Abstract
Non-small-cell lung cancer is the most common type of lung cancer and one of the leading causes of cancer-related death worldwide. For this reason, advances in diagnosis and treatment are urgently needed. With the introduction of new, highly innovative hybrid imaging technologies such as PET/CT, staging and therapy response monitoring in lung cancer patients have substantially evolved. In this review, we discuss the role of FDG PET/CT in the management of lung cancer patients and the importance of new emerging imaging technologies and radiotracer developments on the path to personalized medicine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is still the most frequent cancer with an estimated number of cancer-related deaths worldwide of 1.5 million, representing 19 % of all cancer deaths in 2011 [1]. About 80 % of lung cancers are classified as non-small-cell lung cancers (NSCLC) [2] and more than 65 % of these patients present with locally advanced or metastatic disease [3]. The 5-year survival rate in patients with NSCLC is 17 % [4]. The most prevalent histological type of lung cancer in smokers and nonsmokers is adenocarcinoma at 38.5 %, while the prevalence of squamous cell carcinoma is 23.8 % [5]. Until the turn of the century, advanced lung cancer was treated with platinum-based combination therapy, regardless of the underlying histological subtype [6]. Overall survival has since improved to a median survival of 12 months and longer [7] due to the development of new targeted drugs, consideration of different histological subtypes and driver mutations [8]. Multimodal therapy strategies have further decreased morbidity and mortality with adjuvant and neoadjuvant chemotherapy protocols for patients with resectable tumours [9], and the combination of chemotherapy and radiation instead of radiation alone [10].
In patients with NSCLC and epidermal growth factor receptor (EGFR) mutations, the response rate to the EGFR tyrosine kinase inhibitor erlotinib is 58 %, a dramatic improvement over results achieved with chemotherapy [11]. Mutational profiling in Korean patients with adenocarcinoma revealed mutations of EGFR in 60.5 % [12]. Interestingly, genetic modifications such as EGFR mutations and echinoderm microtubule-associated protein-like 4-anaplastic lymphoma kinase (EML4-ALK) rearrangements are more common in patients who have never smoked [6]. Additionally, new imaging strategies such as endoscopic ultrasonography have improved the accuracy of mediastinal staging [13] and the combination of PET and CT has refined the detection rate of distant metastases and therefore lowered the rate of unnecessary thoracotomies [14, 15]. Thus, multimodal imaging constitutes a key element in the process of staging and therapy response assessment of lung cancer, and additionally, in the era of genome-based specific therapies, the role of image-derived biomarkers and novel tracers has become increasingly important.
In this review, we discuss the role of [18F]FDG PET/CT and other advanced imaging technologies such as diffusion-weighted MRI, CT perfusion and hybrid PET/MRI in the management of lung cancer patients. Emerging molecular imaging techniques utilizing novel target-specific radiotracers, which bring us one step closer to personalized medicine, are also described.
FDG PET/CT
Staging
More than 40 % of patients with NSCLC have metastases at the time of presentation [16]. An accurate staging of the disease with confident detection of distant metastases is therefore of the utmost importance for selection of the most effective therapy [6]. Even though most patients are diagnosed initially by chest radiography or low-dose CT, which might become of importance in lung cancer screening [17], FDG PET/CT plays an important role in the staging of lung cancer. While CT provides high anatomic resolution, the CT criteria for abnormal lymph nodes, such as axial short-axis diameter of ≥1 cm, abnormal shape and low attenuation, yield a limited sensitivity (51 – 64 %) and specificity (74 – 86 %) [18]. Although PET has a lower spatial resolution than CT, the metabolic information derived from FDG PET allows more accurate detection of lymph node metastases than CT, with a sensitivity of 85 % and a specificity of 90 % [19].
In agreement with others, Lardinois et al. showed that staging is more accurate with integrated PET/CT than with CT alone, PET alone, or visual correlation of PET and CT [20]. Valuable, additional information can be derived from the radiological appearance and location of the primary tumour on the CT part of PET/CT. For example, an adenocarcinoma may present as a solitary, lobulated or irregular pulmonary mass that can invade the pleura or grow circumferentially around the lungs [21]. Furthermore, squamous cell carcinoma is highly associated with smoking and chronic inflammation, therefore two-thirds of these tumours are located in the central to mid-lung zones [21]. The appearance of these endoluminal lesions is often associated with airway obstruction (postobstructive atelectasis or pneumonia) [5]. Moreover, the maximal standardized uptake value (SUVmax) of FDG in adenocarcinoma with a bronchioloalveolar carcinoma is significantly lower than that of other subtypes of NSCLC [22].
International guidelines for staging and therapy management of lung cancer recommend the PET/CT scan in the routine diagnostic work-up of lung neoplasms. The interdisciplinary guidelines of the German Respiratory Society and the German Cancer Society strongly recommend a whole-body PET/CT scan and head MRI scan in clinical stage IB/IIIB with the intention of curative treatment, even in patients negative on clinical evaluation [23, 24]. The high negative predictive value for distant metastasis has changed the clinical algorithms to proceed towards surgery without further histological verification. Currently, there is a trend to follow up PET-positive mediastinal lesions using new endoscopic ultrasonography techniques and less-invasive mediastinoscopy [6]. Endoscopic ultrasonography (EUS) and endobronchial ultrasonography (EBUS) have high positive predictive values and are therefore the methods of choice for tissue verification with the advantage of real-time biopsy [25].
Response monitoring and prediction of prognosis
Traditional tumour response assessment in lung cancer is based on measurements of changes in tumour size using the conventional Response Evaluation Criteria in Solid Tumors (RECIST). These anatomically based methods have significant limitations in response monitoring and prediction, especially in the case of molecular target therapies. There are numerous clinical trials that have shown promising results for therapy response assessment and evaluation of prognosis using FDG PET/CT. Several studies have demonstrated that a metabolic response on PET (documented as a decrease in SUV) is a significant predictor of histopathological response and survival. In addition, the SUV of the primary tumour has been identified as an independent prognostic factor [26–28]. Recently, Machtay et al. showed that higher posttreatment tumour SUVs (SUVpeak or SUVmax), measured approximately 14 weeks after conventional concurrent platinum-based chemoradiotherapy, are associated with worse survival in stage III NSCLC [29]. Usmanij et al. found that the degree of change in total lesion glycolysis (TLG) is predictive of response to concomitant chemoradiotherapy as early as the end of the second week in patients with locally advanced NSCLC [30].
