought to be caused by an exaggerated response of the hematopoietic system to an immunological trigger probably caused by Epstein–Barr and herpesvirus 6 infections [29].
Clinical aspects
The most common initial presentation of RDD is massive painless cervical lymphadenopathy in children or young adults, but axillary, para-aortic, inguinal, and mediastinal lymph nodes may also be affected. Nonspecific systemic symptoms (fever, fatigue, and weight loss) are frequently observed [28, 29]. Immunological disorders (autoimmune hemolytic anemia, rheumatoid arthritis, glomerulonephritis, asthma, and diabetes mellitus) are common among these patients.
The RDD can also involve a large variety of extranodal sites [30]. The incidence of extranodal involvement of RDD in most recent series is approximately 40% [28, 30]. The most common extranodal involvement sites are bone, skin, soft tissue, central nervous system, eye, orbit, upper respiratory tract, including salivary glands. The most common abdominal organs involved are liver, pancreas, kidney, gastrointestinal tract, and retroperitoneum [30].
The clinical course of RDD is usually self-limited, with a tendency for total spontaneous regression [29]. However, involvement of the low respiratory tract, kidney, and liver is associated with worse prognosis, as well as the number of extranodal sites involved and the association of immunological disorders [30].
Pathologic findings
Lymph nodes involved by RDD have their normal architecture altered by dilatation of sinuses, leading to effacement of follicles and germinal centers, as well as capsular fibrosis and of pericapsular tissues. Lymph nodes sinuses are expanded by a mixed population of cells, composed mainly of histiocytes and plasma cells clustered around vessels (Fig. 3). Histiocytes have large vesiculous nuclei, prominent nucleoli, well-defined nuclear membranes, and abundant pale eosinophilic cytoplasm. Nuclear atypia, mitosis, and necrosis are rare. The most striking histological feature of RDD is emperipolesis, which is defined as the presence of intact lymphocytes inside intracytoplasmic vacuoles of histiocytes (Fig. 3). Plasma cells, neutrophils, and red blood cells may also be found inside these vacuoles [2, 31].
Rosai–Dorfman disease in a 17-year-old boy with renal nodules on previous ultrasound. A, B Contrast-enhanced CT shows one of cortical kidney nodules (arrow) and bilateral inguinal lymphadenopathy (arrowheads). C, D Histological examination of right inguinal lymph node biopsy demonstrating expansion of sinuses by a mixed cellular infiltrate composed mainly of histiocytes and intact lymphocytes inside intracytoplasmic vacuoles of histiocytes, characterizing emperipolesis (black arrows).
Extranodal RDD has similar morphologic features as nodal couterpart. However, extranodal RDD exhibits more fibrosis, less typical histiocytes, and less emperipolesis [2, 30–32].
At immunohistochemical studies, RDD histiocytes express S100 protein and pan-macrophage markers, like CD68 and CD14. They do not stain for CD1a nor for markers of dendritic differentiation, like CD21, CD23, and CD35 [2, 31].
Abdominal imaging features
Liver
The hepatic lesions usually occur in the form of multiple small hypovascular nodules on CT and MRI representing granuloma-like histiocytic infiltrates, which can be accompanied by clinically detectable hepatomegaly [33].
Pancreas
Primary pancreatic RDD is a very rare entity. Only three cases have been previously reported in the literature [34–36]. Extranodal RDD simulates malignancy because it presents as an infiltrative mass lesion and can be multifocal [34–36].
Kidneys
The renal involvement by RDD should be included in the differential diagnosis of renal hilar masses, subcapsular hypodense infiltration, or renal cortical hypodense nodules on CT (Fig. 3). Renal involvement has been associated with a poorer prognosis, when compared with the overall disease mortality of less than 2% [28, 37, 38].
Gastrointestinal tract
The gastrointestinal tract is the least commonly involved site by RDD, accounting for less than 1% of all extranodal cases [16, 39]. It was described a predilection for the distal portion of the gastrointestinal tract with involvement of the colon and rectum in a majority of cases [39]. The involvement of gastrointestinal tract results in wall thickening or wall masses.
