Abstract
Background
We describe different possible enhancement patterns in liver hemangiomas with atypical appearance on baseline ultrasound after microbubble-based contrast agent injection.
Methods
From a series of 253 consecutive lesions that were indeterminate on baseline ultrasound and then scanned after injection of air-filled microbubble contrast agent, 65 focal liver lesions were retrospectively selected on the basis of a diagnosis of liver hemangioma on multiphase contrast-enhanced computed tomography (n = 23), magnetic resonance imaging (n = 27), or histology (n = 15). Each lesion was scanned during arterial phase (30 s after microbubble injection) and late phase (5 min after injection). On-site sonologists performed retrospective assessment of contrast-enhancement patterns by consensus.
Results
Centripetal fill-in preceded (n = 50) or not preceded (n = 3) by peripheral nodular/rim-like enhancement was the prevalently observed contrast-enhancement pattern, equivalent to the typical enhancement pattern of liver hemangiomas on contrast-enhanced computed tomography or magnetic resonance imaging. In the remaining lesions, additional enhancement patterns (diffuse contrast enhancement with rapid fill-in and a late hyper-isoechoic appearance, n = 6; peripheral nodular enhancement with a late hypoechoic appearance, n = 3; or persistent heterogeneous and hyperechoic appearance, n = 3) were observed.
Conclusion
Different contrast-enhancement patterns are possible in atypical liver hemangiomas after microbubble injection. Typical centripetal fill-in is the prevalent pattern and its evidence allows diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Liver hemangiomas may demonstrate a typical appearance on baseline gray-scale ultrasound (US) [1] that consists of a hyperechoic and homogeneous or centrally heterogeneous pattern, with or without posterior acoustic enhancement [2] and well-defined regular margins. In addition to this typical appearance, liver hemangiomas can present different atypical patterns on baseline US: homogeneous or heterogeneous, hypoechoic or isoechoic, with or without a thin peripheral echoic border [2]. These features make incidental hemangiomas indeterminate on baseline US. Even though typical liver hemangiomas do not need further confirmatory studies [3], benign (focal fatty changes, hepatocellular adenomas, focal nodular hyperplasia, and lipoma) or malignant (hepatocellular carcinomas and metastases) focal liver lesions may present similar appearances on baseline US [1]. Compared with baseline US, color Doppler US shows moderate accuracy in characterizing hemangiomas and, in general, focal liver lesions [4, 5] and may be limited by motion artifacts and low sensitivity to slow flows.
Microbubble-based contrast agents and dedicated US contrast-specific modes have been introduced to overcome color Doppler US limitations in characterizing focal liver lesions and to allow dynamic evaluation of contrast enhancement as in computed tomography (CT) [6–8] or magnetic resonance (MR) imaging [9]. One of the most commonly used microbubble-based agents is Levovist (SH U 508 A, Schering, Berlin, Germany), which is licensed in many European countries. It consists of air-filled microbubbles that are covered by a layer of galactose and palmitic acid and has been found to improve diagnostic performance in the characterization of focal liver lesions [10–13].
This report describes the different morphologic patterns of enhancement after microbubble-based contrast agent injection in liver hemangiomas with atypical appearance on baseline US.
Materials and methods
Patients
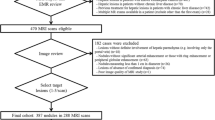
Over 5 years 253 consecutive focal liver lesions in 220 patients (117 men and 103 women, age range 35–80 years, median age 57 years) from two hospitals underwent scanning after injection of a Levovist bolus (2.5 g, rate 300 mg/mL). This was done because focal liver lesions appeared indeterminate on baseline scans and on-site sonologists expressed no definite diagnosis of the nature (benign or malignant) or histology of the lesions. Four on-site sonologists, two from each hospital, were involved. Medical records and radiology files of these patients were reviewed, and 65 lesions in 59 patients (35 men and 24 women, age range 35–70 years, median age 53 years) with one (53 patients) or two (six patients) lesions were retrospectively selected on the basis of a definite diagnosis of hemangioma obtained from reference standards [14].