Early identification of nonresponders could avoid drug side effects and reduce costs associated with unsuccessful therapy. There is some evidence that even after 2 days of erlotinib, assessment of FDG uptake could be useful to identify early resistance in patients [31, 32]. Interestingly, in patients with early-stage NSCLC under neoadjuvant therapy with erlotinib, PET evaluation revealed a metabolic response in 27 %, while CT evaluation using RECIST criteria confirmed a response in only 5 % [33]. Pathological examination following surgery disclosed more than 50 % necrosis in 23 % of these patients and more than 95 % necrosis in 5 % of these patients [34]. These results are in the line with the findings of a current study showing the predictive value of FDG uptake in locally advanced NSCLC, independent of tumour size [34]. In a recently published prospective multicentre study Vera et al. found that assessment of curative-intent radiotherapy or chemoradiotherapy after the 5th week using SUVmax was predictive of disease-free survival after 1 year [35]. The biological basis for the use of FDG uptake for prediction of postsurgical outcome is not yet fully understood. Therefore, Nair et al. analysed FDG uptake and gene expression signatures in NSCLC [36]. They found four single genes (LY6E, RNF149, MCM6, and FAP) that are associated with FDG uptake and survival [36]. In addition, analysis of immunohistochemistry revealed that FDG uptake is significantly associated with glucose transporter 1 (GLUT1), hexokinase I, hypoxia-inducible factor-1 alpha (HIF-1α), vascular endothelial growth factor (VEGF), microvessels (CD34), PI3K/Akt/mTOR signalling pathways (p-Akt, p-mTOR) and EGFR, but PTEN expression showed an inverse correlation [37]. Vesselle et al. described an additional, significant positive correlation between FDG uptake and Ki-67 proliferation index [38]. However, tumour size is still the determining factor in FDG uptake rather than overexpression of GLUT1 and GLUT3 [39].
Due to the small number of enrolled patients in most of the clinical trials using FDG PET for therapy assessment, the explanatory power of most of the studies is limited and more multicentre trials are needed. Moreover, exacerbating the problem of low statistical power, trials that utilize PET systems of different generations are not using protocol-optimized imaging for harmonization of SUV evaluation or other FDG uptake parameters (TLG, metabolic rate of glucose) in order to meet the criteria set out in the European Association of Nuclear Medicine (EANM) guidelines for harmonization of quantitative values [40]. It is essential for future prospective studies of high quality to standardize response criteria, imaging time-points, primary targets (primary tumour or lymph nodes) and clinical endpoints (histology, progression-free survival). Due to the increasing economic constraints on the health-care sector, diagnostic methods such as PET/CT have to show a proven clinical benefit to obtain financial reimbursement. Therefore, Vach et al. prepared some guidelines for the evaluation of direct and indirect clinical benefit covering the following six clinical scenarios: replacement of an invasive procedure, improved accuracy of initial diagnosis, improved accuracy of staging for curative versus palliative treatment, improved accuracy of staging for radiation versus chemotherapy, response evaluation, and acceleration of clinical decisions [41].
Other advanced imaging technologies and biomarkers
Diffusion-weighted MRI
Diffusion-weighted imaging (DWI) is based on the Brownian motion of water within tissue. In contrast to free diffusion, the diffusion of water within biological tissues is restricted by interactions with cell membranes, cell organelles, macromolecules, fibres etc. Thus, diffusion is limited in most parts of malignant tumours due to increased cellularity which decreases the value of the apparent diffusion coefficient (ADC). Originally established in brain imaging, adapted DWI techniques allowing acquisition under free breathing paved the way for extracranial whole-body DWI applications [42]. Based on diffusion characteristics it is possible to distinguish malignant and benign lung nodules [43] and also small-cell lung cancer from NSCLC [44]. Besides tissue characterization in primary staging, DWI offers information of value in monitoring therapy response. Overall, therapy success is mainly indicated by increasing ADC values, in some studies only a few days after starting therapy [45]. In contrast, depending on drug and tumour type, an initial decrease in ADC can also be seen [46], and this might be induced by cellular swelling, reduction in blood flow or haemorrhage. These findings indicate that DWI might represent a complex interplay of several processes and strongly depends on treatment and histological tumour type. Moreover, changes over time have to be observed to draw the right conclusions for a dedicated therapy.
Dynamic contrast-enhanced MRI
Dynamic contrast-enhanced (DCE) MRI is a promising method for tumour characterization and in therapy monitoring. However, several technical aspects have to be taken into account. Although the concentrations of contrast medium normally found in tissue show a linear correlation with the change in spin-lattice relaxation rate, several other factors influence the relationship between contrast medium concentration and signal change in commonly used spoiled gradient echo sequences, including T1 prior to contrast medium injection, flip angle, time of repetition and proton density [47]. Since standard sequences can be used, DCE can easily be integrated in a standard MR protocol. For perfusion quantification, different evaluation methods have been proposed that are mainly based on tracer kinetic models [48]. However, efforts are being made to investigate the role of MRI DCE in therapy monitoring of NSCLC. Chang et al. found distinct changes in perfusion parameters indicating early treatment response to a combined chemotherapy regimen (bevacizumab, gemcitabine, cisplatin) [49].
Quantitative CT perfusion
Currently, efforts are being made to analyse the benefit of measuring tumour perfusion with functional CT. This technique is based on the exchange of iodinated contrast agents between the intravascular space and the extravascular interstitial space. Other possible technologies for measurement of tumour vascularization include 15O-labelled water PET and DCE MRI discussed above. In contrast to iodine-containing contrast agents, [15O]H2O is an ideal perfusion tracer that is freely diffusible and metabolically inert [50]. In spite of different physical backgrounds a good correlation between CT perfusion and [15O]H2O PET has been demonstrated [51]. CT-based techniques can be easily integrated into a clinical routine setting [52], due to short-duration scans and independence from an on-site cyclotron. To further increase perfusion coverage without increasing detector width, repeated spiral scanning and continuous table movement have been combined [53].
The parameters derived from CT perfusion imaging correlate with tumour angiogenesis as reflected by microvessel density (MVD) and VEGF expression [54]. Results from our own group show that higher MVD is associated with higher blood flow and blood volume values [55]. Regarding the assessment of therapy response, some interesting studies have been performed. Tacelli et al. determined whether CT perfusion can depict early perfusion changes in lung cancer treated with antiangiogenic drugs [56]. They found that patients treated with conventional chemotherapy with bevacizumab had a significant perfusion reduction, in contrast to patients without antiangiogenic treatment [56]. Finally, NSCLC with high perfusion values seems to be more sensitive to chemoradiotherapy than tumours with low values, and CT perfusion parameters are significant predictors of early tumour response and overall survival [57].
