Abstract
Benign or malignant diseases confined to the liver can be associated with inflammation, including lymphoid or plasmacytic infiltrate, and can rarely mimic neoplastic hematopoietic disorders. These differential diagnoses have received limited attention in the literature. Understanding the patterns of liver histology caused by lymphoma and various non-neoplastic inflammatory pathologies is essential, as the differential diagnosis varies depending on whether an inflammatory infiltrate primarily involves portal tracts, primarily involves sinusoids, or forms a discrete mass lesion.
The differential diagnosis for pathologic enlargement of the spleen is broad. As a hematopoietic organ, the spleen is a site of primary lymphoma, but also manifests pathologic abnormalities in a variety of infectious diseases, hematologic disorders, and systemic inflammatory disorders that may mimic primary or secondary involvement by a hematopoietic malignancy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Benign or malignant diseases confined to the liver can be associated with inflammation, including lymphoid or plasmacytic infiltrate, and can rarely mimic neoplastic hematopoietic disorders. These differential diagnoses have received limited attention in the literature. Understanding the patterns of liver histology caused by lymphoma and various non-neoplastic inflammatory pathologies is essential, as the differential diagnosis varies depending on whether an inflammatory infiltrate primarily involves portal tracts, primarily involves sinusoids, or forms a discrete mass lesion [1].
The differential diagnosis for pathologic enlargement of the spleen is broad. As a hematopoietic organ, the spleen is a site of primary lymphoma, but also manifests pathologic abnormalities in a variety of infectious diseases, hematologic disorders, and systemic inflammatory disorders that may mimic primary or secondary involvement by a hematopoietic malignancy. The pathologic differential for splenomegaly differs depending on whether it exhibits diffuse homogenous enlargement or radiographically discrete heterogenous masses. Careful gross examination and radiographic correlation are critical to determine areas for proper histologic sampling. Furthermore, ancillary studies are often needed, including flow cytometry and genetic analysis. In the chapter, we will focus on common systemic infections as well as non-infectious inflammatory disorders involving the liver and spleen. Pathologists should be familiar with the etiology and histologic changes in these diseases.
Systemic Infections
Epstein-Barr Virus
Epstein-Barr virus (EBV) belongs to the Gammaherpesvirinae subfamily of herpes viruses. Similar to other herpes viruses, it also exhibits the tendency of establishing latency in the host [2]. Acute viral infection gives rise to lifelong latent infection and affects nearly 90% of individuals depending on geographic location. The exact role of EBV infection in chronic liver disease may be either as a silent companion or as a causative agent [3]. In healthy individuals, primary EBV infection results in transient viremia and activation of cytotoxic T cells, while in an immune-compromised setting, the repeated activation of EBV infection or reactivation leads to B-cell immortality and eventually development of a clonal B-cell lymphoproliferative disorder or lymphoma [4, 5].
Mononucleosis is a systemic response to acute EBV infection (also refer to Chap. 20) and clinically can manifest with hepatosplenomegaly in addition to acute infectious signs and symptoms (fever, sore throat, swollen glands). Rupture of the spleen can occur with rapid increase in splenic size [6, 7]. When a patient develops B symptoms, weight loss, lymphadenopathy, and/or organomegaly, lymphoma may be clinically suspected until laboratory study demonstrates a positive Monospot (heterophile antibody) test. Positive serology for EBV infection [antiviral capsid antigen, anti-VCA IgM and IgG, anti-early antigen (EA) IgG, and anti-EBV nuclear antigen (anti-EBNA)] usually develops weeks or months after Monospot test [6, 8, 9]. Thus, the diagnosis of infectious mononucleosis is primarily based on clinical observation and immediate laboratory assessment, while a biopsy of spleen or liver is not indicated clinically.
Forms of chronic hepatic EBV infection include chronic active EBV infection (CAEBV) , EBV-associated chronic hepatitis, EBV infection/reactivation post-transplant, and EBV-associated hepatocellular carcinoma. The former two entities are included in differential diagnoses of primary EBV-positive hepatic lymphomas, while the latter two settings are not discussed in the chapters. CAEBV, though rare, is observed in patients with or without liver disease. It is diagnosed by abnormal EBV serology, histologic findings consistent with infection ( e.g., hepatitis), and EBV genome integration into the affected tissue [3]. The clinical course resembles a chronic or recurrent infectious mononucleosis [10].
EBV infection could be the trigger for other forms of hepatitis, including infectious (e.g., hepatitis B and C) or autoimmune-mediated disease [3, 11, 12]. The mechanisms are underinvestigated. It is proposed that EBV-specific T cells play an important role by producing various cytokines, including interleukin (IL)-1, IL-2, IL-10, and interferon-gamma (INF-gamma) [13].
Microscopic Features
Liver
An important mimic of hematopoietic neoplasia in the liver is involvement by Epstein-Barr virus (EBV), which can resemble hepatosplenic T-cell lymphoma (HSTCL) among other lymphomas. In EBV infection (mononucleosis), the sinusoids become engorged with numerous bland lymphocytes, which may also be present in portal tracts (Fig. 21.1) [14]. These lymphocytes are predominantly cytotoxic T cells (CD8-positive) [6]; scattered B cells are present in portal tracts and are infected with the virus, which can be demonstrated with EBV-encoded RNA (EBER) in situ hybridization [15].