All patients involved in this study gave their full informed consent for Levovist injection; approval of our institutional review board was not necessary because Levovist is commercially available in Italy. The procedure was done in accord with the Declaration of Helsinki as revised in 1989.
Baseline scan
Each sonologists had at least 5 years of experience in liver imaging and at least 3 years in liver applications of microbubble-based contrast agents. At the time of scanning, on-site sonographers were aware of patients’ clinical histories but were blinded to the final diagnosis. Different state-of-the-art US digital machines (Table 1) with low wideband frequency (2 to 5 MHz) convex-array transducers were used.
Baseline gray-scale US was performed by employing noise and speckle-decreasing tissue harmonic and compound modes. Color Doppler US was performed by using slow-flow settings (pulse repetition frequency 800 to 1500 Hz, wall filter 50 Hz, high levels of color versus echo priority and color persistence). Color gain was changed dynamically during the examination to enhance color signals and avoid excessive noise. Size of the color box was adjusted to include the entire lesion in the field of view of the color image. Spectral analysis of central and peripheral vessels was performed by pulsed Doppler to visualize continuous venous or pulsatile arterial flows.
Contrast-specific modes
After a suitable acoustic window was identified, the US apparatus was set for contrast-specific mode. Because Levovist presents a low harmonic behavior if low transmit power mode is employed [10–12], intermittent high transmission power [10] was used to determine microbubble destruction with consequent emission of a wideband frequency signal. Intermittent US transmission was used to minimize microbubbles destruction. Different high transmission power modes were employed according to the available US equipment (Table 1). One focus was set immediately below the lesion to be assessed, frame rate was set to the lowest level (7 to 9 Hz), and the gray-scale gain was set immediately below the noise threshold.
Levovist was injected intravenously as a 2.5-g bolus, at a concentration of 300 mg/dL, with a 10-mL normal saline flush, by using a 20- or 22-gauge peripheral intravenous cannula. Thirty seconds after Levovist injection (arterial phase) high transmission power imaging (mechanical index 1.1 to 1.5) was turned on for 1 to 2 s to destroy microbubbles. Because the frame rate was set to 7 to 9 Hz, 7 to 18 frames were obtained. The same procedure was repeated 5 min (late phase) after Levovist injection. In patients with more than one lesion, the same procedure was repeated for each lesion at least 20 min after from the previous Levovist injection and after no bubbles were seen in liver portal vessels. Images were stored on MO disk for offline analysis.
Reference standards
The diagnosis of hemangioma was based on multiphase contrast-enhanced helical CT (n = 23 hemangiomas), MR imaging (n = 27), or histopathologic findings (n = 15) obtained from percutaneous core needle biopsy or surgical specimen. CT and MR studies were performed in all patients and included acquisition of nonenhanced and contrast -enhanced images including hepatic arterial dominant phase (25 to 35 s after injection of an intravenous bolus of contrast material), portal venous dominant phase (60 to 70 s), and late phase (2 to 5 min). Strict imaging criteria were applied, including nodular peripheral enhancement, isoattenuation to blood vessels, high signal intensity on T2-weighted images, and no size increase at 6 to 12 months [6–9, 13]. Histologic diagnosis of hemangioma was based on the presence of endothelial-lined vascular channels. The presence and amount of fibrosis within the hemangioma were also noted as evidence of thrombosis.
Off-site contrast-enhancement pattern analysis
After hemangiomas were retrospectively selected, images obtained from baseline and contrast-enhanced US scans were jointly reviewed by the sonologists involved in scanning by using Adobe Photoshop 7.0 (Adobe Systems Inc., Mountain View, CA, USA). Corresponding images obtained before and after Levovist injection were evaluated and matched as pairs on a computer screen. Analysis was performed by consensus. Readers attempted to determine size, baseline appearance, and contrast-enhancement patterns.
