Abstract
Purpose
To evaluate the prognostic value of coronary atherosclerotic burden, assessed by coronary artery calcium (CAC) score, and coronary vascular function, assessed by coronary flow reserve (CFR) in patients with suspected coronary artery disease (CAD).
Methods
We studied 436 patients undergoing hybrid 82Rb positron emission tomography/computed tomography imaging. CAC score was measured according to the Agatston method, and patients were categorized into three groups (0, <400, and ≥400). CFR was calculated as the ratio of hyperemic to baseline myocardial blood flow, and it was considered reduced when <2.
Results
Follow-up was 94% complete during a mean period of 47±15 months. During follow-up, 17 events occurred (4% cumulative event rate). Event-free survival decreased with worsening of CAC score category (p < 0.001) and in patients with reduced CFR (p < 0.005). At multivariable analysis, CAC score ≥400 (p < 0.01) and CFR (p < 0.005) were independent predictors of events. Including CFR in the prognostic model, continuous net reclassification improvement was 0.51 (0.14 in patients with events and 0.37 in those without). At classification and regression tree analysis, the initial split was on CAC score. For patients with a CAC score < 400, no further split was performed, while patients with a CAC score ≥400 were further stratified by CFR values. Decision curve analyses indicate that the model including CFR resulted in a higher net benefit across a wide range of decision threshold probabilities.
Conclusions
In patients with suspected CAD, CFR provides significant incremental risk stratification over established cardiac risk factors and CAC score for prediction of adverse cardiac events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Noninvasive diagnosis of coronary artery disease (CAD) and risk assessment represent major challenges for clinical decision-making and appropriate management in patients with suspected CAD [1]. Coronary artery calcium (CAC) score evaluation has played a significant role in clinical management of patients with suspected CAD [2]. In particular, CAC scoring is considered a powerful tool in risk-stratifying asymptomatic patients at intermediate risk of CAD [3]. It has also been demonstrated that not only the presence but also the extent of coronary calcification significantly improves the prediction of cardiovascular events, in addition to traditional cardiovascular risk factors [4]. Myocardial perfusion imaging (MPI) with positron emission tomography (PET)/computed tomography (CT) allows absolute quantification of myocardial blood flow (MBF) and coronary flow reserve (CFR) with a feasible possibility to perform CAC quantification as a part of the same examination [5]. Previous studies demonstrated that the presence of abnormal CFR, reflecting both the presence of epicardial coronary artery stenosis and microvascular dysfunction, is associated with a higher cardiac event rate in patients with suspected and known CAD [6,7,8]. Recently, some studies evaluated the combined role of structural and functional information obtained by PET/CT [9, 10]. In particular, a significant inverse relationship between extent of CAC and CFR by 82Rb PET/CT has been reported in patients with suspected CAD [10]. However, only few data are available that combine measures of structural abnormalities and coronary vasodilator function in predicting adverse cardiac events in patients without overt CAD. The aim of this study was to evaluate the long-term prognostic value of CAC scoring and coronary vascular function by hybrid 82Rb PET/CT imaging in a cohort of patients with low-intermediate risk of CAD.
Materials and methods
Study population
This prospective study comprised 436 subjects with low-intermediate risk of CAD referred to CAC scoring and MBF measurements by PET/CT for atypical chest pain. For each patient the presence of coronary risk factors was noted. Hypertension was defined as a blood pressure ≥140/90 mmHg or the use of anti-hypertensive medication [11]. Hypercholesterolemia was defined as total cholesterol level >6.2 mmol/L or treatment with cholesterol lowering medication. Patients were classified as having diabetes if they were receiving treatment with oral hypoglycemic drugs or insulin. A positive family history of CAD was defined by the presence of disease in first-degree relatives younger than 55 years in men or 65 years in women. Exclusion criteria were documented history of CAD defined as previous percutaneous coronary intervention, coronary artery bypass graft surgery, or myocardial infarction. Patients with uncontrolled atrial fibrillation, pacemaker, or prosthetic valve were also excluded. The ethics committee of our institution approved the study and all patients gave informed consent.