Retroperitoneum
The most frequent retroperitoneal involvement includes infiltrative mass or lymph nodes surrounding the kidneys, ureters, and retroperitoneal vessels, which may distort vessels and also produce ureteric or renal pelvis obstruction [28].
The main differential diagnoses of RDD are infectious or granulomatous conditions, primary malignancy, lymphoma, and metastatic disease.
Erdheim–Chester disease
Erdheim–chester disease (ECD) is a rare xanthogranulomatous histiocytosis of non-Langerhans cells most common in male adults between the fourth and seventh decades of life. It was first described by Erdheim and Chester in 1930 [40] and is characterized by multifocal osteosclerotic lesions of the long bones.
Although there is a speculation that ECD and other histiocytic disorders may represent an aberrant response to infection, no infectious etiology has been identified. It remains controversial if ECD is a reactive polyclonal histiocyte proliferation or a monoclonal neoplastic process [41, 42].
Clinical aspects
ECD is a systemic disease with a wide spectrum of clinical manifestations. Bone tissue is the most frequently involved. Associated extraskeletal manifestations are observed in 50% of cases. The most common extraskeletal involvements are pituitary gland, skin, orbit, heart, lung, and retroperitoneum [43]. Spleen, lymph nodes, and liver are usually spared. However, a case of ECD with vertebral osteolytic lesions and involvement of liver has been reported [44].
The isolated bone involvement has a good prognosis while disseminated disease especially with involvement of heart or central nervous system has a worse prognosis [43].
Pathologic findings
ECD lesions are composed of an infiltrate of foamy histiocytes and Touton-type giant cells enmeshed in fibrous tissue and sclerotic bone (Fig. 4). Lymphocytes, plasma cells, and sparse eosinophils are also observed.
Erdheim–Chester Disease in a 42-year-old man with weight loss. A, B Axial contrast-enhanced CT and T2WI shows a retroperitoneal infiltrative lesion surrounding the abdominal aorta (arrowheads) and the kidneys (arrows), causing moderate dilatation of the left calyceal system. C, D Contrast-enhanced T1WI demonstrating suprasellar, pontine, and cerebellar lesions with intense enhancement (arrows). E Postcontrast T1WI shows an intense and diffuse enhancement of the tibiae (arrowheads). F, G Histological examination of the right tibia biopsy showing infiltrate composed mainly of foamy histiocytes (black arrows) and a few scattered plasma cells and lymphocytes among sclerotic bone.
At immunohistochemical studies, ECD foamy histiocytes express CD68, CD14, CD163, factos XIIIa, and fascin. They are negative for S100 protein, CD1a, and langerin. Ultrastructural studies reveal that ECD histiocytes contain intracytoplasmic lipid vacuoles. Birbeck granules are absent [2].
Abdominal imaging features
Kidneys
Infiltration of the perirenal fat appears as an irregular renal border producing a “hairy kidney” appearance on CT and MRI. On CT, this manifests as a hypodense and homogeneous band with spiculated contours and mild contrast enhancement. On MRI, it is isointense to muscle on T1- and T2-weighted sequences, with a slight and homogeneous enhancement after contrast injection. Perirenal infiltration may progress to the renal sinuses and produce a post renal obstruction (Fig. 4). The ureteral segments which are most commonly affected by fibrosis are the middle and distal segments. The renal arteries may also be involved by tissue infiltration and fibrosis [43].
Retroperitoneum
Retroperitoneal involvement with ECD can manifest as a mass-like infiltrative surrounding the abdominal aorta with the same characteristics of the perirenal lesions (Figs. 4, 5). This can lead to acute or slowly progressive renal insufficiency. Retroperitoneal involvement frequently includes a bilateral, symmetric, and diffuse thickening of the adrenal glands associated with infiltration of the adjacent fat [43].
Erdheim–Chester Disease in a 52-year-old woman with abdominal pain and fever. A Axial contrast-enhanced CT shows an infiltrative soft tissue lesion surrounding the abdominal aorta and the renal arteries (arrow). B Coronal contrast-enhanced CT demonstrating the longitudinal extension of the aorta encasement (arrows).
