Abstract
Background
We measured myocardial blood flow (MBF) and myocardial perfusion reserve (MPR) by a dynamic low-dose CZT-SPECT protocol in patients with suspected or known coronary artery disease (CAD) and investigated the capability of dynamic data in predicting obstructive CAD. A total of 173 patients with suspected or known CAD underwent dynamic CZT-SPECT after the injection of 155 MBq and 370 MBq of 99mTc-sestamibi for rest and stress imaging, respectively. Standard rest and stress imaging were performed at the end of each dynamic scan. A total perfusion defect (TPD) < 5% were considered normal. Obstructive CAD was defined as ≥ 70% stenosis at coronary angiography.
Results
Global MPR was lower (p < 0.05) in patients with abnormal compared with those with normal MPI (2.40 ± 0.7 vs. 2.70 ± 0.8). A weak, albeit significant correlation between TPD and MPR (r = − 0.179, p < 0.05) was found. In 91 patients with available angiographic data, hyperemic MBF (2.59 ± 1.2 vs. 3.24 ± 1.1 ml/min/g) and MPR (1.96 ± 0.7 vs. 2.74 ± 0.9) were lower (both p < 0.05) in patients with obstructive CAD (n = 21) compared with those without (n = 70). At univariable analysis, TPD, hyperemic MBF, and MPR were significant predictors of obstructive CAD, whereas only MPR was independent predictor at multivariable analysis (p < 0.05). At per vessels analysis, regional hyperemic MBF (2.59 ± 1.2 vs. 3.24 ± 1.1 ml/min/g) and regional MPR (1.96 ± 0.7 vs. 2.74 ± 0.9) were lower in the 31 vessels with obstructive CAD compared with 242 vessels without (both p < 0.05).
Conclusions
In patients with suspected or known CAD, MPR assessed by low-dose dynamic CZT-SPECT showed a good correlation with myocardial perfusion imaging findings and it could be useful to predict obstructive CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) represents the most widely used non-invasive cardiac imaging tool for diagnosis and risk stratification of patients with suspected or known coronary artery disease (CAD) [1,2,3]. Despite the presence of stress-induced myocardial ischemia at visual or semi-quantitative MPI analysis correlates with the occurrence of obstructive CAD, in patients with multivessel disease, the balanced hypoperfusion may affect the diagnostic accuracy, leading to an underestimation of the defect extent [4]. Quantitative assessment of myocardial perfusion reserve (MPR) by cardiac positron emission tomography (PET) has been largely used to evaluate the severity and the extent of CAD [5], providing incremental diagnostic and prognostic information over the perfusion findings [6, 7].
Recently, novel dedicated gamma cameras with semiconductor cadmium-zinc-telluride (CZT) detectors have been introduced in the clinical practice for cardiac imaging [8]. These new cameras, characterized by improved spatial, temporal, and energy resolution as compared with conventional cameras, allow to perform dynamic data by list-mode acquisition, adding to the standard perfusion evaluation the possibility to estimate myocardial blood flow (MBF) and MPR by SPECT imaging [9, 10]. It has been demonstrated that MPR, assessed by dynamic SPECT MPI, is reduced in relation to the extent and severity of the perfusion defects in patients with obstructive CAD [9, 11]. Moreover, the characteristics of CZT cameras, the heart-oriented geometry and higher energy resolution, are expected also to reduce the administrated dose without affecting image quality. Therefore, the aim of the present study was to measure MBF and MPR by a dynamic low-dose CZT-SPECT protocol in a cohort of patients with suspected or known CAD and to investigate the capability of dynamic data in predicting obstructive CAD.