PET imaging
As a routine preparation for 82Rb cardiac PET/CT, patients were asked to discontinue taking nitrates for 6 h, calcium channel blockers and caffeine-containing beverages for 24 h, and beta-blockers for 48 h before their appointment. Scans were acquired using a Biograph mCT 64-slice scanner (Siemens Healthcare). Rest and stress cardiac PET/CT images were acquired as follows: scout CT to check the patient position and low-dose CT (0.4 mSv; 120 kVp; effective tube current, 26 mA [11-mAs quality reference]; 3.3 s) were performed for attenuation correction, during normal breathing before and after PET acquisitions. For both rest and stress images 1110 MBq of 82Rb were injected intravenously and a 6-min list-mode PET study was acquired. Pharmacologic stress was then administered using adenosine (140 μg × kg−1 × min−1 for 4.5 min). Both rest and stress dynamic images were reconstructed into 26 time frames (12 × 5 s, 6 × 10 s, 4 × 20 s, and 4 × 40 s; total, 6 min) using the vendor standard ordered subsets expectation maximization 3D reconstruction (2 iterations, 24 subsets) with a 6.5-mm Gaussian post-processing filter. Regional myocardial perfusion was visually assessed, using standardized segmentation of 17 myocardial regions [12]. Each myocardial segment was scored from normal (score = 0) to absent perfusion (score = 4). The summed stress score was obtained by adding the scores of the 17 segments of the stress images. A similar procedure was applied to the resting images to calculate the summed rest score and summed difference score was the difference between the stress and rest scores. Myocardial perfusion was considered abnormal when the summed stress score was ≥3. Subjects with summed difference score ≥2 were defined as having stress-induced myocardial ischemia (2–6 mild ischemia and >6 moderate-severe ischemia). Absolute MBF (in mL × min−1 × g−1) was computed from the dynamic rest and stress imaging series with commercially available software (Siemens Syngo Dynamic PET) [13]. CFR was defined as the ratio of hyperemic to baseline MBF and was considered reduced when <2 [14].
CT imaging
All patients underwent a CT scan for CAC scoring. Those with heart rate >75 bpm received prior intravenous beta-blockers (5–10 mg atenolol). A standard scanning protocol was applied, with 18-mm section collimation (30 9 0.6 mm), 0.24 ms gantry rotation time, 120 kVp tube voltage, and 60 Q ref. mAs tube current. CAC scoring was obtained during a single breath hold and coronary calcification was defined as a plaque with an area of 1.03 mm2 and a density ≥130 HU. The CAC score was calculated according to the method described by Agatston [15]. Experienced nuclear medicine physicians analyzed the CT, blinded to the PET results (Siemens, Syngo Multimodality Workplace). CAC scores were calculated separately for left anterior descending, left circumflex, and right coronary arteries and summed to provide a total CAC score. The CAC score was also categorized into three groups (0- <400, and ≥400).
Follow-up data
Patient follow-up was prospectively obtained by use of a questionnaire that was assessed by a phone call to all patients and general practitioners or cardiologists and by review of hospital or physicians’ records by individuals blinded to the patient’s test results. The outcome was a composite end-point of cardiac death, nonfatal myocardial infarction, or unstable angina requiring coronary revascularization, whichever occurred first. The cause of death was confirmed by review of death certificate, hospital chart, or physician’s records. Death was considered to be of cardiac origin if the primary cause was defined as acute myocardial infarction, congestive heart failure, valvular heart disease, sudden cardiac death, or cardiac interventional/surgical procedure related. Myocardial infarction was defined when >2 of the following 3 criteria were met: chest pain or equivalent symptom complex, positive cardiac biomarkers, or typical electrocardiographic changes [16]. The date of the last examination or consultation was used to determine the length of follow-up.