New radiotracers
Tumour cells are usually highly metabolically active and favour a more inefficient anaerobic pathway, a phenomenon called the Warburg effect. To adjust for the increased glucose demands, glucose transporters and hexokinases are often upregulated, as shown previously. These combined mechanisms allow tumour cells to take up and retain higher levels of FDG than healthy tissues [58]. Because FDG is not cancer-specific and will accumulate in regions with high levels of glucose metabolism and glycolysis, more specific radiotracers are of interest. Besides energy metabolism, there are numerous targets that are specifically upregulated in lung cancer and that could be further elucidated using dedicated radiotracers, including: sustaining proliferative signalling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, activating invasion and metastasis, genome instability, inflammation, evading immune destruction and the tumour microenvironment [59–61]. Blood tests that measure cell-free DNA [62] or anticancer antibodies [63] can be used to diagnose the presence of lung cancer and the cancer subtype, but lack the key benefits of novel radiotracers which provide both spatial and temporal information that is important for guiding further interventional strategies.
There is some evidence that changes in 3′-deoxy-3′-[18F]fluorothymidine (FLT) uptake during radiotherapy exceed test–retest variability and are predictive of early therapy response [64]. A direct comparison between FLT and FDG in NSCLC patients treated with erlotinib revealed that FLT uptake also predicted significantly longer progression-free survival, but not overall survival, and was not predictive of nonprogression after 6 weeks of therapy [65, 66]. A recent study has shown that thymidine phosphorylase, a key enzyme in the pyrimidine nucleoside salvage pathway, catalyses the reversible phosphorylation of thymidine [67]. By regulating the levels of endogenous thymidine, thymidine phosphorylase can influence FLT uptake in cancer cells and in patients with NSCLC. While Kaira et al. [37] described a positive correlation between FDG uptake and EGFR expression, Putora et al. [68] found no correlation between SUV and EGFR mutation status in lung adenocarcinomas. Therefore, methods that would enable in vivo monitoring of receptor drug binding and receptor occupancy, determination of the duration of EGFR inhibition and identification of a primary or secondary mutation in EGFR would be of interest [69]. EGFR comprises three regions as possible targets: an extracellular binding domain, a single hydrophobic transmembrane region, and an intracellular domain with tyrosine kinase activity. EGFR-labelled biomarkers are directed either at the external ligand binding domain using antibodies and Affibodies [70] or at the internal ATP binding domain using small reversible and irreversible inhibitors [69].
Recently, small-animal PET and biodistribution studies have shown that [11C]erlotinib shows high uptake in HCC827 tumour-bearing mice [71]. HCC827 lung cancer cells show high expression of EGFR and harbour an in-frame deletion mutation (delE746-A750), in contrast to A549 and NC1358 cells. Irreversible labelled bioprobes such as [18F]ML04 appear to provide clear and elevated signals in tumour tissue with low background activity levels [69]. Also the new tracer [18F]PEG6-IPQA binds irreversibly with high selectivity to the activated EGFR mutant L858R in NSCLC and might therefore provide additional information as to resistance to gefitinib or erlotinib treatment [72]. For targeting the external binding domain of the EGFR, labelled anti-EGFR monoclonal antibodies such as cetuximab using various radionuclides (64Cu, 88Y, 111In, 125I) have been developed (Fig. 1). These labelled antibodies specifically detect tumours with EGFR overexpression, but often high liver accumulation is present. This limitation can be overcome either by acquiring late images or by adding PEG chains to the conjugating chelators [69]. Affibodies are antibody fragments with a low molecular weight and fast target binding. However, only low to moderate tumour uptake and high kidney uptake limit their range of application.
Uptake patterns of PET tracers FDG (a), FLT (b) and [64Cu]DOTA-cetuximab (c) visualized as maximum intensity profiles in nude mice bearing EGFR overexpressing NSCLC xenograft tumours in the right shoulder. Increased glycolysis as measured with FDG and tumour cell proliferation measured with FLT have both been attributed to tumour aggressiveness. [64Cu]DOTA-cetuximab shows moderate uptake in the tumour, indicating the presence of EGFR overexpression. EGFR overexpression is linked specifically to hallmarks of cancer such as uncontrolled growth, invasion, angiogenic potential and metastasis development. Although the absolute uptake of [64Cu]DOTA-cetuximab in the tumour is similar to that of [18F]FDG and the specificity to the tumour can't compare to that of [18F]FLT, this radiolabeled anti-body not only reveals the presence of EGFR in the tumour, but can give an indication of drug penetration into the tumour
Overexpression of cell surface antigens in malignant tumours is not only of major interest for detection using immuno-SPECT or immuno-PET. The availability of matched imaging and therapeutic radionuclide pairs, such as 124I/131I, 64Cu/67Cu and 86Y/90Y, is a very interesting option for radioimmunotherapy [73]. One example is a radioimmunotherapy approach that uses the lupus-associated (La)-specific murine monoclonal antibody DAB4 radiolabelled with 177Lu [74]. Combining [177Lu]DAB4 with polymerase inhibitors and chemotherapy produced a substantial anti-tumour response in a murine Lewis lung (LL2) model. Immunotherapy that aims to stimulate the immune system is another interesting option for lung cancer treatment [75]. In 2011, the US Food and Drug Administration approved ipilimumab for the treatment of metastatic melanoma [76]. Recently, Neumann et al. identified HLA ligands and T-cell epitopes for potential immunotherapy of lung cancer [77]. It is well known that tumour growth often exceeds the vascular supply and this leads to hypoxia and upregulation of angiogenesis [78]. An interesting target for angiogenesis imaging is integrin αvβ3 which has been reported to be a marker of activated, but not resting, vessels. Several markers that are based on the RGD motif, e.g. [18F]galacto-RGD, are under evaluation in NSCLC and other malignancies [79].
The variable blood flow through leaky, immature vessels in the heterogeneous tumour microenvironment in NSCLC causes hypoxia and acidosis [80]. These factors contribute to a reduced therapy response predisposing patients to metastasis [80]. Hypoxia imaging using PET in NSCLC has been assessed using various radiotracers such as 1H-1-(3-[18F]fluoro-2-hydroxypropyl)-2-nitroimidazole ([18F]FMISO), [64Cu]diacetyl-bis(N4-methylsemicarbazone ([64Cu]ATSM), 1-α-d-(5-deoxy-5-[18F]fluoroarabinofuranosyl)-2-nitroimidazole ([18F]FAZA), 3-[18F]fluoro-2-(4-((2-nitro-1H-imidazol-1-yl)methyl)-1H-1,2,3,-triazol-1-yl)-propan-1-ol ([18F]HX4) and [18F]fluoro-erythro-nitroimidazole ([18F]FETNIM) [81]. There is a large variation in the distribution of hypoxia across different lung tumours. Residual tumour hypoxia at the end of treatment seems to be a prognostic marker in regard to response after chemoradiotherapy, and therefore further studies that focus on hypoxia-based radiation dose escalation are needed [82].