The largest diameter of the lesion was measured on baseline US. Because larger hemangiomas frequently appear heterogeneous [2], hemangiomas were grouped as lesions no larger than 3 cm and as lesions larger than 3 cm.
Lesion echogenicity on baseline and contrast-enhanced US scans was classified as hyperechoic, hypoechoic, or isoechoic according if signal intensity was higher, lower, or similar, respectively, to that of the adjacent liver. Lesion appearance was classified as homogeneous or heterogeneous according to the absence or presence, respectively, of different echogenicities in different portions of each lesion. Enhancement patterns [6–9, 13] were classified as peripheral nodular (continuous or discontinuous with nodular appearance), peripheral rim-like (continuous peripheral ring), or diffuse (enhancement of the entire lesion consisting of a rapid fill-in). Progression to complete or incomplete fill-in from peripheral enhancement was also noted [13].
Results
Appearance of hemangiomas on baseline scan
Diameters of hemangiomas were no larger than 3 cm (n = 27) or larger than 3 cm (n = 38), with a range of 1 to 11.5 cm (mean 4.5 cm).
Hemangiomas no larger than 3 cm appeared hypoechoic (n = 19), isoechoic (n = 3), or heterogeneous but prevalently hyperechoic (n = 5). In 15 of 19 hypoechoic liver hemangiomas no larger than 3 cm, the adjacent liver presented a diffuse hyperechoic fatty appearance, whereas four of 19 were observed in patients with chronic liver disease. Heterogeneous but prevalently hyperechoic liver hemangiomas were observed in patients with proved colon malignancy (n = 3) or chronic liver disease (n = 2).
Hemangiomas larger than 3 cm appeared heterogeneous, prevalently hypoechoic (n = 31), isoechoic (n = 2), or hyperechoic (n = 5). In 25 of 31 hypoechoic liver hemangiomas larger than 3 cm, the liver was normal, whereas six of 31 were observed in patients with proved colon (n = 4) or lung (n = 2) malignancy. Isoechoic and hyperechoic liver hemangiomas larger than 3 cm were observed in normal liver.
Peripheral (n = 12) or peripheral and intranodular (n = 53) arterial and/or venous vessels were identified on color Doppler US.
Appearance of hemangiomas oncontrast-enhanced US
In 50 lesions that were no larger than 3 cm (n = 15) or larger than 3 cm (n = 35), peripheral nodular (n = 38) or rim-like (n = 12) contrast enhancement followed by centripetal fill-in was observed (Fig. 1). In four hemangiomas larger than 3 cm, centripetal fill-in spared a central portion of the lesion (Fig. 1). Hemangiomas appeared isoechoic (n = 7) or hyperechoic (n = 43) at late phase.
A 65-year-old man with a primary colon malignancy, C3 mode. A On conventional US, a hypoechoic lesion (arrowheads) that is slightly heterogeneous is identified in the right liver lobe. Nodular peripheral enhancement (arrowheads) is present at arterial phase (B) with centripetal fill-in and isoechoic appearance at late phase (C), sparing a central hypoechoic area (arrowheads).
In three heterogeneous and prevalently hyperechoic liver hemangiomas larger than 3 cm, progressive fill-in without evidence of centripetal progression (Fig. 2) was identified with isoechoic appearance to the adjacent liver at late phase. In these hemangiomas, the progressive fill-in involved the periphery and center of the lesion at the same time during arterial and late phases without evidence of peripheral nodular or rim-like enhancement.
A 50-year-old woman examined by routine US for abdominal pain, pulse inversion mode. A On conventional US, a hyperechoic lesion (arrows) that is slightly heterogeneous is identified in the right liver lobe. Progressive fill-in without centripetal progression 30 s (B) and 5 min (C) after bolus Levovist injection is seen.