A liver biopsy is usually not performed for chronic active EBV infection (CAEBV). However, EBV can be identified in EBV-associated chronic hepatitis via in situ hybridization assay using EBER [12] in addition to histologic evidence of chronic hepatitis.
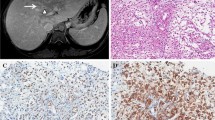
Spleen
Acute EBV infection (i.e., infectious mononucleosis) is commonly associated with splenomegaly, and is an important differential to consider or exclude in the evaluation of lymphoma. Florid follicular hyperplasia may give way to a marked atypical lymphoid hyperplasia that includes large reactive immunoblasts, which mimic lymphoma cells. Based on morphology, it is sometimes difficult to differentiate between acute EBV infection and a B-cell lymphoma such as diffuse large B-cell lymphoma. EBV infection in patients with a history of prior organ transplant can result in a polymorphous post-transplant lymphoproliferative disorder (PTLD) (Fig. 21.2).
Post-transplant lymphoproliferative disorder may have polymorphous morphology, with a wide spectrum of B-cell differentiation and even overt plasmacytoid appearance, as seen here. Individual large scattered immunoblasts are also present, not unlike the reactive atypical cells that can be seen in infectious mononucleosis
Differential Diagnosis
The differential between acute self-limited EBV infection and malignant lymphoproliferative disorder can be extremely challenging by morphology alone, and correlation with additional studies, including B cell clonality studies by flow cytometry, and genetic evaluation for chromosomal abnormalities by karyotyping, is advised.
In self-limited acute EBV infection, the large immunoblasts of concern typically provide a mottled appearance, alongside reactive histiocytes, plasma cells, and small lymphocytes, and should not extend into large sheets comparable to diffuse large B-cell lymphoma. Several aggressive T- or B-cell lymphomas must be excluded in accordance with clinicopathologic findings.
Hepatosplenic T-Cell Lymphoma
In a similar fashion, hepatosplenic T-cell lymphoma (HSTCL) occupies the sinusoids of the liver (Fig. 21.3) [16, 17]. Three findings can help distinguish this T-cell neoplasm, frequently expressing gamma-delta TCR, from EBV infection. First, the lymphoma cells should not involve the portal tracts, unlike the lymphocytes in EBV infection. Second, damaged or dying hepatocytes can be seen in severe EBV infection but should not be seen in lymphoma. Third, the cells in EBV infection retain CD5 immunoreactivity , whereas CD5 is usually negative in HSTCL [17, 18]. Clinical symptoms may overlap somewhat, as both processes can cause fever and hepatomegaly.
Other T- or B-Cell Lymphomas/Leukemias
Burkitt lymphoma, classic Hodgkin lymphoma, and a subset of diffuse large B-cell lymphoma, not otherwise specified, are frequently associated with EBV [19]. Involvement by the aforementioned lymphoma in the liver and/or spleen can occur [16, 20, 21]. A previously diagnosed lymphoma and the corresponding immunophenotypic changes help to confirm hepatic involvement by the lymphoma. Identification of clonal B cells via flow cytometry, immunohistochemical staining, or PCR study aids a final diagnosis. Coexisting CAEBV infection/reactivation and EBV-associated chronic hepatitis should be carefully sought in the liver biopsy if there are laboratory data supporting EBV infection.
Of note, hairy cell leukemia can also involve the liver sinusoids, though the appearance is often sufficiently distinct [22, 23]. In the spleen, hairy cell leukemia exhibits a unique infiltrating pattern: red pulp expansion and a “blood lake” appearance [24]. The hepatic infiltrating pattern is similar to chronic EBV infection. However, the unique immunophenotype of hairy cell leukemia (CD20+, CD11c+, CD25+, CD103+, Annexin 1+, and TRAP+) and BRAF V600E mutation provide an important diagnostic distinction [25].
Hairy cell leukemia is usually not associated with EBV infection. However, EBV-positive cells can be detected in the liver biopsy as bystanders if a chronic EBV hepatitis is present.
Cytomegalovirus
Cytomegalovirus (CMV) is a member of the Herpesviridae family. Reactivation of CMV often occurs in immunocompromised individuals, while acute infection could be acquired before or after birth or even in the adult [26]. Clinically, the infection is usually asymptomatic but can manifest with infectious mononucleosis-like signs or symptoms (fever, pharyngitis, lymphadenopathy, hepatosplenomegaly) [26]. Several laboratory methods (viral culture, direct immunofluorescence, DNA in situ hybridization, immunohistochemical staining, PCR for CMV DNA, and antigen tests) are used for diagnosis of CMV infection, in addition to morphologic assessment [26,27,28]. PCR is the most reliable way for monitoring the viral infection [28].
CMV hepatitis presents with a long-lasting fever, mildly elevated transaminases, and a low ratio of alanine aminotransferase to LDH. There are only mild histopathological changes found on liver biopsy. Atypical lymphocytosis and splenomegaly are two common findings [29].