Finally, there are some promising new radiotracer developments based on amino acid compounds. xC − is a transporter involved in the cellular uptake of cystine in exchange for intracellular glutamate, and plays a role in growth and progression of cancer and glutathione-based drug resistance. Baek et al. developed a tracer called (4S)-4-(3-[18F]fluoropropyl)-l-glutamate (BAY 94-9392) that allows assessment of xC − transporter activity with a relatively high cancer detection rate in patients with NSCLC [83]. L-Type amino acid transporter 1 (LAT1) is associated with tumour growth as well as poor outcome, and can be detected using l-[3-18F]-α-methyl tyrosine [84]. l-[3-18F]-α-Methyl tyrosine seems to be an independent prognostic factor in patients with adenocarcinoma [85].
Multiparametric imaging
Hybrid PET/CT
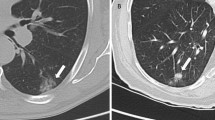
Modern PET/CT scanners provide multifunctional parameters. This is due to the fact that the CT technology has evolved from yielding pure morphology towards more functional information, e.g. provided by CT perfusion as discussed above. Therefore, CT perfusion techniques can be fully integrated into conventional FDG PET/CT studies of lung cancer patients [86]. Results from our own group show that FDG uptake correlates with Ki67, whereas blood flow, blood volume and flow extraction product correlate with MVD [87]. Therefore, these image-derived parameters provide complementary information following noninvasive tumour profiling. This technology also offers the possibility to assess the blood flow–metabolism mismatch that is associated with a poor response to systemic therapy and early relapse or disease progression [88]. Miles et al. were pioneers in this field in NSCLC [89], and we have contributed with new results indicating that this mismatch is dependent on the histological subtype and is more pronounced in squamous cell carcinomas [87]. Possibly due to uncoupling of FDG uptake and perfusion parameters in primary tumours, there is no direct correlation between these two processes [90, 91]. However, in mediastinal lymph nodes in NSCLC patients there is a negative correlation between perfusion parameters and FDG uptake [90] (Fig. 2).
Perfusion maps (a–c, e–g) and FDG PET images (d, h) in a patient with a squamous cell carcinoma (a–d) and a patient with a lymph node metastasis of an adenocarcinoma (e–h). The perfusion maps of blood flow (BF a, e), blood volume (BV b, f) and flow extraction product (K trans c, g) allow noninvasive elucidation of tumour angiogenesis. Compared with FDG uptake, the tumour perfusion parameters are much more heterogeneously distributed across the tumour and the adjacent atelectasis. The negative correlation between perfusion and FDG uptake in a mediastinal lymph node metastasis is reflected by low BF and BV, while FDG uptake is high
Hybrid PET/MRI
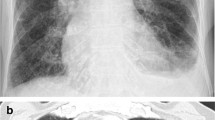
Combined PET/MRI is a new imaging technology that integrates the superior tissue contrast and the functional information derived from MRI with the molecular parameters provided by PET [58]. At the moment, several approaches for the technical integration of the two systems exist, with simultaneous approaches being the most promising [92]. Comparison of whole-body hybrid PET/MRI and PET/CT in pulmonary lesion assessment has revealed similar tumour stages with both imaging systems [93]. However, such a system allows a more dedicated imaging-based tumour characterization, e.g. using DWI and FDG PET [94]. Data from our own group comparing the ADCmin and SUVmax as measures of cell density and glucose metabolism showed a significant negative correlation (r = −0.80, P = 0.0006; Fig. 3). There is most probably an association between the measurements of the two methods because of increased cellularity and glucose metabolism of FDG-avid pulmonary lesions. Ohno et al. investigated the role of DWI and FDG PET in predicting tumour response in patients with NSCLC under chemotherapy, and found that ADC is superior to FDG PET [95]. These findings underline the complementary nature of DWI and FDG PET. It is not clear which parameters are complementary and which parameters can be omitted due to redundant information when dealing with multiparametric imaging.
PET/MR scan of ADC map (left) and superimposed ADC map and FDG PET image (middle) in a 60-year-old female patient with a necrotic bronchial carcinoma of the right lung (squamous cell carcinoma). Right Two-dimensional histogrammed voxel-wise scatterplot of SUV (y axis) and ADC (x axis). The yellow line is the linear regression line. Note the discrepant behaviour of ADC and SUV at the inner rim of the tumour with low ADC and SUV. This example indicates the complementary nature of diffusivity and glycolysis
Radiogenomics
One forward-looking approach for the identification of new prognostic imaging biomarkers is the integration of medical images with high-throughput molecular technologies such as metabolomics and genomics, as well as survival data in public gene expression datasets. This technology is summarized under the term radiogenomics. Gevaert et al. have described a special multistep strategy that may identify new biomarkers when long-term clinical outcomes are not immediately available [96]. This strategy involves integration of CT and PET images and gene microarray data from the study cohort, mapping of the metagenes to publicly available microarray data with survival, and linking of image features expressed in terms of metagenes to public gene expression data. The authors found several interesting associations, e.g. the presence of an internal air bronchogram is related to the overexpression of KRAS and its targets, but only in adenocarcinoma. The image features predicted all 56 metagenes with a mean accuracy of 72 %.
Outlook
The development and use of new imaging biomarkers is still limited because of issues involving insurance coverage, health regulation aspects, and health-care policies. Given the fact that the cost of imaging procedures are only a fraction of the cost of therapy, new concepts need to be implemented. As shown in this review, imaging is an integral part of staging and therapy response assessment in lung cancer as it can document and objectify treatment strategies. New personalized therapy concepts will therefore profit from more refined imaging techniques offering noninvasive biomarkers.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi:10.3322/caac.20107.
Devesa SS, Bray F, Vizcaino AP, Parkin DM. International lung cancer trends by histologic type: male:female differences diminishing and adenocarcinoma rates rising. Int J Cancer. 2005;117:294–9. doi:10.1002/ijc.21183.
Morgensztern D, Ng SH, Gao F, Govindan R. Trends in stage distribution for patients with non-small cell lung cancer: a National Cancer Database survey. J Thorac Oncol. 2010;5:29–33. doi:10.1097/JTO.0b013e3181c5920c.
Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e211S–50. doi:10.1378/chest.12-2355.