Materials and methods
Study population
We studied 173 consecutive patients with suspected or known CAD, submitted by referring physicians to stress MPI for the assessment of myocardial ischemia. Within 90 days after MPI, 91 (52%) patients underwent coronary angiography. The decision to send patients to angiography was made by the referring physicians, not aware of the MPR and MBF results. Patient clinical history was collected, and cardiac risk factors were assessed before nuclear testing. Hypertension was defined as a blood pressure ≥ 140/90 mmHg or the use of anti-hypertensive medication. Hypercholesterolemia was defined as total cholesterol level > 6.2 mmol/L or treatment with cholesterol lowering medication. Patients were classified as having diabetes if they were receiving treatment with oral hypoglycemic drugs or insulin. A positive family history of CAD was defined by the presence of disease in first-degree relatives younger than 55 years in men or 65 years in women. Patients with previous myocardial infarction (n = 72) and or prior revascularization procedures (n = 84) were considered as having known CAD. The review committee of our institution approved this study and all patients gave informed consent (“Comitato Etico, Università Federico II,” protocol number 110/17).
SPECT imaging
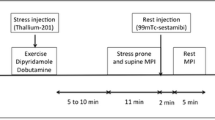
All patients performed a 1-day rest-stress protocol (Fig. 1). Patients were instructed not to consume products containing caffeine for 24 h before the test. MPI was performed in upright position using a dedicated cardiac CZT camera (D-SPECT, Spectrum Dynamics, Caesarea, Israel). A dose of 37 MBq of 99mTc-sestamibi was administered for a 60-s pre-scan acquisition to check patient position, to identify the location of the heart and to set the angle limits of scanning for each detector (region of interest-centric scanning). For rest dynamic images, an intravenous bolus administration of 155 MBq of 99mTc-sestamibi at rate of 1–2 cm3/s using an automatic injector system (Empower CTA, Bracco Imaging Italia, Milano, Italy) and flushed by 30 mL of saline to ensure consistent delivery of a tight bolus. From the injection time, a list-mode acquisition of 6 min started. Standard rest perfusion images were acquired at the end of rest dynamic scan; the time per projection was set to target the recording of 1000 myocardial kcounts allowing a duration of the scans of less than 10 min. Thereafter, pharmacologic stress test using dipyridamole was started. Dipyridamole was infused at dose of 0.56 mg/kg intravenously over a 4-min period (142 mcg/kg/min). All along the infusion, monitoring of heart rate and rhythm, blood pressure, and electrocardiography were performed. Four minutes after completion of dipyridamole infusion, a second bolus of 370 MBq of 99mTc-sestamibi was injected for dynamic stress acquisition followed by a list-mode acquisition of 6 min and by a subsequent stress gated acquisition of 4 min. At the end of the dynamic stress acquisition, a dose of 100 mg of aminophylline was administered intravenously in the event of chest pain or other symptoms, or after significant ST depression. List-mode data were re-binned into 32 frames consisting of 21 × 3-s, 1 × 9-s, 1 × 15-s, 1 × 21-s, 1 × 27-s, and 7 × 30-s frames [10]. Summed and gated projections were reconstructed with an iterative maximum likelihood expectation maximization algorithm using 7 and 4 iterations, respectively.
CZT-SPECT imaging protocol. An initial dose of approximately 37 MBq is administered in order to position (Pos) the patient’s heart within the field of view using a 60-s pre-scan acquisition. A dose of 155 MBq is then injected to the patient as a bolus with a dynamic list-mode images acquisition. After a delay of 25 min, a rest gated perfusion scan is acquired. After controlling the correct position (Pos) of the heart a dipyridamole infusion was started. A second bolus of tracers was injected for dynamic stress by a list-mode acquisition of 6 min with a subsequent stress gated acquisition of 4 min.
Imaging interpretation
An automated software program (e-soft, 2.5, QGS/QPS, Cedars- Sinai Medical Center, Los Angeles, CA, USA) was used to calculate left ventricular (LV) volumes and ejection fraction and the scores incorporating both the extent and severity of perfusion defects, using a standardized segmentation of 17 myocardial regions [12]. The total perfusion defect (TPD) of the stress images was also generated, representing the defect extent and severity and expressed as a percentage of the LV myocardium [13]. In presence of a TPD < 5%, MPI was considered normal [14].
MBF quantification
Dynamic imaging data and corresponding perfusion information were analyzed using commercially available Corridor 4DM software (v2015, INVIA, Ann Arbor, MI, USA).