Liver
While CMV infection may be associated with chronic inflammation, it is typically limited and involves a patchy periportal lymphocytic infiltrate and mild lobular hepatitis [29]. Apoptosis can be observed. However, there is no overt damage of hepatocytes, such as bridging necrosis, as can be found in hepatitis A, B, and, C [29]. In acute infection, or the mononucleosis-like syndrome, infiltrates within portal tracts and sinusoids may become more prominent. Micro abscesses may also be seen. The pathognomonic finding in CMV hepatitis is a classic cytomegalic cytopathic effect that may be seen in enlarged hepatocytes, endothelial cells, biliary epithelium, or sinusoidal macrophages (Kupffer cells) [29, 30]. There is massive nuclear and cytoplasmic enlargement with intranuclear inclusions (Cowdry type A) typical of herpesvirus infection (Fig. 21.4) [30]. Immunostaining for CMV antigen is often useful for highlighting virally infected cells.
Differential Diagnosis
Differential diagnoses should include, but not be limited to, EBV-driven infectious mononucleosis, other viral hepatitis, lymphoma, and graft-versus-host disease in patients status post solid organ transplantation. Morphologic evidence of cytomegalic cytopathic effect, Cowdry type A cells, and positive CMV immunohistochemical staining helps to confirm the presence of CMV infection [30].
Spleen
Architectural changes within the spleen attributable to CMV are somewhat similar to the mononucleosis-like changes of EBV, albeit typically less pronounced. Follicular hyperplasia, marginal zone proliferation, and sinusoidal proliferations of immunoblasts or plasma cells may be seen. In some severe cases, vasculitis and lymphocyte depletion may be seen. As above, characteristic cell enlargement and viral inclusions can be expected, and immunostaining for CMV is particularly helpful.
Human Immunodeficiency Virus
Human immunodeficiency virus (HIV) is the virus causing acquired immunodeficiency syndrome (AIDS) and is spread via contacting with the blood, semen, fluids, or breast milk of an HIV-positive individual. HIV infection can be divided into 4 clinical stages from asymptomatic to advanced disease, according to the WHO clinical staging system for HIV/AIDS. Opportunistic infections are commonly accompanied in stage IV disease [31].
Liver
A variety of histologic liver abnormalities are commonly seen in the setting of HIV, but virtually none are specific to this virus. Common findings include steatosis, marked iron deposition (related to transfusion history), granulomas associated with a variety of opportunistic infections, and high co-incidence of primary hepatotropic virus infection [32]. Importantly, when co-infection with HIV and hepatitis C virus (HCV) occurs, the severity of histologic damage from HCV may be worse, particularly with respect to more severe fibrosis and piecemeal necrosis [33, 34].
Spleen
Likewise, the most notable pathologic changes of the spleen associated with HIV/AIDS are not directly attributable to the virus itself, but largely reflect the sequelae of disease such as secondary opportunistic infections (e.g., CMV and atypical Mycobacterium) and AIDS-related malignancies/lymphomas. In the era before highly active antiretroviral therapy (HAART), white pulp depletion was more commonly seen [35]. Other histologic patterns that are likely attributable to systemic HIV infection include follicular hyperplasia and intraparenchymal plasmacytosis [36].
Malaria (Plasmodium species)
Malaria is caused by protozoan parasites of the genus Plasmodium spread through the bites of infected female Anopheles mosquitoes. It can cause life-threatening disease, but it is preventable and curable [37]. The two most common species (5 in total) – P. falciparum and P. vivax – are the most causative [37].
Diagnostic evaluation for presence and speciation of Plasmodium species is effectively performed on a routine blood smear. That being said, studies of the liver and spleen histopathology in malaria have revealed some correlative findings. The laboratory methods used for diagnosing malaria have been well established, including microscopic examination of peripheral blood films (thick and thin preparation), QBC staining, anti-malaria antibody (rapid diagnostic tests), serological tests, and molecular tests [37].
The liver stage of the disease is an obligatory phase in which sporozoites develop into merozoites, prior to red blood cell infection. In severe malaria, most commonly caused by P. falciparum, worsening liver damage is associated with severe hyperbilirubinemia and more extensive periportal inflammation, fatty change, and Kupffer cell hyperplasia [38].
Splenomegaly is also routinely found, and can be so severe as to cause splenic rupture. The degree of splenomegaly is likely attributable to a combination of congestion related to clearance of hemolyzed red cells, parasite clearance and sequestration, and cytokine-mediated inflammatory changes.
In endemic areas, hyperreactive malarial splenomegaly syndrome (HMSS) secondary to chronic malaria antigen stimulation is frequently observed, accounting for 31–76% of splenomegaly in different African countries, and which has a high mortality rate (up to 36% within 3 years) [39]. PCR is the most sensitive diagnostic tool when compared with histologic examination for microorganism inclusions in peripheral blood specimen, which is usually negative in the setting [40, 41].
Differential Diagnosis
Since histologic findings in both liver and spleen could be non-specific , identification of intracellular Plasmodium in red blood cells on peripheral smear or PCR study for the presence of Plasmodium DNA is critical for the establishment of malarial infection [37, 41].
Hemophagocytic Lymphohistiocytosis, Secondary (or Infection-Related)
Hemophagocytic lymphohistiocytosis (HLH) is a systemic inflammatory disorder (a.k.a. macrophage activation syndrome), in which natural killer (NK) and T-cell function become dysregulated, leading to uncontrolled immune system activation. The primary form of this disease is familial (i.e., genetic) and most frequently known to occur among patients with mutations in elements of the perforin cytotoxic pathway. Secondary HLH most commonly occurs in response to viral infection (HIV, EBV, or others), may be related to an underlying malignancy (e.g., T-cell lymphoma), and still in some cases is ultimately idiopathic [42]. Organomegaly (i.e., hepatosplenomegaly) is among one of the multiple diagnostic criteria; therefore, liver and splenic manifestations of HLH are important to recognize, as the liver may be among the most common tissues biopsied (following bone marrow) to document hemophagocytosis, and splenomegaly may be evaluated prior to clinical consideration of HLH in the diagnostic differential (also refer to Chap. 17).