Statistical analysis
Continuous data are expressed as means ± SD and categorical data as percentage. Comparison between groups was performed with unpaired t test or chi-square test, as appropriate. A p value <0.05 was considered statistically significant. The ln(CAC + 1) score transformation was used to adjust for the rightward skew of the data and to reduce heteroscedasticity. Annualized event rates, expressed as % person-years, were calculated as the cumulative number of events divided by person-time. This latter is an estimate of the actual time-at risk that all persons contribute to the study, i.e., the sum of each individual follow-up period. Event-free survival curves were obtained by the Kaplan-Meier method and compared with the log-rank test. Hazard ratios with 95% confidence intervals (CI) were calculated by univariable and multivariable Cox regression analysis. Variables showing a p value <0.05 at univariable analysis were considered for multivariable analysis. The incremental prognostic value of clinical data and imaging findings was assessed considering variables in hierarchical order. For this purpose, we considered three nested models: a model including only clinical variables (model 1), a model including clinical variables and CAC score (model 2), and a model including clinical variables, CAC score, and CFR (model 3). Cox models of different complexity were compared using the log likelihood statistics [17]. The added prognostic value of CFR for predicting study outcomes beyond and above clinical variables and CAC score was investigated using Harrell’s C index (a measure of discrimination) and compared using Somers’ D test [18]. Classification and regression tree (CART) analysis was performed using the CART Stata package for failure time data [19]. This program uses the martingale residuals of the Cox model including clinical variables, CAC score, and CFR to calculate chi-square values for all possible cut-points of the covariates. A tree was generated allowing the CART program to determine the variable with the optimal first split. The ability of CFR in patients’ reclassification was evaluated by continuous net reclassification index (cNRI), and absolute and relative integrated discrimination improvement (IDI) for survival data [20,21,22]. The basic idea behind the NRI and IDI is that a valuable marker will tend to increase predicted risks for patients with events and decrease predicted risks for patients without such events. Finally, the added value of CFR was also evaluated comparing the net benefit curves obtained by decision curve analysis [23] using model 2 and model 3. The net benefit is calculated as true-positive rate − false-positive rate × weighting factor. Specifically, the false-positive rate is multiplied by the ratio of the threshold probability divided by 1 − the threshold probability. Statistical analysis was performed with STATA 15.0 for Windows (StataCorp LP, College Station, TX).
Results
Patient characteristics and outcome
Of the 436 patients enrolled, follow-up data were not available in 26 patients (6%), leaving 410 subjects available for the analysis. The median follow-up was 50 months (range 5–72) for overall study population, 50 months (range 12–72) for censored subjects and 29 months (range 5–56) for patients with events. During follow-up, 17 events occurred (4% cumulative event rate, with an annual event rate of 0.087% person-years). The events were cardiac death in three patients, nonfatal myocardial infarction in three, and unstable angina requiring revascularization in 11. Clinical characteristics of patients with and without events are reported in Table 1. Patients who experienced an event were older and had a higher prevalence of hypertension and hypercholesterolaemia and had higher body mass index values than patients without an event.
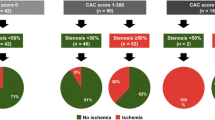
Imaging findings of patients with and without events are reported in Table 2. Patients with an event showed a higher ln(CAC + 1) than those without. Myocardial perfusion was normal in 369 (90%) patients, while 41 (10%) patients had stress-induced mild ischemia. The prevalence of abnormal perfusion was higher in patients with events as compared to those without. Patients with an event showed lower hyperemic MBF and CFR values compared to patients without an event, while there were no differences in baseline MBF between the two groups. Moreover, patients with an event had a lower prevalence of CAC score 0 and a higher prevalence of CAC ≥400 than patients without events. On the contrary, the prevalence of CAC score <400 was not significantly different between the two groups. Event rates according to CAC score and CFR categories are illustrated in Fig. 1. As shown, the annualized event rate significantly increased with increasing of CAC score categories (p for trend <0.001), and it was higher in patients with reduced CFR (p < 0.001).