The summed myocardial images obtained beyond 2 min in the list-mode acquisition, and a midwall surface was used and divided in 460 polar map sectors. LV myocardial tissue time activity curves (TAC) were sampled across all time frames at the center of each polar map sector of the midwall surface. From the polar map TACs, global and regional TACs were averaged. The MPR analysis makes use of ROI blood sampling by averaging a region in the LV blood pool, specifically in the center of the LV in the short axis (ROI size, 2 pixels) and centered at the basal valve plane along the long-axis (ROI length, 30 mm long), across all time frames. The input function region was verified for each patient and adjusted if needed. Motion correction was manually performed for each frame when appropriate. A net retention model [15, 16] was used to calculate the retention rate (R) [10].
Coronary angiography
Coronary angiography was performed using the standard Judkins method. Experienced cardiologists visually interpreted all coronary angiograms. Presence of luminal diameter stenosis ≥ 70% in at least one of the major vascular territories was considered as obstructive CAD [17, 18].
Statistical analysis
Continuous data are expressed as mean ± SD and categorical data as percentage. Unpaired two-sample t test and chi-square test were used to compare differences in continuous and categorical variables, respectively. A p value < 0.05 (two-sided) was considered statistically significant. Correlations between TPD and stress MBF and global MPR by D-SPECT have been evaluated by Pearson’s coefficient. Univariable and multivariable logistic regression analyses were used to evaluate the ability of MPR in predicting obstructive CAD. The variables resulted significant at univariate analysis, were introduced into multivariate model. Receiver operating characteristic (ROC) areas under the curve (AUC) were used to evaluate the ability of relevant predictors to identify obstructive CAD and to identify the best trade-off between sensitivity and specificity for different regional MPR cutoff points [19]. Statistical analysis was performed with Stata 15.1 software (StataCorp, College Station, Texas, USA).
Results
Characteristics of the patients are summarized in Table 1. Of the overall 173 patients, 83 (48%) had normal and 90 (52%) abnormal MPI. Hyperemic MBF was significantly lower in patients with abnormal compared with those with normal MPI (2.90 ± 1.2 vs. 3.54 ± 1.1 ml/min/g, p < 0.01). Similarly, MPR was significantly lower in patients with abnormal compared with those with normal MPI (2.40 ± 0.7 vs. 2.70 ± 0.8, respectively, p < 0.05). Moreover, a weak albeit significant inverse correlation between TPD and hyperemic MBF (r = − 0.43, p < 0.01) and MPR (r = − 0.18, p < 0.05) was found (Fig. 2).
Predictors of CAD
Among 91 patients with available coronary angiographic data, 21 (23%) had obstructive CAD. Of these latter patients, 13 (62%) had single-vessel disease, 6 (29%) two-vessel disease, and 2 (9%) three-vessel disease. At coronary angiography, all patients with prior revascularization showed no flow-limiting coronary stenosis in the corresponding treated vessels. The response to pharmacologic stress test, MPI findings, and dynamic data in patients with and without obstructive CAD are reported in Table 2. A significant response to pharmacologic stress test was observed in both groups of patients. Patients with obstructive CAD had higher TPD and post-stress end-diastolic volume compared with patients without CAD. Patients with obstructive CAD also had lower hyperemic MBF and MPR (both p < 0.01) compared with patients without CAD. At univariate logistic regression analysis, TPD (p < 0.05), hyperemic MBF (p < 0.01), and MPR (p < 0.01) resulted significant predictors of obstructive CAD. At multivariate analysis, only MPR resulted significant predictor of obstructive CAD (p < 0.01) (Table 3). At ROC analysis, the AUC for the identification of obstructive CAD were 0.61 (95% confidence interval, CI, 0.46–0.75) for TPD, 0.68 (95% CI 0.57–0.80) for hyperemic MBF, and 0.70 (95% CI 0.57–0.83) for MPR (p = 0.60). A MPR value of 2.6 provided the best trade-off between sensitivity and specificity for identifying obstructive CAD (Fig. 3). Using this cutoff value, sensitivity and specificity for CAD detection were 86% (95% CI 0.64–0.97) and 50% (95% CI 0.38–0.62).