Liver
HLH is another process that can lead to increased inflammatory cells within the sinusoids, potentially mimicking a hematopoietic disorder. Microscopic changes can vary widely but generally include hemophagocytosis by macrophages within the sinusoids, portal tract, and lobules (Fig. 21.5), along with increased lymphocytic inflammation in these areas. In some cases, the portal infiltrate is sufficiently heavy that HLH can also mimic a portal or intrasinusoidal malignant lymphoma [43].
Hemophagocytic lymphohistiocytosis can produce dense lymphocytic inflammation throughout the hepatic parenchyma and particularly within sinusoids. Careful histopathologic and clinical correlation is needed to exclude T-cell/histiocyte-rich large B-cell lymphoma, peripheral T-cell lymphoma, or hepatosplenic T-cell lymphoma
Spleen
Massive histiocytic infiltration of splenic red pulp occurs in HLH, accompanied by marked erythrophagocytosis. Histiocytes expand both sinuses and cords, with expanded but intact splenic architecture . Atrophy of the white pulp may be seen. Due to the normally high number of resident macrophages present in the splenic reticuloendothelial system, it may be difficult to surmise when HLH is present in less florid cases. As with other tissues, CD163 or CD68 immunostaining may help identify islands of erythrophagocytosis (i.e., nucleated red blood cells accumulated and enveloped within pockets of positively staining histiocytic cytoplasm).
Differential Diagnosis
The primary malignant differential for HLH in the liver is HSTCL or T-cell/histiocyte-rich large B-cell lymphoma (T/HRLBCL). Careful histologic evaluation and immunohistochemical staining for aberrant T cells and large atypical B cells is advised if lymphoma is suspected.
Granulomatous Infections
Necrotizing Granulomatous Inflammation
Widespread or hematogenous dissemination of invasive fungus (e.g., histoplasmosis) or Mycobacteria species (e.g., M. tuberculosis) can give rise to the tumor-like formation of necrotizing granulomata in the liver or spleen [44,45,46].
In both liver and splenic parenchyma, infiltration by variably sized organized granuloma can occur, typically without regard to specific architectural elements. Well-formed palisading walls of histiocytes are rimmed by small lymphocytes (predominantly CD4-positive T cells) and typically abundant necrotic debris (Fig. 21.6). The presence of necrosis strongly favors an infectious etiology, but by comparison, the presence of abundant non-necrotizing granulomata (which may frequently be presumed to correlate with systemic sarcoidosis) is an important mimic of the granulomatous variant of classic Hodgkin lymphoma (see discussion below).
Fibrin-Ring Granulomas
This peculiar type of granuloma is generally described in the liver. Small and rounded, they resemble epithelioid, non-caseating granulomas, though the center contains a damaged globule of fat surrounded by a fibrinous ring (hence the name) (Fig. 21.7). They are most strongly associated with Q fever, though they have been described in numerous other disease states, including EBV infection, cytomegalovirus hepatitis, and drug-induced liver injury (allopurinol, ipilimumab, and others) [47, 48]. They have also been described in patients with hepatic involvement by Hodgkin lymphoma, though most cases also show obvious evidence of involvement, with mixed inflammation and Reed-Sternberg cells involving portal tracts [16]. The presence of fibrin-ring granulomas in the liver should still at least raise the possibility of lymphoma, especially in patients with suggestive symptoms. Ultimately, however, a different diagnosis is more likely to be correct in any given case with this type of granuloma.
Parasitic Hydatid Cyst
Cystic parasitic lesions of the liver and spleen are rare, and due to their distinctive radiographic and gross appearance, they are not commonly included in the differential with hematopoietic disorders.
Hydatid cysts are caused by larval infection from the Echinococcus species of tapeworm, which is one step in a complicated developmental lifecycle that involves different stages in both intermediate and definitive hosts. Intermediate hosts develop the cystic form of the disease and are more severely affected due to disease dissemination of the oncosphere, which hatches from an ingested egg to penetrate the intestinal wall and disseminates systemically before forming hydatid cysts. Symptoms are related to mass effects of the enlarging cysts, and potentially severe inflammatory reactions when cysts rupture. In the United States, the most common species is E. granulosus, which typically forms uniloculated cysts in the liver and spleen, among other organs. Other species include E. multilocularis, E. oligarthus, and E. vogeli, the latter of which forms multiloculated cysts [49]. The liver is the most commonly affected organ, while isolated splenic cysts are uncommon and typically result from abdominal dissemination of a ruptured hepatic cyst. Histologically, the cyst wall has a characteristic lamellated appearance, with an outer fibrous layer and inner germinative layers of the organism in which parasitic structures such as hooklets and scolices can be found. Surrounding the cyst is an inflammatory infiltrate comprised predominantly of chronic lymphocytic inflammation, macrophages, and eosinophils [49].