Akin O, Brennan SB, Dershaw DD, Ginsberg MS, Gollub MJ, Schöder H, et al. Advances in oncologic imaging: update on 5 common cancers. CA Cancer J Clin. 2012;62:364–93. doi:10.3322/caac.21156.
Reck M, Heigener DF, Mok T, Soria JC, Rabe KF. Management of non-small-cell lung cancer: recent developments. Lancet. 2013;382:709–19. doi:10.1016/s0140-6736(13)61502-0.
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–50. doi:10.1056/NEJMoa061884.
Scagliotti GV, Parikh P, von Pawel J, Biesma B, Vansteenkiste J, Manegold C, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26:3543–51. doi:10.1200/jco.2007.15.0375.
Pignon JP, Tribodet H, Scagliotti GV, Douillard JY, Shepherd FA, Stephens RJ, et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE collaborative group. J Clin Oncol. 2008;26:3552–9. doi:10.1200/jco.2007.13.9030.
Sause W, Kolesar P, Taylor IV S, Johnson D, Livingston R, Komaki R, et al. Final results of phase III trial in regionally advanced unresectable non-small cell lung cancer: Radiation Therapy Oncology Group, Eastern Cooperative Oncology Group, and Southwest Oncology Group. Chest. 2000;117:358–64.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–46. doi:10.1016/s1470-2045(11)70393-x.
Seo JS, Ju YS, Lee WC, Shin JY, Lee JK, Bleazard T, et al. The transcriptional landscape and mutational profile of lung adenocarcinoma. Genome Res. 2012;22:2109–19. doi:10.1101/gr.145144.112.
Annema JT, van Meerbeeck JP, Rintoul RC, Dooms C, Deschepper E, Dekkers OM, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA. 2010;304:2245–52. doi:10.1001/jama.2010.1705.
Fischer B, Lassen U, Mortensen J, Larsen S, Loft A, Bertelsen A, et al. Preoperative staging of lung cancer with combined PET-CT. N Engl J Med. 2009;361:32–9. doi:10.1056/NEJMoa0900043.
Zeliadt SB, Loggers ET, Slatore CG, Au DH, Hebert PL, Klein GJ, et al. Preoperative PET and the reduction of unnecessary surgery among newly diagnosed lung cancer patients in a community setting. J Nucl Med. 2014;55:379–85. doi:10.2967/jnumed.113.124230.
Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg. 2009;15:4–9.
Humphrey LL, Deffebach M, Pappas M, Baumann C, Artis K, Mitchell JP, et al. Screening for lung cancer with low-dose computed tomography: a systematic review to update the US Preventive services task force recommendation. Ann Intern Med. 2013;159:411–20. doi:10.7326/0003-4819-159-6-201309170-00690.
Walker CM, Chung JH, Abbott GF, Little BP, El-Sherief AH, Shepard JA, et al. Mediastinal lymph node staging: from noninvasive to surgical. AJR Am J Roentgenol. 2012;199:W54–64. doi:10.2214/ajr.11.7446.
Gould MK, Kuschner WG, Rydzak CE, Maclean CC, Demas AN, Shigemitsu H, et al. Test performance of positron emission tomography and computed tomography for mediastinal staging in patients with non-small-cell lung cancer: a meta-analysis. Ann Intern Med. 2003;139:879–92.
Lardinois D, Weder W, Hany TF, Kamel EM, Korom S, Seifert B, et al. Staging of non-small-cell lung cancer with integrated positron-emission tomography and computed tomography. N Engl J Med. 2003;348:2500–7. doi:10.1056/NEJMoa022136.
Rosado-de-Christenson ML, Templeton PA, Moran CA. Bronchogenic carcinoma: radiologic-pathologic correlation. Radiographics. 1994;14:429–46. doi:10.1148/radiographics.14.2.8190965. quiz 47–8.
Sun JS, Park KJ, Sheen SS, Yoon JK, Yoon SN, Lee KB, et al. Clinical usefulness of the fluorodeoxyglucose (FDG)-PET maximal standardized uptake value (SUV) in combination with CT features for the differentiation of adenocarcinoma with a bronchioloalveolar carcinoma from other subtypes of non-small cell lung cancers. Lung Cancer. 2009;66:205–10. doi:10.1016/j.lungcan.2009.01.009.
Goeckenjan G, Sitter H, Thomas M, Branscheid D, Flentje M, Griesinger F, et al. Prevention, diagnosis, therapy, and follow-up of lung cancer: interdisciplinary guideline of the German Respiratory Society and the German Cancer Society. Pneumologie. 2011;65:39–59. doi:10.1055/s-0030-1255961.
Silvestri GA, Gould MK, Margolis ML, Tanoue LT, McCrory D, Toloza E, et al. Noninvasive staging of non-small cell lung cancer: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007;132:178S–201. doi:10.1378/chest.07-1360.
Rintoul RC, Tournoy KG, El Daly H, Carroll NR, Buttery RC, van Kralingen K, et al. EBUS-TBNA for the clarification of PET positive intra-thoracic lymph nodes – an international multi-centre experience. J Thorac Oncol. 2009;4:44–8. doi:10.1097/JTO.0b013e3181914357.
De Geus-Oei LF, van der Heijden HF, Corstens FH, Oyen WJ. Predictive and prognostic value of FDG-PET in nonsmall-cell lung cancer: a systematic review. Cancer. 2007;110:1654–64.
Paesmans M, Berghmans T, Dusart M, Garcia C, Hossein-Foucher C, Lafitte JJ, et al. Primary tumor standardized uptake value measured on fluorodeoxyglucose positron emission tomography is of prognostic value for survival in non-small cell lung cancer: update of a systematic review and meta-analysis by the European Lung Cancer Working Party for the International Association for the Study of Lung Cancer Staging Project. J Thorac Oncol. 2010;5:612–9. doi:10.1097/JTO.0b013e3181d0a4f5.
Berghmans T, Paesmans M, Sculier JP. Prognostic factors in stage III non-small cell lung cancer: a review of conventional, metabolic and new biological variables. Ther Adv Med Oncol. 2011;3:127–38. doi:10.1177/1758834011401951.
Machtay M, Duan F, Siegel BA, Snyder BS, Gorelick JJ, Reddin JS, et al. Prediction of survival by [18F]fluorodeoxyglucose positron emission tomography in patients with locally advanced non-small-cell lung cancer undergoing definitive chemoradiation therapy: results of the ACRIN 6668/RTOG 0235 trial. J Clin Oncol. 2013;31:3823–30. doi:10.1200/jco.2012.47.5947.