Per-vessel analysis
In the 91 patients with available coronary angiographic data, 273 individual vessels were analyzed, and obstructive CAD was observed in 31 (11%) vessels (Table 4). During stress-induced hyperemia, baseline MBF increased significantly (p < 0.001) in both vessels with and without obstructive CAD. Vessels with obstructive CAD had lower regional hyperemic MBF (both p < 0.01) and regional MPR (p < 0.001) (Fig. 4). At multivariable analysis, only regional MPR resulted independent predictor of obstructive CAD (odds ratio 0.30, 95% CI 0.15–0.58, p < 0.001). The AUC at ROC analysis for hyperemic MBF and MPR for the identification of obstructive CAD were 0.64 (95% CI 0.54–0.74) and 0.76 (95% CI 0.66–0.86), respectively. A regional MPR of 2.1 provided the best trade-off between sensitivity and specificity for identifying obstructive CAD (Fig. 5). Using this cutoff point, sensitivity and specificity for obstructive CAD detection was 65% (95% CI 0.45–0.81) and 83% (95% CI 0.77–0.87).
Discussion
The results of this study demonstrated that in patients with suspected or known CAD, there was a relationship between MPI findings and both hyperemic MBF and MPR obtained by CZT-SPECT. Yet, global MPR resulted independent predictor of CAD and regional MPR was useful for the identification of obstructive CAD in the corresponding coronary artery.
MPI is a robust and widely used imaging tool in the diagnostic and prognostic evaluation of patients with known or suspected CAD [1,2,3]. Different studies outlined the incremental value of measurements of coronary flow reserve in different categories of patients for both diagnostic and prognostic purposes [20]. Quantitative measurements of coronary vascular function can improve the diagnostic accuracy of MPI [6, 21]. In particular, patients with severe multivessel disease, where a normal MPI result does not necessarily identify truly low-risk subgroups among high-risk cohorts, usually show a reduced MPR [20, 22]. The presence of a normal MPR by PET imaging is associated with a high negative predictive value for high-risk CAD [22]. On the other hand, the addition of an abnormal MPR to other high-risk findings on stress testing may improve the identification of patients with high-risk CAD on angiography [21]. With the introduction of new solid-state dedicated cardiac camera with CZT detectors, it may be feasible to obtain a quantification of regional and global myocardial perfusion and perfusion reserve [9, 10, 23]. Ben-Haim et al. [9] in 95 patients with suspected or known stable CAD showed that CZT-SPECT assessed MPR is lower in patients with myocardial perfusion defects. In a small subgroup of 16 patients with available angiographic data, MPR showed a stepwise decrease with increasing extent of obstructive CAD on angiography. Global MPR correlated inversely with the extent of obstructive CAD on coronary angiography and regional MPR was lower in territories supplied by coronary arteries with at least 50% stenosis than in those with non-obstructive disease [9]. More recent data from Agostini et al. [10] showed that dynamic CZT-SPECT (using an injected dose for rest-stress imaging of 3 MBq/kg and 9 MBq/kg, respectively) provide similar MPR compared with 15O-water PET imaging with high diagnostic value in detecting abnormal fractional flow reserve in 30 patients with stable CAD.
In the present investigation, the prevalence of abnormal perfusion was 67% in patients with obstructive CAD and 56% in those without. The high rate of abnormal perfusion in patients without obstructive CAD is likely due to the presence of 38 subjects with known CAD (prior myocardial infarction and/or coronary revascularization). We found an inverse relationship between myocardial perfusion parameters obtained by CZT-SPECT and both hyperemic MBF and MPR, with lower values of MBF and MPR in regions with abnormal MPI as compared with those with normal findings.