Differential Diagnosis
Comparatively non-parasitic cysts and pseudocysts are much more common in Western populations. Splenic pseudocysts, which are more common than true cysts, lack an epithelial lining, are comprised of well-formed fibrous tissue, and typically result from lack of resorption from post-traumatic hemorrhage or hematoma, post-splenic infarction, and local regional inflammation. True cysts may contain either epithelial, mesothelial, or epidermoid lining.
Miscellaneous
On a final note, with respect to systemic infections , there are a myriad of other infectious agents that cause splenomegaly but are not routinely considered in the differential with lymphoma. These include brucellosis, echinococcosis, histoplasmosis, leishmaniasis, schistosomiasis, syphilis, toxoplasmosis, trypanosomiasis, and typhoid fever. The details are not discussed in the chapter.
Inflammatory Liver Disease
Viral Hepatitis
Hepatitis C Virus
In chronic HCV, the portal tracts of the liver become filled with a moderately dense inflammatory infiltrate composed predominantly of lymphocytes (Fig. 21.8) [50]. Lobular inflammation may also be present, though less striking . The portal inflammation is generally contained to that region, creating round contours clearly delineating the portal areas from the lobules. Severely affected portal tracts may show evidence of germinal center formation (Fig. 21.9). However, the portal tracts are not equally affected, meaning inflammation may be sparse in some.
Differential Diagnosis
The main potential mimic of lymphoma in the liver is chronic viral hepatitis, particularly hepatitis C (HCV), which can resemble liver involvement by CLL/SLL. Hepatic involvement by CLL/SLL somewhat resembles chronic HCV at low power, with the portal tracts involved by a chronic inflammatory infiltrate [16]. On closer inspection, however, the lymphocytes are packed slightly more densely than in HCV, and they appear monomorphic (Fig. 21.10). All portal tracts are involved to a similar degree. Additionally, the inflammation often spills beyond the portal tracts, causing irregular contours around the inflammatory foci. CLL/SLL should not induce liver fibrosis, unlike chronic HCV, so the presence of liver fibrosis (portal, periportal, bridging, or cirrhotic) generally favors the latter diagnosis.
Immunostains for CD5, CD20, and CD23 should all be positive in the lesional cells of CLL/SLL, helping confirm the diagnosis. In contrast, the inflammation seen in chronic HCV is predominantly CD4- and CD8-positive T cells, meaning CD20 and CD23 should be negative; B cells may be seen, particularly in the center of lymphoid aggregates [51].
Clinical history is the best method of distinguishing HCV from hepatic CLL/SLL. Serologic testing can easily determine a patient’s viral load. With the advent of new medication that can cure HCV (e.g., sofosbuvir), this once-common pathologic pattern of injury is becoming less frequently seen; loss of familiarity with this pattern may possibly increase the chance of misinterpretation.
Other Viral Hepatitides
In Western populations, other pathogens responsible for viral hepatitis include hepatitis A virus (HAV) and hepatitis B virus (HBV) , as well as other less common primary hepatotropic viruses (hepatitis D, E, and F viruses), adenovirus, and less common human herpesviruses. In tropical regions and lesser developed nations, pathogens of concern include yellow fever virus and other rare flaviviruses, along with numerous tropical, zoonotic, and hemorrhagic viruses (Filo-, Arena-, Bunya-, Corona-, Picorna-, and Reovirus family members). Clinical and laboratory tests help diagnose other viral hepatitides.
Granulomatous Hepatitis, Non-infectious
Non-necrotizing granulomas of the liver have a broad differential, as they may be primary to the liver (e.g., primary biliary cholangitis, autoimmune hepatitis), or the result of systemic disease (e.g., sarcoidosis, Crohn’s disease, systemic lupus erythematous) . Approximately 80% of sarcoidosis have hepatosplenic involvement [52]. Given this broad differential, which will often not yet be narrowed at the time of pathologic evaluation, it is critical to consider the possibility of the granulomatous pattern of classic Hodgkin lymphoma (particularly in patients with suspected systemic disease and lymphadenopathy). Rarely, the granulomatous inflammation can be so florid as to nearly obscure the presence of diagnostic Reed-Sternberg cells (Fig. 21.11).
(a and b) Abundant well-formed non-necrotizing granulomata and associated giant cells can be seen infiltrating throughout the liver parenchyma in sarcoidosis, among other inflammatory disorders (a). Care should be taken if there is any history or clinical suspicion of classic Hodgkin lymphoma to evaluate for elusive Hodgkin/Reed-Sternberg cells, which can hide within a prominent background granulomatous pattern (b)
Reactive Lymphoid Hyperplasia
Reactive lymphoid hyperplasia (pseudolymphoma) is an unusual localized inflammatory process that may mimic hepatocellular carcinoma clinically or a lymphoma microscopically [53]. Histology shows a well-demarcated nodular region composed of mature lymphocytes (B cells) forming follicles with germinal centers. Adjacent portal tracts may show similar inflammation. The differential diagnosis includes any lymphoma that can present as an isolated liver mass (such as T-cell/histiocyte rich B-cell lymphoma). Molecular studies help confirm the benign, polyclonal nature of this rare process.