Usmanij EA, de Geus-Oei LF, Troost EG, Peters-Bax L, van der Heijden EH, Kaanders JH, et al. 18F-FDG PET early response evaluation of locally advanced non-small cell lung cancer treated with concomitant chemoradiotherapy. J Nucl Med. 2013;54:1528–34. doi:10.2967/jnumed.112.116921.
Takahashi R, Hirata H, Tachibana I, Shimosegawa E, Inoue A, Nagatomo I, et al. Early [18F]fluorodeoxyglucose positron emission tomography at two days of gefitinib treatment predicts clinical outcome in patients with adenocarcinoma of the lung. Clin Cancer Res. 2012;18:220–8. doi:10.1158/1078-0432.CCR-11-0868.
Tiseo M, Ippolito M, Scarlattei M, Spadaro P, Cosentino S, Latteri F, et al. Predictive and prognostic value of early response assessment using 18FDG-PET in advanced non-small cell lung cancer patients treated with erlotinib. Cancer Chemother Pharmacol. 2014;73:299–307. doi:10.1007/s00280-013-2356-x.
Schaake EE, Kappers I, Codrington HE, Valdés Olmos RA, Teertstra HJ, van Pel R, et al. Tumor response and toxicity of neoadjuvant erlotinib in patients with early-stage non-small-cell lung cancer. J Clin Oncol. 2012;30:2731–8. doi:10.1200/jco.2011.39.4882.
Ulger S, Demirci NY, Eroglu FN, Cengiz HH, Tunc M, Tatci E, et al. High FDG uptake predicts poorer survival in locally advanced nonsmall cell lung cancer patients undergoing curative radiotherapy, independently of tumor size. J Cancer Res Clin Oncol. 2014;140:495–502. doi:10.1007/s00432-014-1591-9.
Vera P, Mezzani-Saillard S, Edet-Sanson A, Ménard JF, Modzelewski R, Thureau S, et al. FDG PET during radiochemotherapy is predictive of outcome at 1 year in non-small-cell lung cancer patients: a prospective multicentre study (RTEP2). Eur J Nucl Med Mol Imaging. 2014;41:1057–65. doi:10.1007/s00259-014-2687-9.
Nair VS, Gevaert O, Davidzon G, Napel S, Graves EE, Hoang CD, et al. Prognostic PET 18F-FDG uptake imaging features are associated with major oncogenomic alterations in patients with resected non-small cell lung cancer. Cancer Res. 2012;72:3725–34. doi:10.1158/0008-5472.can-11-3943.
Kaira K, Serizawa M, Koh Y, Takahashi T, Yamaguchi A, Hanaoka H, et al. Biological significance of 18F-FDG uptake on PET in patients with non-small-cell lung cancer. Lung Cancer. 2014;83:197–204. doi:10.1016/j.lungcan.2013.11.025.
Vesselle H, Salskov A, Turcotte E, Wiens L, Schmidt R, Jordan CD, et al. Relationship between non-small cell lung cancer FDG uptake at PET, tumor histology, and Ki-67 proliferation index. J Thorac Oncol. 2008;3:971–8. doi:10.1097/JTO.0b013e31818307a7.
Suzawa N, Ito M, Qiao S, Uchida K, Takao M, Yamada T, et al. Assessment of factors influencing FDG uptake in non-small cell lung cancer on PET/CT by investigating histological differences in expression of glucose transporters 1 and 3 and tumour size. Lung Cancer. 2011;72:191–8. doi:10.1016/j.lungcan.2010.08.017.
Lasnon C, Desmonts C, Quak E, Gervais R, Do P, Dubos-Arvis C, et al. Harmonizing SUVs in multicentre trials when using different generation PET systems: prospective validation in non-small cell lung cancer patients. Eur J Nucl Med Mol Imaging. 2013;40:985–96. doi:10.1007/s00259-013-2391-1.
Vach W, Høilund-Carlsen PF, Gerke O, Weber WA. Generating evidence for clinical benefit of PET/CT in diagnosing cancer patients. J Nucl Med. 2011;52 Suppl 2:77S–85. doi:10.2967/jnumed.110.085704.
Takahara T, Imai Y, Yamashita T, Yasuda S, Nasu S, Van Cauteren M. Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med. 2004;22:275–82.
Chen L, Zhang J, Bao J, Zhang L, Hu X, Xia Y, et al. Meta-analysis of diffusion-weighted MRI in the differential diagnosis of lung lesions. J Magn Reson Imaging. 2013;37:1351–8. doi:10.1002/jmri.23939.
Koyama H, Ohno Y, Nishio M, Takenaka D, Yoshikawa T, Matsumoto S, et al. Diffusion-weighted imaging vs STIR turbo SE imaging: capability for quantitative differentiation of small-cell lung cancer from non-small-cell lung cancer. Br J Radiol. 2014;87:20130307. doi:10.1259/bjr.20130307.
Zhai G, Kim H, Sarver D, Samuel S, Whitworth L, Umphrey H, et al. Early therapy assessment of combined anti-DR5 antibody and carboplatin in triple-negative breast cancer xenografts in mice using diffusion-weighted imaging and (1)H MR spectroscopy. J Magn Reson Imaging. 2014;39:1588–94. doi:10.1002/jmri.24319.
Schraml C, Schwenzer NF, Martirosian P, Bitzer M, Lauer U, Claussen CD, et al. Diffusion-weighted MRI of advanced hepatocellular carcinoma during sorafenib treatment: initial results. AJR Am J Roentgenol. 2009;193:W301–7. doi:10.2214/AJR.08.2289.
Evelhoch JL. Key factors in the acquisition of contrast kinetic data for oncology. J Magn Reson Imaging. 1999;10:254–9.
Sourbron SP, Buckley DL. Classic models for dynamic contrast-enhanced MRI. NMR Biomed. 2013;26:1004–27. doi:10.1002/nbm.2940.
Chang YC, Yu CJ, Chen CM, Hu FC, Hsu HH, Tseng WY, et al. Dynamic contrast-enhanced MRI in advanced nonsmall-cell lung cancer patients treated with first-line bevacizumab, gemcitabine, and cisplatin. J Magn Reson Imaging. 2012;36:387–96. doi:10.1002/jmri.23660.
Hoekstra CJ, Stroobants SG, Hoekstra OS, Smit EF, Vansteenkiste JF, Lammertsma AA. Measurement of perfusion in stage IIIA-N2 non-small cell lung cancer using H(2)(15)O and positron emission tomography. Clin Cancer Res. 2002;8:2109–15.
Kramer GM, Yaqub M, Bahce I, Smit EF, Lubberink M, Hoekstra OS, et al. CT-perfusion versus [(15)O]H2O PET in lung tumors: effects of CT-perfusion methodology. Med Phys. 2013;40:052502. doi:10.1118/1.4798560.