In three hemangiomas no larger than 3 cm that were hypoechoic (n = 1) or heterogeneous hyperechoic (n = 2), a persistent peripheral nodular enhancement without evidence of centripetal progression (Fig. 3) was identified at arterial and late phases, with sparing of a central hypoechoic region. In these hemangiomas, a thrombotic or fibrosclerotic pattern was proved at histology.
A 55-year-old man with a primary colon malignancy, agent detection imaging. A On conventional US, a hyperechoic and slightly heterogeneous lesion (arrows) smaller than 3 cm is identified. Peripheral nodular enhancement is visible at arterial phase (B) with a hypoechoic appearance at late phase (C), without evidence of centripetal progression. Fibrosclerotic hemangioma was proved at histology from the resected specimen.
In six hypoechoic hemangiomas no larger than 3 cm, four of which were detected among patients with cirrhosis, diffuse contrast enhancement with rapid fill-in was observed, with hyperechoic appearance at arterial phase and hyperechoic (n = 2), isoechoic (n = 2), or slightly hypoechoic (n = 2) appearance at late phase (Fig. 4).
In three heterogeneous hyperechoic hemangiomas no larger than 3 cm, a persistent heterogeneous and hyperechoic appearance was identified during arterial and late phases without evidence of any defined enhancement pattern (Fig. 5).
Discussion
Hemangiomas are the most common benign tumors of the liver [14]. In addition to a typical homogeneous and hyperechoic appearance, liver hemangiomas may demonstrate different atypical patterns on baseline gray-scale US that could make characterization uncertain. Color Doppler US provides no typical feature in liver hemangiomas [4, 5, 15] that could allow differentiation from other focal liver lesions [16–18]. Motion artifacts, limitations in detecting tumoral vessels in deep liver lesions, and insensitivity to slow flows are other limitations of color Doppler US. Microbubble-based contrast agents and contrast-specific modes were introduced to overcome color Doppler US limitations and to improve US accuracy in characterization of focal liver lesions [19–20]. In particular, different contrast-enhancement patterns were described in liver hemangiomas with a typical or atypical appearance on baseline US, even though the most typical pattern was the peripheral globular with centripetal fill-in [10–12, 15, 16, 21].
In this series, we analyzed different dynamic patterns observed after Levovist injection in liver hemangiomas retrospectively selected from a series of focal liver lesions assessed as indeterminate on baseline US. The first finding of this study is that the injection of air-filled microbubble-based contrast agent showed peripheral nodular or rim-like enhancement with centripetal progression in most liver hemangiomas, resembling a contrast-enhancement pattern described previously on contrast-enhanced CT and MR imaging [6–9, 13] as typical and diagnostic for liver hemangiomas. In four hemangiomas larger than 3 cm, centripetal fill-in spared a central portion that probably corresponded to a central nonenhancing thrombotic or fibrotic region.
The second important finding of this study is that liver hemangiomas present a prevalently persistent bubble uptake at late phase with an isoechoic or hyperechoic appearance in relation to the adjacent liver. This was previously shown in benign liver lesions using color-coded contrast-specific modes as stimulated acoustic emission [22], and it was probably determined by the similar histologic pattern of benign lesions and liver parenchyma, as in focal nodular hyperplasia, or by microbubble pooling in vascular spaces, as in liver hemangiomas. The persistent bubble uptake observed at late phase could allow differentiation of hyper-enhancing, rapidly filling hemangiomas from malignant hypervascular liver lesions, such as hypervascular metastases or hepatocellular carcinomas, which appear hypoechoic at late phase as reported in previous studies [10–12, 23]. In any case, the isoechoic appearance at late phase may be sometimes observed in malignant liver lesions, as in hepatocellular carcinomas [10].
Rapidly filling hemangiomas are generally no larger than 3 cm [24] and correspond roughly to 16% to 18% of all hemangiomas [2]. In this series, rapidly filling hemangiomas with diffuse contrast enhancement at arterial phase were prevalently identified in patients with cirrhosis, as reported in previous series [24]. Even though diffuse contrast enhancement at arterial phase was observed prevalently in hepatocellular carcinomas [10–12], this pattern should not be considered exclusive to malignant lesions, particularly in patients with cirrhosis.