Splenomegaly, Non-infectious
Extramedullary Hematopoiesis (Also See Chap. 17)
Hematopoiesis occurs outside of the bone marrow (medullary) cavity in adults under a variety of malignant and benign conditions that impair or limit normal blood growth [54]. Examples include bone marrow irradiation, thalassemia, infectious and inflammatory syndromes, primary or secondary bone marrow fibrosis, and marrow infiltration by metastatic cancer [54]. Extramedullary hematopoiesis (EMH) in different organs or tissue is characterized by the appearance of trilineage hematopoietic precursors, including megakaryocytes, nucleated erythroid precursors, and early myeloid precursors (myelocytes, promyelocytes, and myeloblasts) (Fig. 21.12). The liver and spleen are the two most frequent sites of EMH secondary to myeloproliferative neoplasms (MPN) or EMH without MPN [54, 55]. Resultant splenomegaly easily triples or quadruples normal spleen size (e.g., easily exceeding 1000 grams in weight). Pathologic EMH must be conceptually distinguished from physiologic or primary EMH, which occurs as a normal part of embryologic development prior to 4–5 months’ gestational age [56].
Fibrocongestive Splenomegaly
Longstanding portal hypertension, due to a variety of conditions including liver cirrhosis, congestive heart failure, portal vain stenosis, and thrombosis of portal veins, hepatic veins (i.e., Budd-Chiari syndrome) or splenic veins, may cause chronic red pulp congestion, sinusoidal dilatation, and fibrotic changes. Histologically dilated veins and sinuses can be seen (Fig. 21.13), along with hemosiderin-laden macrophages, fibrosis of red pulp, normal or attenuated white pulp, and Gamna-Gandy body formation (see below). Fibrocongestive splenomegaly is not an uncommon finding in patients with sickle cell disease (see separate chapter) [57].
(a and b) Fibrocongestive splenomegaly shows large areas of the spleen overtaken by congested sinusoids packed with red blood cells. Residual areas of normal splenic parenchyma may persist (a). At higher power, the most fibrocongestive areas are devoid of white pulp lymphocytes and contain fibroblastic and reticular cell proliferations (b)
Gamna-Gandy Bodies
Chronic hemolysis, infarction of the spleen, or fibrocongestive changes can result in excessive iron deposition and dystrophic calcification within dense fibrotic lesions of the spleen known as Gamna-Gandy bodies. This phenomenon most commonly occurs in sickle cell anemia, but other conditions where they may be seen include portal hypertension, acquired hemochromatosis, and patients with chronic blood transfusion [58]. These deposits are siderotic, pigment-laden lesions that show up on a variety of imaging techniques, including magnetic resonance imaging and ultrasound. They may be mistaken for tumor-forming masses within the spleen. On gross examination, these nodules more likely mimic desmoplastic reaction to metastatic tumor than the soft tissue appearance of lymphoma. Histologic sectioning reveals distinct pigment deposition that is rust-to-yellow-to-black in color (Fig. 21.14) . They are pathologically insignificant, but in rare cases require clinical correlation with a preceding history of hemolysis or iron overload.
Diagnostic Caveats
-
1.
Certain benign or malignant diseases confined to the liver can be associated with inflammation, including a lymphoid or plasmacytic infiltrate, that rarely mimics neoplastic hematopoietic disorders. Of note, dense lymphoid infiltrate in HCV hepatitis could mimic chronic lymphocytic leukemia/small lymphocytic lymphoma, and infectious mononucleosis may resemble hepatosplenic T-cell lymphoma. Acute or chronic EBV infection should be distinguished from EBV-associated lymphomas.
-
2.
It is important to know the patterns of liver histology caused by lymphoma and various non-neoplastic inflammatory pathologies, since the differential diagnosis varies depending on whether an inflammatory infiltrate primarily involves portal tracts, primarily involves sinusoids, or forms a discrete mass lesion.
-
3.
Whether a disease process causes diffuse homogenous enlargement or radiographically discrete heterogenous masses in the spleen provides diagnostic clues in patients with splenomegaly. Careful gross examination and radiographic correlation are critical to determine areas for proper histologic sampling.
-
4.
It is important to correlate with clinical history as well as laboratory findings to identify infectious etiologies, and to distinguish autoimmune disease, secondary inflammatory conditions, or granulomatous processes from neoplastic hematopoietic disorders.
-
5.
Furthermore, ancillary studies are often needed, including immunohistochemical study, flow cytometry, and genetic analysis, to exclude hematopoietic malignancy. In the situation, adequate tissue biopsy tissue is essential.
References
Baumhoer D, Tzankov A, Dirnhofer S, Tornillo L, Terracciano LM. Patterns of liver infiltration in lymphoproliferative disease. Histopathology. 2008;53(1):81–90.
Cohen JI. Epstein-Barr virus infection. N Engl J Med. 2000;343(7):481–92.
Petrova M, Kamburov V. Epstein-Barr virus: silent companion or causative agent of chronic liver disease? World J Gastroenterol. 2010;16(33):4130–4.
Maurmann S, Fricke L, Wagner HJ, et al. Molecular parameters for precise diagnosis of asymptomatic Epstein-Barr virus reactivation in healthy carriers. J Clin Microbiol. 2003;41(12):5419–28.
Richinson A, Kieff E. Epstein-Barr virus. In: Knipe D, Howley P, editors. Tields virology. Vol 1 and 2. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 2575–627.
CDC. Epstein-barr virus and infectious mononucleosis: laboratory testing. https://www.cdc.gov/epstein-barr/laboratory-testing.html. Updated 2018.