Miles KA, Charnsangavej C, Lee FT, Fishman EK, Horton K, Lee TY. Application of CT in the investigation of angiogenesis in oncology. Acad Radiol. 2000;7:840–50.
Haberland U, Klotz E, Abolmaali N. Performance assessment of dynamic spiral scan modes with variable pitch for quantitative perfusion computed tomography. Investig Radiol. 2010;45:378–86. doi:10.1097/RLI.0b013e3181dfda9f.
Ma SH, Le HB, Jia BH, Wang ZX, Xiao ZW, Cheng XL, et al. Peripheral pulmonary nodules: relationship between multi-slice spiral CT perfusion imaging and tumor angiogenesis and VEGF expression. BMC Cancer. 2008;8:186. doi:10.1186/1471-2407-8-186.
Spira D, Neumeister H, Spira SM, Hetzel J, Spengler W, von Weyhern CH, et al. Assessment of tumor vascularity in lung cancer using volume perfusion CT (VPCT) with histopathologic comparison: a further step toward an individualized tumor characterization. J Comput Assist Tomogr. 2013;37:15–21. doi:10.1097/RCT.0b013e318277c84f.
Tacelli N, Santangelo T, Scherpereel A, Duhamel A, Deken V, Klotz E, et al. Perfusion CT allows prediction of therapy response in non-small cell lung cancer treated with conventional and anti-angiogenic chemotherapy. Eur Radiol. 2013;23:2127–36. doi:10.1007/s00330-013-2821-2.
Wang J, Wu N, Cham MD, Song Y. Tumor response in patients with advanced non-small cell lung cancer: perfusion CT evaluation of chemotherapy and radiation therapy. AJR Am J Roentgenol. 2009;193:1090–6. doi:10.2214/ajr.08.1367.
Sauter AW, Wehrl HF, Kolb A, Judenhofer MS, Pichler BJ. Combined PET/MRI: one step further in multimodality imaging. Trends Mol Med. 2010;16:508–15. doi:10.1016/j.molmed.2010.08.003.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74. doi:10.1016/j.cell.2011.02.013.
Holland JP, Cumming P, Vasdev N. PET of signal transduction pathways in cancer. J Nucl Med. 2012;53:1333–6. doi:10.2967/jnumed.112.105387.
Wood SL, Pernemalm M, Crosbie PA, Whetton AD. The role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targets. Cancer Treat Rev. 2014;40:558–66. doi:10.1016/j.ctrv.2013.10.001.
Nygaard AD, Holdgaard PC, Spindler KL, Pallisgaard N, Jakobsen A. The correlation between cell-free DNA and tumour burden was estimated by PET/CT in patients with advanced NSCLC. Br J Cancer. 2014;110:363–8. doi:10.1038/bjc.2013.705.
Lam S, Boyle P, Healey GF, Maddison P, Peek L, Murray A, et al. EarlyCDT-Lung: an immunobiomarker test as an aid to early detection of lung cancer. Cancer Prev Res (Phila). 2011;4:1126–34. doi:10.1158/1940-6207.capr-10-0328.
Trigonis I, Koh PK, Taylor B, Tamal M, Ryder D, Earl M, et al. Early reduction in tumour [(18)F]fluorothymidine (FLT) uptake in patients with non-small cell lung cancer (NSCLC) treated with radiotherapy alone. Eur J Nucl Med Mol Imaging. 2014;41:682–93. doi:10.1007/s00259-013-2632-3.
Kahraman D, Scheffler M, Zander T, Nogova L, Lammertsma AA, Boellaard R, et al. Quantitative analysis of response to treatment with erlotinib in advanced non-small cell lung cancer using 18F-FDG and 3′-deoxy-3′-18F-fluorothymidine PET. J Nucl Med. 2011;52:1871–7. doi:10.2967/jnumed.111.094458.
Zander T, Scheffler M, Nogova L, Kobe C, Engel-Riedel W, Hellmich M, et al. Early prediction of nonprogression in advanced non-small-cell lung cancer treated with erlotinib by using [(18)F]fluorodeoxyglucose and [(18)F]fluorothymidine positron emission tomography. J Clin Oncol. 2011;29:1701–8. doi:10.1200/jco.2010.32.4939.
Lee SJ, Yeo JS, Lee HJ, Lee EJ, Kim SY, Jang SJ, et al. Thymidine phosphorylase influences [(18)F]fluorothymidine uptake in cancer cells and patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2014;41:1327–35. doi:10.1007/s00259-014-2712-z.
Putora PM, Müller J, Borovicka J, Plasswilm L, Schmidt F. Relevance of incidental colorectal FDG-PET/CT-enhanced lesions. Onkologie. 2013;36:200–4. doi:10.1159/000350302.
Mishani E, Hagooly A. Strategies for molecular imaging of epidermal growth factor receptor tyrosine kinase in cancer. J Nucl Med. 2009;50:1199–202. doi:10.2967/jnumed.109.062117.
Miao Z, Ren G, Liu H, Qi S, Wu S, Cheng Z. PET of EGFR expression with an 18F-labeled affibody molecule. J Nucl Med. 2012;53:1110–8. doi:10.2967/jnumed.111.100842.
Memon AA, Jakobsen S, Dagnaes-Hansen F, Sorensen BS, Keiding S, Nexo E. Positron emission tomography (PET) imaging with [11C]-labeled erlotinib: a micro-PET study on mice with lung tumor xenografts. Cancer Res. 2009;69:873–8. doi:10.1158/0008-5472.can-08-3118.
Yeh HH, Ogawa K, Balatoni J, Mukhapadhyay U, Pal A, Gonzalez-Lepera C, et al. Molecular imaging of active mutant L858R EGF receptor (EGFR) kinase-expressing nonsmall cell lung carcinomas using PET/CT. Proc Natl Acad Sci U S A. 2011;108:1603–8. doi:10.1073/pnas.1010744108.
Pecking AP, Bellet D, Alberini JL. Immuno-SPET/CT and immuno-PET/CT: a step ahead to translational imaging. Clin Exp Metastasis. 2012;29:847–52. doi:10.1007/s10585-012-9501-5.
Staudacher AH, Al-Ejeh F, Fraser CK, Darby JM, Roder DM, Ruszkiewicz A, et al. The La antigen is over-expressed in lung cancer and is a selective dead cancer cell target for radioimmunotherapy using the La-specific antibody APOMAB®. EJNMMI Res. 2014;4:2. doi:10.1186/2191-219x-4-2.
Tartour E, Zitvogel L. Lung cancer: potential targets for immunotherapy. Lancet Respir Med. 2013;1:551–63. doi:10.1016/s2213-2600(13)70159-0.