Predictors of events
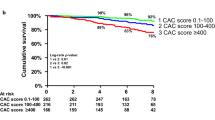
Univariable and multivariable Cox regression analyses are reported in Table 3. Age, diabetes, hypertension, hypercholesterolaemia, CAC score, stress-induced ischemia, and CFR were univariable predictors of events, while at multivariable analysis only CAC score and CFR were independent predictors. The event-free survival curves according to CAC score categories and CFR are reported in Fig. 2. As illustrated, event-free survival decreased with worsening of CAC score category and in patients with reduced CFR (both p < 0.001). At incremental analysis, CAC score added prognostic information to model 1 increasing the global chi-square from 23.2 to 33.7 (p < 0.005). The addition of CFR to model 2 further increased global chi-square from 33.7 to 42.5 (p < 0.001). Also Harrell’s C significantly increased from 0.86 (95% CI 0.79–0.93) for model 2 to 0.90 (95% CI 0.85–0.95) for model 3 (p < 0.001). The effect of CFR on predicted hazard ratio among CAC categories is depicted in Fig. 3. As shown, the increase in hazard ratio across the different CAC score categories becomes appreciable from CFR value <3.
Patient reclassification
CART analysis produced three terminal groups (Fig. 4) based on CAC score and CFR values, while clinical variables did not add to the CART structure. The initial split was on CAC score, followed by CFR. For patients with CAC score <400 (group 1) no further split was performed, while patients with CAC score ≥400 were further stratified by CFR values ≥2 (group 2) and <2 (group 3). The event rates (% person-years) were 0.49 (95% CI 0.24–1.04) for group 1, 2.66 (95% CI 1.11–6.39) for group 2, and 19.4 (95% CI 11.4–26.8) for group 3 (p for trend <0.001). The event-free survival curves according to CART groups are reported in Fig. 5.
CART analysis considering clinical variables, calcium score, and CFR. The initial split is based on CAC score <400. Patients with CAC score ≥400 are further stratified by CFR values. Patients with CAC score ≥400 and CFR <2 have the highest hazard ratio. Clinical variables did not add to the CART structure. N = number of patients, E = number of events, RHR = relative hazard rate
Including CFR in model 2, cNRI was 0.51 (95% bootstrap CI 0.42–0.61). Specifically, cNRI was 0.14 in patients with and 0.37 in those without events. Such increase in prognostic power was confirmed by absolute (0.10; 95% bootstrap CI 0.03–0.21) and relative (0.69; 95% bootstrap CI 0.23–1.22) IDI.
Decision curve analysis
At decision curve analysis, model 3 was associated with the highest net benefit (Fig. 6) and the largest reduction in false-positive rate without missing any event (Fig. 7) compared to model 2 and to a strategy considering that all patients will experience events for the range of threshold probabilities up to 30%.
Decision curves analysis using model 2 and model 3 for the prediction of cardiac events in patients with suspected CAD. The red line is the net benefit of treating no patients, assuming that all would be alive; the navy line is the net benefit of treating all patients similarly regardless of their severity, assuming that all would die; the green line is the net benefit of treating patients according to model 2; and the orange line is the net benefit of treating patients based on the model 3
Net reduction in false-positive rate at different threshold probability with models 2 and 3 compared with the strategy of considering that all patients will undergo a subsequent event. At a probability threshold of 10%, compared to a strategy assuming that all patients will experience events, the net reduction in false-positive rate is 59 per 100 patients for model 2 and 65 per 100 patients for model 3 without missing any event.
Discussion
Our study first evaluated the interplay between coronary atherosclerotic burden, assessed by CAC score, and coronary vascular function assessed by PET in patients with suspected CAD during a long-term follow-up. From this study it emerged that both the extent of coronary atherosclerotic burden and the presence of coronary vascular dysfunction are associated with increased risk of adverse cardiac events, even after adjustment for cardiovascular risk factors.
The presence of CAC score is indicative of the overall coronary atherosclerotic burden and is a strong predictor of cardiac events as investigated in prior studies. A very low rate of cardiovascular events among patients with CAC score of 0 has been observed [24], while event rate increases progressively according to CAC score. In a large cohort of asymptomatic patients, Budoff et al. [25] demonstrated that increasing plaque burden is associated with increasing risk, supporting evidence of the relationship between CAC extent and all-cause mortality. CAC score also showed the highest improvement in the prediction of event over the others cardiovascular risk marker, suggesting its use as a powerful tool in improving cardiovascular risk prediction in individuals classified as intermediate risk [26].