Persistent peripheral enhancement followed by a late central hypoechoic appearance was observed in a few liver hemangiomas that presented a fibrosclerotic pattern at histologic analysis. The progressive and complete fill-in of liver hemangiomas is a diagnostic pattern [6–9, 13], whereas incomplete fill-in with a hypoechoic central appearance at late phase is not because it may suggest the presence of a central scar or a central necrotic component as in malignant lesions [20].
Few hyperechoic hemangiomas no larger than 3 cm and with heterogeneous hyperechoic pattern showed a persistent heterogeneous hyperechoic appearance after Levovist injection. This was probably determined by the difficulty in identifying contrast enhancement in hyperechoic lesions, especially when using high transmission power, which does not allow effective signal suppression from native stationary tissues as does low transmission power, which may be employed with new-generation microbubbles filled with perfluorocarbon or sulfur hexafluoride.
Our study is limited by its retrospective nature and by the fact that sonographers were aware of the diagnosis of hemangioma at the time of retrospective analysis. Nevertheless, the aim of this study was the assessment of the appearance of hemangiomas after injection of microbubbles, which is probably not biased by awareness of the final diagnosis. Another limitation is that this study comprised only a description of the different contrast-enhancement patterns in liver hemangiomas, without assessment of the overall accuracy in the differential diagnosis from other focal liver lesions. The described patterns should be employed in a future prospective analysis to assess the diagnostic performance of contrast-enhanced US in focal liver lesion characterization. Another limitation is the employed technique using intermittent high transmission power mode. High transmission power insonation presents several drawbacks, such as transiency of harmonic signals, absent suppression of stationary tissue background, and the strong presence of artifacts produced by microbubble destruction. Low transmission power insonation produces a longer persistence of harmonic signals, effective suppression of stationary tissue background, and fewer artifacts. Low transmission power insonation is now possible with the employment of microbubbles that are filled with perfluorocarbon or sulfur hexafluoride [25].
In conclusion, contrast-specific modes with Levovist showed a progressive fill-in in most hemangiomas, which allowed diagnosis. Centripetal progression, with a final isoechoic or hyperechoic appearance, may be absent. Even though contrast-enhancement patterns appeared different in the remaining lesions, the benign nature of liver hemangiomas was suggested for the most part by their isoechoic or hyperechoic appearance at late phase due to persistent microbubble uptake, whereas only a few liver hemangiomas appeared hypoechoic at late phase, thus resembling malignant lesions.
References
Caturelli E, Pompili M, Bartolucci F, et al. (2001) Hemangioma-like lesions in chronic liver disease: diagnostic evaluation in patients. Radiology 220:337–342
Vilgrain V, Boulos L, Vullierme MP, et al. (2000) Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics 20:379–397
Leifer DM, Middleton WD, Teefey SA, et al. (2000) Follow-up of patients at low risk for hepatic malignancy with characteristic hemangioma at US. Radiology 214:167–172
Lee MG, Auh YH, Cho KS, et al. (1996) Color Doppler flow imaging of hepatocellular carcinomas. Comparison with metastatic tumors and hemangiomas by three step grading color hues. Clin Imaging 20:199–203
Nino-Murcia M, Ralls PW, Jeffrey RB Jr, Johnson M (1992) Color Flow Doppler characterization of focal hepatic lesions. AJR 159:1195–1197