A low-dose stress MPI protocol by CZT camera provides a high diagnostic performance and a dramatic reduction in patient radiation doses [24]. Tracer activity may be reduced using CZT-SPECT, resulting in a radiation dose exposure of 2–3 mSv for a complete rest and stress study, placing nuclear MPI at the same level with PET and even below diagnostic invasive angiography [25, 26]. Our results suggest that MPR by dynamic CZT-SPECT, with a tracer dose lower than previous studies, is useful in predicting the presence of obstructive CAD. According to recent published data, a further dose decrease could be hypothesized [27]. This aspect outlined the important role of CZT camera in reducing dose administration in an era where dose-saving strategies enable nuclear MPI to be more cost-effective [26]. Interestingly, in our study, we observed lower values of both hyperemic MBF and MPR in vessels with obstructive CAD. MPR also resulted as independent predictor of the presence of obstructive CAD. In a per-vessel analysis, a threshold of 2 has been identified in the detection of obstructive CAD in corresponding lesions with a good diagnostic performance using this cutoff value. These results are in agreement with recent findings analyzing coronary artery territories with a cutoff value < 2.1 by CZT-SPECT and showing a sensitivity and specificity of 58% and 85%, respectively, in identifying a fractional flow reserve ≤ 0.8. [10]. It has also been demonstrated that a regional MPR cutoff point of 2.2 provides a sensitivity of 63% and 74% for the identification of obstructive CAD in the corresponding artery [11]. Our results obtained in a larger patient population and using a lower injected dose are in agreement with these published data. Despite significantly lower MPR for vessels with obstructive CAD compared with those without, there was a wide margin of error including data approaching 1 or below 1 in the non-obstructive CAD group. This finding could be explained by the presence of few vessels (3%) without obstructive CAD and reduced MPR in some patients with prior myocardial infarction, coronary artery stenosis < 70%, and multiple risk factors.
Study limitations
This study has some limitations. First, coronary vascular function is influenced by other factors then major coronary artery anatomy, such as microvascular disease. In addition, 99mTc-labeled tracers are not ideal flow agents, and their myocardial uptake is low at high flow rates. Even so, this new SPECT technology offers the opportunity for high-resolution myocardial perfusion imaging joined with dynamic imaging. With the increasing availability of dedicated cardiac cameras with solid-state detectors, this technology offers great promise for MBF and CFR quantification with dynamic SPECT. Future studies will clarify the effectiveness of dynamic SPECT flow imaging [28].
Conclusion
In patients with suspected or known CAD, MPR assessed by low-dose dynamic 1-day rest-stress CZT-SPECT weakly correlates with myocardial perfusion findings and is an independent predictor of obstructive CAD. A regional MPR cutoff point of 2.1 is useful for the identification of obstructive CAD in the corresponding artery.
References
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/ SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging. J Am Coll Cardiol. 2009;53:2201–29.
Green R, Cantoni V, Petretta M, Acampa W, Panico M, Buongiorno P, et al. Negative predictive value of stress myocardial perfusion imaging and coronary computed tomography angiography: a meta-analysis. J Nucl Cardiol. 2018;25:1588–97.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–85.
Berman DS, Kang X, Slomka PJ, Gerlach J, de Yang L, Hayes SW, et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol. 2007;14:521–8.
Bybee KA, Lee J, Markiewicz R, Longmore R, McGhie AI, O’Keefe JH, et al. Diagnostic and clinical benefit of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial perfusion stress imaging. J Nucl Cardiol. 2010;17:188–96.
Zampella E, Acampa W, Assante R, Nappi C, Gaudieri V, Mainolfi CG, et al. Combined evaluation of regional coronary artery calcium and myocardial perfusion by (82)Rb PET/CT in the identification of obstructive coronary artery disease. Eur J Nucl Med Mol Imaging. 2018;45:521–9.
Assante R, Acampa W, Zampella E, Arumugam P, Nappi C, Gaudieri V, et al. Prognostic value of atherosclerotic burden and coronary vascular function in patients with suspected coronary artery disease. Eur J Nucl Med Mol Imaging. 2017;44:2290–8.
Esteves FP, Raggi P, Folks RD, Keidar Z, Askew JW, Rispler S, et al. Novel solid-state-detector dedicated cardiac camera for fast myocardial perfusion imaging: multicenter comparison with standard dual detector cameras. J Nucl Cardiol. 2009;16:927–34.
Ben-Haim S, Murthy VL, Breault C, Allie R, Sitek A, Roth N, et al. Quantification of myocardial perfusion reserve using dynamic SPECT imaging in humans: a feasibility study. J Nucl Med. 2013;54:873–9.