The use of PET has the potential for absolute quantification of MBF and CFR as markers of coronary vascular function and previous studies have demonstrated the prognostic role of PET-derived CFR in subjects with and without known CAD [8, 27]. In particular, inclusion of CFR in the risk prediction models provided incremental risk stratification beyond clinical and perfusion variables in patients with known or suspected CAD [27, 28].
In patients with suspected CAD, a combined evaluation of CAC score and coronary vascular function could significantly change patient clinical management. Dikic et al. [29], in a cohort of asymptomatic diabetic patients, demonstrated that both CAC score and coronary flow velocity reserve obtained by multi-slice CT and by transthoracic Doppler echocardiography assessments respectively, provide independent and complementary prognostic information. A combined use of the two parameters improved the risk stratification ability and identified patients at higher risk who could benefit from more aggressive treatment.
A principal advantage of hybrid PET/CT is its potential ability to evaluate both the coronary atherosclerotic burden as assessed by CAC score and coronary vascular function as CFR in a same examination. Only few data are available about the use of combined measure of structural abnormalities and coronary vasodilator function by 82Rb PET/CT in predicting adverse cardiac events. In a previous study, Naya et al. [30] in a large cohort of symptomatic patients with suspected CAD, undergoing 82Rb PET/CT followed for a median of 1.53 years, demonstrated that both the extent of coronary calcium deposits and the presence of coronary vascular dysfunction are associated with increased risk of adverse cardiac events. However, after adjustment for clinical risk, only coronary vascular dysfunction improved risk assessment, confirming that total burden of coronary calcium was only modestly associated with impaired vascular function. They concluded that direct measures of coronary vasodilator function might be more powerful marker of cardiac risk than simply the total burden of calcified atherosclerosis.
To the best of our knowledge this is the first study assessing long-term prognostic value of combining measures of structural abnormalities and coronary vasodilator function by 82Rb PET/CT to predict adverse cardiac events in subjects at low-intermediate risk of CAD. We observed a cumulative event rate of 4% in a cohort of patients mostly with (i.e., 90%) normal myocardial perfusion. We found that both CAC score ≥400 and CFR, but not stress-induced ischemia, were independent predictors of cardiac events during a long-term follow-up. In particular, event-free survival decreased with worsening of CAC score categories, and it was worse in patients with reduced CFR. CAC score also added prognostic information to a model including clinical variables. Yet, the addition of CFR further increased the prognostic power of the model. The decision curve is a graphical summary useful to illustrate potential clinical impact of risk models for recommending treatment or intervention. Noteworthy, CFR not only increased the discrimination of a multivariable model including calcium score, but led to an improvement in the decision-curve analysis over a realistic range of threshold probabilities. CART analysis also indicates that a reduced CFR is useful for identify among patients with high CAC score, those at highest risk of subsequent event. Conversely, the increase in hazard ratio across the different CAC score categories becomes apparent only for CFR value <3.
These findings are consistent with previous data demonstrating that direct measures of coronary vasodilator function may be more powerful measures of CAD risk than simply the total burden of calcified atherosclerosis [30]. In particular, it has been shown that for any level of severity of coronary calcification, impaired CFR constantly identified patients at higher short-term risk of adverse cardiac events. Our study might have important clinical implications, suggesting that also during longer follow-up, direct measures of coronary vascular function may help to risk-stratify patients with low-intermediate risk of CAD, in particular those with high level of calcium score.
Conclusions
In patients with suspected CAD, both the extent of coronary calcification and the presence of coronary vascular dysfunction are associated with increased risk of adverse cardiac events, even after adjustment for cardiovascular risk factors. Thus, combined evaluation of functional and structural abnormalities might allow a better risk stratification in patients with low-intermediate risk of CAD. Our results suggest a potential use of CAC scanning for triaging patients at low-intermediate CAD risk for cardiac stress test imaging. More advanced testing should be recommended for risk stratification in patients with a CAC score of ≥400. Conversely, in subjects without coronary calcium there is a very low risk of subsequent cardiac events and advanced imaging tests are not indicated. Finally, in patients with CAC score <400, the need for more advanced imaging tests should be governed by additional information, such as exercise capacity.