Others (rare)
There are few reports of involvement of the liver [44] and bile ducts [45]. Biliary hilar infiltration may produce Klatskin-like lesions.
The main differential diagnoses of RDD are retroperitoneal fibrosis, sclerosing mesenteritis, and retroperitoneal neoplasms, mainly lymphoma and germ cell tumor.
Hemophagocytic syndromes
Clinical aspects
Among all types of histiocytosis, hemophagocytic syndromes are the most important in terms of morbidity and mortality. They may be primary (genetical) or secondary (acquired). These syndromes are characterized by a disseminated and uncontrolled proliferation and activation of macrophages and T lymphocytes, with upregulation of inflammatory cytokines, mediated mainly by TNF-α, in response to varied stimuli. The excessive activation of inflammatory cytokines may lead to a potentially fatal systemic inflammatory syndrome, characterized by bone marrow depression, hepatosplenomegaly, alteration of liver function, and coagulation cascade disturbances [46, 47].
Primary forms are motivated by mutations of genes related to NK cells and T lymphocytes function, which prompt disturbances in these cells activities. However, many of the genes involved are yet to be detected and the pathogenesis of these conditions remains to be clarified [46]. On the other hand, secondary forms are triggered by a varied number of stimuli, like viral infections, especially EBV, lymphoproliferative diseases and other neoplasms, parenteral nutrition, multiple organic failure, and rheumatologic disorders.
Pathologic findings
Hemophagocytosis is a common finding in bone marrow biopsies and is not a sufficient criterion for the diagnosis of hemophagocytic syndrome. It is necessary to consider clinical aspects and laboratory data as well. Histiocyte Society has defined criteria for the diagnosis of hemophagocytic lymphohistiocytosis, which are summarized in Table 2.
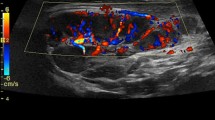
Abdominal imaging features
The main abdominal radiological findings are hepatosplenomegaly, increased periportal echogenicity at ultrasound, gallbladder wall thickening, nephromegaly with increased cortical echogenicity, lymphadenopathy and free fluid [48] (Fig. 6).
Hemophagocytic syndrome (HS) in a 1-year-old girl with fever, hepatosplenomegaly, and biochemical markers of HS. A Axial T2WI shows hepatomegaly, heterogeneous liver signal, splenomegaly, and ascites. B Axial contrast-enhanced T1WI GRE with fat saturated demonstrating diffuse transient hepatic parenchymal enhancement. Liver biopsy confirmed HS associated with veno-occlusive disease.
Veno-occlusive disease is a rare complication of hemophagocytic syndrome [49] (Fig. 6).
Conclusion
Histiocytic disorders encompass a group of rare diseases with a wide range of manifestations, in which the abdominal involvement is quite infrequent. The role of the radiologist is to report the major imaging findings and the differential diagnosis; however, the imaging features are unspecific and biopsy usually is necessary to establish the definitive diagnosis.