Handin R. Blood: pricinples and practice of hematology. Philadelphia: Lippincott Williams & Wilkins; 2003.
Mononucleosis. https://www.mayoclinic.org/diseases-conditions/mononucleosis/diagnosis-treatment/drc-20350333. Accessed 6 Aug 2017.
Elgh F, Linderholm M. Evaluation of six commercially available kits using purified heterophile antigen for the rapid diagnosis of infectious mononucleosis compared with Epstein-Barr virus-specific serology. Clin Diagn Virol. 1996;7(1):17–21.
Straus SE. The chronic mononucleosis syndrome. J Infect Dis. 1988;157(3):405–12.
Vento S, Cainelli F. Is there a role for viruses in triggering autoimmune hepatitis? Autoimmun Rev. 2004;3(1):61–9.
Drebber U, Kasper HU, Krupacz J, et al. The role of Epstein-Barr virus in acute and chronic hepatitis. J Hepatol. 2006;44(5):879–85.
Jabs WJ, Wagner HJ, Schlenke P, Kirchner H. The primary and memory immune response to Epstein-Barr virus infection in vitro is characterized by a divergent production of IL-1beta/IL-6 and IL-10. Scand J Immunol. 2000;52(3):304–8.
Suh N, Liapis H, Misdraji J, Brunt EM, Wang HL. Epstein-Barr virus hepatitis: diagnostic value of in situ hybridization, polymerase chain reaction, and immunohistochemistry on liver biopsy from immunocompetent patients. Am J Surg Pathol. 2007;31(9):1403–9.
Niedobitek G, Agathanggelou A, Steven N, Young LS. Epstein-Barr virus (EBV) in infectious mononucleosis: detection of the virus in tonsillar B lymphocytes but not in desquamated oropharyngeal epithelial cells. Mol Pathol. 2000;53(1):37–42.
Loddenkemper C, Longerich T, Hummel M, et al. Frequency and diagnostic patterns of lymphomas in liver biopsies with respect to the WHO classification. Virchows Arch. 2007;450(5):493–502.
Shi Y, Wang E. Hepatosplenic T-cell lymphoma: a clinicopathologic review with an emphasis on diagnostic differentiation from other T-cell/natural killer-cell neoplasms. Arch Pathol Lab Med. 2015;139(9):1173–80.
Kaplan D, Smith D, Meyerson H, Pecora N, Lewandowska K. CD5 expression by B lymphocytes and its regulation upon Epstein-Barr virus transformation. Proc Natl Acad Sci U S A. 2001;98(24):13850–3.
Castillo JJ, Beltran BE, Miranda RN, Paydas S, Winer ES, Butera JN. Epstein-barr virus-positive diffuse large B-cell lymphoma of the elderly: what we know so far. Oncologist. 2011;16(1):87–96.
Fugl A, Andersen CL. Epstein-Barr virus and its association with disease – a review of relevance to general practice. BMC Fam Pract. 2019;20(1):62.
Biemer JJ. Hepatic manifestations of lymphomas. Ann Clin Lab Sci. 1984;14(4):252–60.
Yam LT, Janckila AJ, Chan CH, Li CY. Hepatic involvement in hairy cell leukemia. Cancer. 1983;51(8):1497–504.
Choi WT, Gill RM. Hepatic lymphoma diagnosis. Surg Pathol Clin. 2018;11(2):389–402.
Wotherspoon A, Attygalle A, Mendes LS. Bone marrow and splenic histology in hairy cell leukaemia. Best Pract Res Clin Haematol. 2015;28(4):200–7.
Kreitman RJ, Arons E. Update on hairy cell leukemia. Clin Adv Hematol Oncol. 2018;16(3):205–15.
Kaye K. Cytomegalovirus (CMV) infection. https://www.merckmanuals.com/home/infections/herpesvirus-infections/cytomegalovirus-cmv-infection. Accessed 27 May 2019.
Eguchi H, Horita N, Ushio R, et al. Diagnostic test accuracy of antigenaemia assay for PCR-proven cytomegalovirus infection-systematic review and meta-analysis. Clin Microbiol Infect. 2017;23(12):907–15.
Weinberg A, Hodges TN, Li S, Cai G, Zamora MR. Comparison of PCR, antigenemia assay, and rapid blood culture for detection and prevention of cytomegalovirus disease after lung transplantation. J Clin Microbiol. 2000;38(2):768–72.
Kunno A, Abe M, Yamada M, Murakami K. Clinical and histological features of cytomegalovirus hepatitis in previously healthy adults. Liver. 1997;17(3):129–32.
Colina F, Juca NT, Moreno E, et al. Histological diagnosis of cytomegalovirus hepatitis in liver allografts. J Clin Pathol. 1995;48(4):351–7.
Weinberg JL, Kovarik CL. The WHO clinical staging system for HIV/AIDS. Virtual Mentor. 2010;12(3):202–6.
Wilkins MJ, Lindley R, Dourakis SP, Goldin RD. Surgical pathology of the liver in HIV infection. Histopathology. 1991;18(5):459–64.
Garcia-Samaniego J, Soriano V, Castilla J, et al. Influence of hepatitis C virus genotypes and HIV infection on histological severity of chronic hepatitis C. The Hepatitis/HIV Spanish Study Group. Am J Gastroenterol. 1997;92(7):1130–4.