Freeny PC, Marks WM (1986) Hepatic hemangioma: dynamic bolus computed tomography. AJR 147:711–719
Hanafusa K, Ohashi I, Himeno Y, et al. (1995) Hepatic hemangioma: findings with two phase CT. Radiology 196:465–469
Leslie DF, Johnson CD, MacCarty RL, et al. (1995) Single-pass CT of hepatic tumors: value of globular enhancement in distinguishing hemangiomas from hypervascular metastases. AJR 165:1403–1406
Semelka RC, Brown ED, Ascher SM, et al. (1994) Hepatic hemangiomas: a multi-institutional study of appearance on T2-weighted and serial gadolinium-enhanced gradient-echo MR images. Radiology 192:401–406
Bertolotto M, Dalla Palma L, Quaia E, Locatelli M (2000) Characterization of unifocal liver lesions with pulse inversion harmonic imaging after Levovist injection: preliminary results. Eur Radiol 9:1369–1376
Wilson SR, Burns PN, Murdali D, et al. (2000) Harmonic hepatic ultrasound with microbubble contrast agent: initial experience showing improved characterization of haemangioma, hepatocellular carcinoma and metastasis. Radiology 215:153–161
Tanaka S, Ioka T, Oshikawa O, et al. (2001) Dynamic sonography of hepatic tumors. AJR 177:799–805
Nino-Murcia M, Olcott EW, Jeffrey RB, et al. (2000) Focal liver lesions: pattern-based classification scheme for enhancement at arterial phase. Radiology 215:746–751
Ros PR. Computed tomography–pathologic correlations in hepatic tumors. In: Ferrucci JT, Mathiew DG, eds. Advances in hepatobiliary radiology. St. Louis: CV Mosby, 1990:75–108
Kim TH, Han JK, Kim AY, Choi BI (1999) Limitations of characterization of hepatic hemangiomas using an ultrasound contrast agent (Levovist) and power Doppler ultrasound. J Ultrasound Med 18:737–743
Tanaka S, Kitamura T, Fujita M, et al. (1990) Color Doppler flow imaging of liver tumors. AJR 154:509–514
Tano S, Ueno N, Tomiyama T, Kimura K (1997) Possibility of differentiating small hyperechoic liver tumours using contrast enhanced colour Doppler ultrasonography: a preliminary study. Clin Radiol 52:41–45
Wang LY, Wang JH, Lin ZY, et al. (1997) Hepatic focal nodular hyperplasia: findings on color Doppler ultrasound. Abdom Imaging 22:178–181
Kim TK, Choi BI, Han JK, et al. (2000) Hepatic tumours: contrast agent-enhancement patterns with pulse inversion harmonic US. Radiology 216:411–417
Harvey CJ, Blomley MJK, Cosgrove DO, et al. (2000) Is the presence of an echogenic rim around focal liver lesions imaged in the late phase of liver specific ultrasound microbubbles in phase inversion mode specific to malignancy? Radiology 217(P):304
Quaia E, Bertolotto M, Dalla Palma L (2002) Characterization of liver hemangiomas with pulse inversion harmonic imaging. Eur Radiol 12:537–544
Blomley MJK, Sidhu PS, Cosgrove DO, et al. (2001) Do different types of liver lesions differ in their uptake of the microbubble contrast agent SHU-508 A in the late liver phase? Early experience. Radiology 220:661–667
Kim T, Federle MP, Baron RL, et al. (2001) Discrimination of small hepatic hemangiomas from hypervascular malignant tumors smaller than 3 cm with three-phase helical CT. Radiology 219:699–706
Brancatelli G, Federle MP, Blachar A, Grazioli L (2001) Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology 219:69–74
Whittingham T (2005) Contrast-specific imaging techniques: technical perspective. In: Quaia E (ed). Contrast media in ultrasonography: basic principles and clinical applications. Berlin, Heidelberg, New York: Springer, pp 43–70
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quaia, E., Bartolotta, T.V., Midiri, M. et al. Analysis of different contrast enhancement patterns after microbubble-based contrast agent injection in liver hemangiomas with atypical appearance on baseline scan. Abdom Imaging 31, 59–64 (2006). https://doi.org/10.1007/s00261-005-0358-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-005-0358-9