References
Favara BE, Feller AC, Pauli M, et al. (1997) Contemporary classification of histiocytic disorders. The WHO Committee On Histiocytic/Reticulum Cell Proliferations. Reclassification Working Group of the Histiocyte Society. Med Pediatr Oncol 29(3):157–166
Swerdlow SH, Campo E, Harris NL, et al. (2008) WHO classification of tumours of haematopoietic and lymphoid tissues, vol. 2, 4th edn. Lyon: IARC Press
Chu T, D'Angio GJ, Favara B, Ladisch S, et al. (1987) Histiocytosis syndromes in children. Writing Group of the Histiocyte Society. Lancet 1(8526):208–209
Broadbent V, Egeler RM, Nesbit ME Jr (1994) Langerhans cell histiocytosis–clinical and epidemiological aspects. Br J Cancer 23:S11–S16
Campos MK, Viana MB, de Oliveira BM, Ribeiro DD, Silva CM (2007) Langerhans cell histiocytosis: a 16-year experience. J Pediatr 83(1):79–86
Martin A, Macmillan S, Murphy D, Carachi R (2014) Langerhans cell histiocytosis: 23 years’ paediatric experience highlights severe long-term sequelae. Scott Med J 59(3):149–157
Alston RD, Tatevossian RG, McNally RJ, et al. (2007) Incidence and survival of childhood Langerhans cell histiocytosis in Northwest England from 1954 to 1998. Pediatr Blood Cancer 48(5):555–560
Arico M (2004) Langerhans cell histiocytosis in adults: more questions than answers? Eur J Cancer 40(10):1467–1473
Nicholson HS, Egeler RM, Nesbit ME (1998) The epidemiology of Langerhans cell histiocytosis. Hematol Oncol Clin North Am 12(2):379–384
Egeler RM, D’Angio GJ (1995) Langerhans cell histiocytosis. J Pediatr 127(1):1–11
Schmidt S, Eich G, Hanquinet S, et al. (2004) Extra-osseous involvement of Langerhans’ cell histiocytosis in children. Pediatr Radiol 34(4):313–321
Schmidt S, Eich G, Geoffray A, et al. (2008) Extraosseous langerhans cell histiocytosis in children. Radiographics 28(3):707–726
Jubran RF, Marachelian A, Dorey F, Malogolowkin M (2005) Predictors of outcome in children with Langerhans cell histiocytosis. Pediatr Blood Cancer 45(1):37–42
Kim BE, Koh KN, Suh JK, et al. (2014) Clinical features and treatment outcomes of Langerhans cell histiocytosis: a nationwide survey from Korea histiocytosis working party. J Pediatr Hematol Oncol 36(2):125–133
Lieberman PH, Jones CR, Steinman RM, et al. (1996) Langerhans cell (eosinophilic) granulomatosis. A clinicopathologic study encompassing 50 years. Am J Surg Pathol 20(5):519–552
McClain KL, Natkunam Y, Swerdlow SH (2004) Atypical cellular disorders. Hematology Am Soc Hematol Educ Program 1:283–296
Braier J, Ciocca M, Latella A, et al. (2002) Cholestasis, sclerosing cholangitis, and liver transplantation in Langerhans cell Histiocytosis. Med Pediatr Oncol 38(3):178–182
Jaffe R (2004) Liver involvement in the histiocytic disorders of childhood. Pediatr Dev Pathol 7(3):214–225
Wong A, Ortiz-Neira CL, Reslan WA, et al. (2006) Liver involvement in Langerhans cell histiocytosis. Pediatr Radiol 36(10):1105–1107
Chan YL, Li CK, Lee CY (1997) Sonographic appearance of hepatic Langerhans cell histiocytosis. Clin Radiol 52(10):761–763
Kaplan KJ, Goodman ZD, Ishak KG (1999) Liver involvement in Langerhans’ cell histiocytosis: a study of nine cases. Mod Pathol 12(4):370–378
Meyer JS, Harty MP, Mahboubi S, et al. (1995) Langerhans cell histiocytosis: presentation and evolution of radiologic findings with clinical correlation. Radiographics 15(5):1135–1146
Egeler RM, Schipper ME, Heymans HS (1990) Gastrointestinal involvement in Langerhans’ cell histiocytosis (Histiocytosis X): a clinical report of three cases. Eur J Pediatr 149(5):325–329
Hyams JS, Haswell JE, Gerber MA, Berman MM (1985) Colonic ulceration in histiocytosis X. J Pediatr Gastroenterol Nutr 4(2):286–290
Geissmann F, Thomas C, Emile JF, et al. (1996) Digestive tract involvement in Langerhans cell histiocytosis. The French Langerhans Cell Histiocytosis Study Group. J Pediatr 129(6):836–845
Sutphen JL, Fechner RE (1986) Chronic gastroenteritis in a patient with histiocytosis-X. J Pediatr Gastroenterol Nutr 5(2):324–328