References
Berman DS, Hachamovitch R, Shaw LJ, Friedman JD, Hayes SW, Thomson LE, et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: Noninvasive risk stratification and a conceptual framework for the selection of noninvasive imaging tests in patients with known or suspected coronary artery disease. J Nucl Med. 2006;47:1107–18.
Lee H, Yoon YE, Park JB, Kim HL, Park HE, Lee SP, et al. The incremental prognostic value of cardiac computed tomography in comparison with single-photon emission computed tomography in patients with suspected coronary artery disease. PLoS One. 2016;11:e0160188.
Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. American College of Cardiology Foundation, American Heart Association. ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;2010:e50–103.
Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–6.
Bybee KA, Lee J, Markiewicz R, Longmore R, McGhie AI, O'Keefe JH, et al. Diagnostic and clinical benefit of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial perfusion stress imaging. J Nucl Cardiol. 2010;17:188–96.
Daniele S, Nappi C, Acampa W, Storto G, Pellegrino T, Ricci F, et al. Incremental prognostic value of coronary flow reserve assessed with single-photon emission computed tomography. J Nucl Cardiol. 2011;18:612–9.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation. 2015;131:19–27.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150–6.
Danad I, Raijmakers PG, Appelman YE, Harms HJ, de Haan S, Marques KM, et al. Quantitative relationship between coronary artery calcium score and hyperemic myocardial blood flow as assessed by hybrid 15O-water PET/CT imaging in patients evaluated for coronary artery disease. J Nucl Cardiol. 2012;19:256–64.
Assante R, Zampella E, Arumugam P, Acampa W, Imbriaco M, Tout D, et al. Quantitative relationship between coronary artery calcium and myocardial blood flow by hybrid rubidium-82 PET/CT imaging in patients with suspected coronary artery disease. J Nucl Cardiol. 2017;24:494–501.
Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J, Izzo JL Jr, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115:2761–88.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Klein R, Renaud JM, Ziadi MC, Thorn SL, Adler A, Beanlands RS, et al. Intra- and inter-operator repeatability of myocardial blood flow and myocardial flow reserve measurements using rubidium-82 PET and a highly automated analysis program. J Nucl Cardiol. 2010;17:600–16.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356:830–40.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Joint ESC/ACCF/AHA/WHF task force for the universal definition of myocardial infarction. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35.
Vickers AJ, Cronin AM, Begg CB. One statistical test is sufficient for assessing new predictive markers. BMC Med Res Methodol. 2011;11:13.
Newson R. Comparing the predictive powers of survival models using Harrell’s C or Somers’ D. Stata J. 2010;10:339–58.
van Putten W. Classification and regression tree analysis with Stata. http://www.stata.com/meeting/2dutch/cart.pdf.
Pencina MJ, D'Agostino RB Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30:11–21.
Chambless LE, Cummiskey CP, Cui G. Several methods to assess improvement in risk prediction models: extension to survival analysis. Stat Med. 2011;30:22–38.
Uno H, Tian L, Cai T, Kohane IS, Wei LJ. A unified inference procedure for a class of measures to assess improvement in risk prediction systems with survival data. Stat Med. 2013;32:2430–42.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Mak. 2006;26:565–74.
Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA, Kondos GT, et al. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J. 2009;158:554–61.
Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–70.
Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–95.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124:2215–24.
Ziadi MC, Dekemp RA, Williams KA, Guo A, Chow BJ, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol. 2011;58:740–8.
Dikic M, Tesic M, Markovic Z, Giga V, Djordjevic-Dikic A, Stepanovic J, et al. Prognostic value of calcium score and coronary flow velocity reserve in asymptomatic diabetic patients. Cardiovasc Ultrasound. 2015;13:41.
Naya M, Murthy VL, Foster CR, Gaber M, Klein J, Hainer J, et al. Prognostic interplay of coronary artery calcification and underlying vascular dysfunction in patients with suspected coronary artery disease. J Am Coll Cardiol. 2013;61:2098–106.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Assante, R., Acampa, W., Zampella, E. et al. Prognostic value of atherosclerotic burden and coronary vascular function in patients with suspected coronary artery disease. Eur J Nucl Med Mol Imaging 44, 2290–2298 (2017). https://doi.org/10.1007/s00259-017-3800-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3800-7