Mohsen AH, Easterbrook PJ, Taylor C, et al. Impact of human immunodeficiency virus (HIV) infection on the progression of liver fibrosis in hepatitis C virus infected patients. Gut. 2003;52(7):1035–40.
Diaz LK, Murphy RL, Phair JP, Variakojis D. The AIDS autopsy spleen: a comparison of the pre-anti-retroviral and highly active anti-retroviral therapy eras. Mod Pathol. 2002;15(4):406–12.
Falk S, Muller H, Stutte HJ. The spleen in acquired immunodeficiency syndrome (AIDS). Pathol Res Pract. 1988;183(4):425–33.
Tangpukdee N, Duangdee C, Wilairatana P, Krudsood S. Malaria diagnosis: a brief review. Korean J Parasitol. 2009;47(2):93–102.
Viriyavejakul P, Khachonsaksumet V, Punsawad C. Liver changes in severe Plasmodium falciparum malaria: histopathology, apoptosis and nuclear factor kappa B expression. Malar J. 2014;13:106.
Leoni S, Buonfrate D, Angheben A, Gobbi F, Bisoffi Z. The hyper-reactive malarial splenomegaly: a systematic review of the literature. Malar J. 2015;14:185.
Mothe B, Lopez-Contreras J, Torres OH, Munoz C, Domingo P, Gurgui M. A case of hyper-reactive malarial splenomegaly. The role of rapid antigen-detecting and PCR-based tests. Infection. 2008;36(2):167–9.
SM AE, El-Rayah el A, Giha HA. Validation of PCR for detection and characterization of parasitaemia in massive splenomegaly attributed clinically to malaria infection. Diagn Microbiol Infect Dis. 2011;70(2):207–12.
George MR. Hemophagocytic lymphohistiocytosis: review of etiologies and management. J Blood Med. 2014;5:69–86.
Chen JH, Fleming MD, Pinkus GS, et al. Pathology of the liver in familial hemophagocytic lymphohistiocytosis. Am J Surg Pathol. 2010;34(6):852–67.
Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev. 2007;20(1):115–32.
Lee DG, Choi JH, Kim YJ, et al. Hepatosplenic tuberculosis mimicking disseminated candidiasis in patients with acute leukemia. Int J Hematol. 2001;73(1):119–21.
Gupta PP, Fotedar S, Agarwal D, Sansanwal P. Tuberculosis of spleen presenting with pyrexia of unknown origin in a non-immunocompromised woman. Lung India. 2008;25(1):22–4.
Everett J, Srivastava A, Misdraji J. Fibrin ring granulomas in checkpoint inhibitor-induced hepatitis. Am J Surg Pathol. 2017;41(1):134–7.
Marazuela M, Moreno A, Yebra M, Cerezo E, Gomez-Gesto C, Vargas JA. Hepatic fibrin-ring granulomas: a clinicopathologic study of 23 patients. Hum Pathol. 1991;22(6):607–13.
Pedrosa I, Saiz A, Arrazola J, Ferreiros J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20(3):795–817.
Goodman ZD, Ishak KG. Histopathology of hepatitis C virus infection. Semin Liver Dis. 1995;15(1):70–81.
Tucci FA, Broering R, Lutterbeck M, Schlaak JF, Kuppers R. Intrahepatic B-cell follicles of chronically hepatitis C virus-infected individuals lack signs of an ectopic germinal center reaction. Eur J Immunol. 2014;44(6):1842–50.
Vardhanabhuti V, Venkatanarasimha N, Bhatnagar G, et al. Extra-pulmonary manifestations of sarcoidosis. Clin Radiol. 2012;67(3):263–76.
Lv A, Liu W, Qian HG, Leng JH, Hao CY. Reactive lymphoid hyperplasia of the liver mimicking hepatocellular carcinoma: incidental finding of two cases. Int J Clin Exp Pathol. 2015;8(5):5863–9.
Fan N, Lavu S, Hanson CA, Tefferi A. Extramedullary hematopoiesis in the absence of myeloproliferative neoplasm: Mayo Clinic case series of 309 patients. Blood Cancer J. 2018;8(12):119.
Tefferi A. Primary myelofibrosis: 2019 update on diagnosis, risk-stratification and management. Am J Hematol. 2018;93(12):1551–60.
Kim CH. Homeostatic and pathogenic extramedullary hematopoiesis. J Blood Med. 2010;1:13–9.
Chopra R, Al-Mulhim AR, Al-Baharani AT. Fibrocongestive splenomegaly in sickle cell disease: a distinct clinicopathological entity in the Eastern province of Saudi Arabia. Am J Hematol. 2005;79(3):180–6.
Selcuk D, Demirel K, Kantarci F, Mihmanli I, Ogut G. Gamna-Gandy bodies: a sign of portal hypertension. Turk J Gastroenterol. 2005;16(3):150–2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gonzalez, R.S., Evans, A.G. (2020). Infectious and Inflammatory Mimickers of Hematopoietic Disorders in the Liver and Spleen. In: Zhang, L., Shao, H., Alkan, S. (eds) Diagnostic Pathology of Hematopoietic Disorders of Spleen and Liver. Springer, Cham. https://doi.org/10.1007/978-3-030-37708-3_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-37708-3_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-37707-6
Online ISBN: 978-3-030-37708-3
eBook Packages: MedicineMedicine (R0)