Rosai J, Dorfman RF (1969) Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol 87(1):63–70
Foucar E, Rosai J, Dorfman R (1990) Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 7(1):19–73
Sodhi KS, Suri S, Nijhawan R, Kang M, Gautam V (2005) Rosai-Dorfman disease: unusual cause of diffuse and massive retroperitoneal lymphadenopathy. Br J Radiol 78(933):845–847
Gaitonde S (2007) Multifocal, extranodal sinus histiocytosis with massive lymphadenopathy: an overview. Arch Pathol Lab Med 131(7):1117–1121
Juskevicius R, Finley JL (2001) Rosai-Dorfman disease of the parotid gland: cytologic and histopathologic findings with immunohistochemical correlation. Arch Pathol Lab Med 125(10):1348–1350
Maric I, Pittaluga S, Dale JK, et al. (2005) Histologic features of sinus histiocytosis with massive lymphadenopathy in patients with autoimmune lymphoproliferative syndrome. Am J Surg Pathol 29(7):903–911
Lauwers GY, Perez-Atayde A, Dorfman RF, Rosai J (2000) The digestive system manifestations of Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy): review of 11 cases. Hum Pathol 31(3):380–385
Esquivel J, Krishnan J, Jundi M, Sugarbaker PH (1999) Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) of the pancreas: first case report. Hepato-gastroenterology 46(26):1202–1205
Zivin SP, Atieh M, Mosier M, Paner GP, Aranha GV (2009) Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) of the pancreas: second case report. J Gastrointest Surg 13(4):806–809
Podberezin M, Angeles R, Guzman G, Peace D, Gaitonde S (2010) Primary pancreatic sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): an unusual extranodal manifestation clinically simulating malignancy. Arch Pathol Lab Med 134(2):276–278
Brown WE, Coakley FV, Heaney M (2002) Renal involvement by Rosai-Dorfman disease: CT findings. Abdom Imaging 27(2):214–216
Tabata H, Hisasue S, Tsukamoto T (2012) Extranodal Rosai-Dorfman disease of the kidney and bone. Int J Urol 19(5):486–487
Alatassi H, Ray MB, Galandiuk S, Sahoo S (2006) Rosai-Dorfman disease of the gastrointestinal tract: report of a case and review of the literature. Int J Surg Pathol 14(1):95–99
Chester W (1930) Über lipoid Granulomatose. Virchows Arch Pathol Anat 279:561–602
Chetritt J, Paradis V, Dargere D, et al. (1999) Chester-Erdheim disease: a neoplastic disorder. Hum Pathol 30(9):1093–1096
Al-Quran S, Reith J, Bradley J, Rimsza L (2002) Erdheim-Chester disease: case report, PCR-based analysis of clonality, and review of literature. Mod Pathol 15(6):666–672
Surabhi VR, Menias C, Prasad SR, et al. (2008) Neoplastic and non-neoplastic proliferative disorders of the perirenal space: cross-sectional imaging findings. Radiographics 28(4):1005–1017
Ivan D, Neto A, Lemos L, Gupta A (2003) Erdheim-Chester disease: a unique presentation with liver involvement and vertebral osteolytic lesions. Arch Pathol Lab Med 127(8):e337–e339
Gundling F, Nerlich A, Heitland WU, Schepp W (2007) Biliary manifestation of Erdheim-Chester disease mimicking Klatskin’s carcinoma. Am J Gastroenterol 102(2):452–454
Weitzman S (2011) Approach to hemophagocytic syndromes. Hematol Am Soc Hematol Educ Program 2011:178–183
Janka GE (2007) Hemophagocytic syndromes. Blood Rev 21(5):245–253
Fitzgerald NE, MacClain KL (2003) Imaging characteristics of hemophagocytic lymphohistiocytosis. Pediatr Radiol 33(6):392–401
Nakatsuka A, Wada J, Nagase R, et al. (2007) Hemophagocytic syndrome associated with fatal veno-occlusive disease in the liver. Intern Med 46(8):495–499
Wilejto M, Abla O (2012) Langerhans cell histiocytosis and Erdheim-Chester disease. Curr Opin Rheumatol 24(1):90–96
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Souza Maciel Rocha Horvat, N., Coelho, C.R., Roza, L.C. et al. Spectrum of abdominal imaging findings in histiocytic disorders. Abdom Imaging 40, 2738–2746 (2015). https://doi.org/10.1007/s00261-015-0449-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0449-1