Agostini D, Roule V, Nganoa C, Roth N, Baavour R, Parienti JJ, et al. First validation of myocardial flow reserve assessed by dynamic (99m)Tc-sestamibi CZT-SPECT camera: head to head comparison with (15)O-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging. 2018;45:1079–90.
de Souza ACDAH, Gonçalves BKD, Tedeschi AL, Lima RSL. Quantification of myocardial flow reserve using a gamma camera with solid-state cadmium-zinc-telluride detectors: relation to angiographic coronary artery disease. J Nucl Cardiol. 2019. https://doi.org/10.1007/s12350-019-01775-z.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42 Review.
Slomka PJ, Nishina H, Berman DS, Akincioglu C, Abidov A, Friedman JD, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol. 2005;12:66–77.
Nakazato R, Tamarappoo BK, Kang X, Wolak A, Kite F, Hayes SW, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: correlation with invasive coronary angiography. J Nucl Med. 2010;51:1724–31.
Leppo JA, Meerdink DJ. Comparison of the myocardial uptake of a technetium-labeled isonitrile analogue and thallium. Circ Res. 1989;65:632–9.
Yoshida K, Mullani N, Gould KL. Coronary flow and flow reserve by PET simplified for clinical applications using rubidium-82 or nitrogen-13-ammonia. J Nucl Med. 1996;37:1701–12.
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64:1929–49.
Petretta M, Acampa W, Daniele S, Petretta MP, Nappi C, Assante R, et al. Transient ischemic dilation in SPECT myocardial perfusion imaging for prediction of severe coronary artery disease in diabetic patients. J Nucl Cardiol. 2013;20:45–52.
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. 2008;50:419–30.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124:2215–24
Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, et al. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med. 2014;55:248–55.
Ben Bouallègue F, Roubille F, Lattuca B, Cung TT, Macia JC, Gervasoni R, et al. SPECT myocardial perfusion reserve in patients with multivessel coronary disease: correlation with angiographic findings and invasive fractional flow reserve measurements. J Nucl Med. 2015;56:1712–7.
Giubbini R, Bertoli M, Durmo R, Bonacina M, Peli A, Faggiano I, et al. Comparison between N(13)NH(3)-PET and (99m)Tc-Tetrofosmin-CZT SPECT in the evaluation of absolute myocardial blood flow and flow reserve. J Nucl Cardiol. 2019. https://doi.org/10.1007/s12350-019-01939-x.
Perrin M, Djaballah W, Moulin F, Claudin M, Veran N, Imbert L, et al. Stress-first protocol for myocardial perfusion SPECT imaging with semiconductor cameras: high diagnostic performances with significant reduction in patient radiation doses. Eur J Nucl Med Mol Imaging. 2015;42:1004–11.
Einstein AJ, Johnson LL, DeLuca AJ, Kontak AC, Groves DW, Stant J, et al. Radiation dose and prognosis of ultra-low-dose stress-first myocardial perfusion SPECT in patients with chest pain using a high-efficiency camera. J Nucl Med. 2015;56:545–51.
Acampa W, Buechel RR, Gimelli A. Low dose in nuclear cardiology: state of the art in the era of new cadmium-zinc-telluride cameras. Eur Heart J Cardiovasc Imaging. 2016;17:591–5.
Nkoulou R, Fuchs T, Pazhenkottil AP, Wolfrum M, Buechel R, Gaemperli O, et al. High efficiency gamma camera enables ultra-low fixed dose stress/rest myocardial perfusion imaging. Eur Heart J Cardiovasc Imaging. 2019;20:218–24.
Petretta M, Storto G, Pellegrino T, Bonaduce D, Cuocolo A. Quantitative assessment of myocardial blood flow with SPECT. Prog Cardiovasc Dis. 2015;57:607–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wanda Acampa and Roberta Assante shared first co-authorship.
This article is part of the Topical Collection on Cardiology
Rights and permissions
About this article
Cite this article
Acampa, W., Assante, R., Mannarino, T. et al. Low-dose dynamic myocardial perfusion imaging by CZT-SPECT in the identification of obstructive coronary artery disease. Eur J Nucl Med Mol Imaging 47, 1705–1712 (2020). https://doi.org/10.1007/s00259-019-04644-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04644-6