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi:10.1056/NEJMoa1003466.
Neumann A, Hörzer H, Hillen N, Klingel K, Schmid-Horch B, Bühring HJ, et al. Identification of HLA ligands and T-cell epitopes for immunotherapy of lung cancer. Cancer Immunol Immunother. 2013;62:1485–97. doi:10.1007/s00262-013-1454-2.
Höckel M, Vaupel P. Tumor hypoxia: definitions and current clinical, biologic, and molecular aspects. J Natl Cancer Inst. 2001;93:266–76.
Beer AJ, Lorenzen S, Metz S, Herrmann K, Watzlowik P, Wester HJ, et al. Comparison of integrin alphaVbeta3 expression and glucose metabolism in primary and metastatic lesions in cancer patients: a PET study using 18F-galacto-RGD and 18F-FDG. J Nucl Med. 2008;49:22–9. doi:10.2967/jnumed.107.045864.
Graves EE, Maity A, Le QT. The tumor microenvironment in non-small-cell lung cancer. Semin Radiat Oncol. 2010;20:156–63. doi:10.1016/j.semradonc.2010.01.003.
Bollineni VR, Wiegman EM, Pruim J, Groen HJ, Langendijk JA. Hypoxia imaging using positron emission tomography in non-small cell lung cancer: implications for radiotherapy. Cancer Treat Rev. 2012;38:1027–32. doi:10.1016/j.ctrv.2012.04.003.
Thorwarth D, Alber M. Implementation of hypoxia imaging into treatment planning and delivery. Radiother Oncol. 2010;97:172–5. doi:10.1016/j.radonc.2010.05.012.
Baek S, Choi CM, Ahn SH, Lee JW, Gong G, Ryu JS, et al. Exploratory clinical trial of (4S)-4-(3-[18F]fluoropropyl)-L-glutamate for imaging xC- transporter using positron emission tomography in patients with non-small cell lung or breast cancer. Clin Cancer Res. 2012;18:5427–37. doi:10.1158/1078-0432.ccr-12-0214.
Kaira K, Oriuchi N, Shimizu K, Imai H, Tominaga H, Yanagitani N, et al. Comparison of L-type amino acid transporter 1 expression and L-[3-18F]-α-methyl tyrosine uptake in outcome of non-small cell lung cancer. Nucl Med Biol. 2010;37:911–6. doi:10.1016/j.nucmedbio.2010.06.004.
Kaira K, Oriuchi N, Shimizu K, Tominaga H, Yanagitani N, Sunaga N, et al. 18F-FMT uptake seen within primary cancer on PET helps predict outcome of non-small cell lung cancer. J Nucl Med. 2009;50:1770–6. doi:10.2967/jnumed.109.066837.
Ippolito D, Capraro C, Guerra L, De Ponti E, Messa C, Sironi S. Feasibility of perfusion CT technique integrated into conventional 18FDG/PET-CT studies in lung cancer patients: clinical staging and functional information in a single study. Eur J Nucl Med Mol Imaging. 2013;40:156–65. doi:10.1007/s00259-012-2273-y.
Sauter AW, Winterstein S, Spira D, Hetzel J, Schulze M, Mueller M, et al. Multifunctional profiling of non-small cell lung cancer using 18F-FDG PET/CT and volume perfusion CT. J Nucl Med. 2012;53:521–9. doi:10.2967/jnumed.111.097865.
Mankoff DA, Dunnwald LK, Partridge SC, Specht JM. Blood flow-metabolism mismatch: good for the tumor, bad for the patient. Clin Cancer Res. 2009;15:5294–6. doi:10.1158/1078-0432.ccr-09-1448.
Miles KA, Griffiths MR, Keith CJ. Blood flow-metabolic relationships are dependent on tumour size in non-small cell lung cancer: a study using quantitative contrast-enhanced computer tomography and positron emission tomography. Eur J Nucl Med Mol Imaging. 2006;33:22–8. doi:10.1007/s00259-005-1932-7.
Sauter AW, Spira D, Schulze M, Pfannenberg C, Hetzel J, Reimold M, et al. Correlation between [18F]FDG PET/CT and volume perfusion CT in primary tumours and mediastinal lymph nodes of non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2013;40:677–84. doi:10.1007/s00259-012-2318-2.
van Elmpt W, Das M, Hüllner M, Sharifi H, Zegers CM, Reymen B, et al. Characterization of tumor heterogeneity using dynamic contrast enhanced CT and FDG-PET in non-small cell lung cancer. Radiother Oncol. 2013;109:65–70. doi:10.1016/j.radonc.2013.08.032.
Wehrl HF, Sauter AW, Judenhofer MS, Pichler BJ. Combined PET/MR imaging – technology and applications. Technol Cancer Res Treat. 2010;9:5–20.
Schwenzer NF, Schraml C, Müller M, Brendle C, Sauter A, Spengler W, et al. Pulmonary lesion assessment: comparison of whole-body hybrid MR/PET and PET/CT imaging – pilot study. Radiology. 2012;264:551–8. doi:10.1148/radiol.12111942.
Schmidt H, Brendle C, Schraml C, Martirosian P, Bezrukov I, Hetzel J, et al. Correlation of simultaneously acquired diffusion-weighted imaging and 2-deoxy-[18F] fluoro-2-D-glucose positron emission tomography of pulmonary lesions in a dedicated whole-body magnetic resonance/positron emission tomography system. Investig Radiol. 2013;48:247–55. doi:10.1097/RLI.0b013e31828d56a1.
Ohno Y, Koyama H, Yoshikawa T, Matsumoto K, Takahashi M, Van Cauteren M, et al. T2* measurements of 3-T MRI with ultrashort TEs: capabilities of pulmonary function assessment and clinical stage classification in smokers. AJR Am J Roentgenol. 2011;197:W279–85. doi:10.2214/AJR.10.5350.
Gevaert O, Xu J, Hoang CD, Leung AN, Xu Y, Quon A, et al. Non-small cell lung cancer: identifying prognostic imaging biomarkers by leveraging public gene expression microarray data – methods and preliminary results. Radiology. 2012;264:387–96. doi:10.1148/radiol.12111607.
Acknowledgments
The work of Mark Divine was funded by the German Federal Ministry of Education and Research (BMBF) grant no. 0316186E.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sauter, A.W., Schwenzer, N., Divine, M.R. et al. Image-derived biomarkers and multimodal imaging strategies for lung cancer management. Eur J Nucl Med Mol Imaging 42, 634–643 (2015). https://doi.org/10.1007/s00259-014-2974-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2974-5