Abstract
Clinical studies have demonstrated that hybrid single photon emission computed tomography (SPECT)/CT for various diagnostic issues has an added value as compared to SPECT alone. However, the combined acquisition of functional and anatomical images can substantially increase radiation exposure to patients, in particular when using a hybrid system with diagnostic CT capabilities. It is, therefore, essential to carefully balance the diagnostic needs and radiation protection requirements. To this end, the evidence on health effects induced by ionizing radiation is outlined. In addition, the essential concepts for estimating radiation doses and lifetime attributable cancer risks associated with SPECT/CT examinations are presented taking into account both the new recommendations of the International Commission on Radiological Protection (ICRP) as well as the most recent radiation risk models. Representative values of effective dose and lifetime attributable risk are reported for ten frequently used SPECT radiopharmaceuticals and five fully diagnostic partial-body CT examinations. A diagnostic CT scan acquired as part of a combined SPECT/CT examination contributes considerably to, and for some applications even dominates, the total patient exposure. For the common SPECT and CT examinations considered in this study, the lifetime attributable risk of developing a radiation-related cancer is less than 0.27 %/0.37 % for men/women older than 16 years, respectively, and decreases markedly with increasing age at exposure. Since there is no clinical indication for a SPECT/CT examination unless an emission scan has been indicated, the issue on justification comes down to the question of whether it is necessary to additionally acquire a low-dose CT for attenuation correction and anatomical localization of tracer uptake or even a fully diagnostic CT. In any case, SPECT/CT studies have to be optimized, e.g. by adapting dose reduction measures from state-of-the-art CT practice, and exposure levels should not exceed the national diagnostic reference levels for standard situations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medical imaging using ionizing radiation always poses some risk of adverse health effects to the persons examined—especially radiation-related cancer. This particularly applies to patient studies using hybrid positron emission tomography (PET)/CT or single photon emission computed tomography (SPECT)/CT devices that combine two imaging modalities, both of which can expose patients to relatively high radiation doses: a positron or single photon emission tomograph for functional imaging and a CT system for anatomical imaging [1, 2]. The particular roles and perspectives of both these hybrid imaging technologies for health care are still a matter of debate [3].
According to a recent international survey [4], the majority of SPECT/CT centres do not fully utilize the diagnostic potential of the CT component of dual-modality systems. This is basically due to the high fraction of first-generation SPECT/CTs currently in clinical operation that are equipped only with a lower-quality CT component designed for attenuation correction of the emission data and anatomical localization of radiotracer uptake. However, most recent second-generation SPECT/CTs are equipped with state-of-the-art CT technology providing a high-output X-ray tube and an axially extended detector system. This technical progress will not only improve the clinical flexibility and diagnostic confidence in hybrid SPECT/CT imaging but it will also increase radiation exposure to patients substantially. It is, therefore, essential to carefully balance the diagnostic needs and radiation protection requirements.
From a radiation protection point of view, SPECT/CT is actually more challenging and methodologically complex than PET/CT for several reasons:
-
As compared to PET, there is a much larger number of approved and, due to the availability of commercial kits, clinically accessible radiopharmaceuticals for SPECT, some of which may subject patients to considerable levels of radiation due to the long half-life of the gamma emitters used for radiolabelling in cases of a non-critical use.
-
Except for brain and cardiac examinations, SPECT/CT studies are usually performed after conventional planar scintigraphy and generally focus on a specific body region requiring more detailed evaluation using the hybrid tomographic imaging technology. Accordingly, X-ray dosimetry has to be adapted to the particular scan region in SPECT/CT, which is not necessary for the majority of PET/CT studies carried out as whole-body scans.
-
PET/CT is being used predominantly for imaging elderly cancer patients with a reduced radiation susceptibility and life expectancy, whereas SPECT/CT examinations are more often carried out in younger patients suffering from benign diseases (see below).
The aim of this review article is to outline the evidence on health effects induced by ionizing radiation, to present the essential concepts for estimating radiation doses and risks associated with SPECT and CT examinations as well representative results, and to discuss various aspects that have to be considered in the process of justification and optimization of SPECT/CT studies, in particular when using a hybrid system with diagnostic CT capabilities.
Evidence of health hazards from ionizing radiation and principles of radiation protection
Radiation exposure of patients undergoing a SPECT/CT examination may lead to stochastic health effects, the most significant being the induction of cancer. Cancers caused by ionizing radiation occur after a latency period of several years to decades after the time of exposure. They do not differ in clinical appearance from cancers caused by other factors. Radiation-induced cancers can thus not be recognized as such, and it is only by means of epidemiological studies that increases in the cancer incidence of irradiated groups can be detected.
Increased cancer rates have been demonstrated in humans through various radio-epidemiological studies at moderate or high doses. The so-called Life Span Study (LSS) of the survivors of the atomic bombings in Hiroshima and Nagasaki is the most important one of these studies [5]. The follow-up of the atomic bomb survivors has provided detailed knowledge of the relationships between radiation risk and a variety of factors, such as the absorbed dose, the age at exposure, the age at diagnosis and other parameters. The data are largely supported by a multitude of smaller studies, mostly on groups of individuals exposed for medical reasons, both in diagnostics and therapy [6].
Until now, there is considerable controversy regarding the risk of low levels of radiation (< 100 mSv), typical of diagnostic radiation exposures, since radiation risks evaluated at low dose levels are not based on experimental and epidemiological evidence [7–9]. Given this lack of evidence, estimates on risk, derived from high doses, have been extrapolated down to low dose levels by various scientific bodies, including the International Commission on Radiological Protection (ICRP, [10]), the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR, [11]), and the Biological Effects on Ionizing Radiation Committee (BEIR, [6]). Estimates on risk per unit of dose have been derived using the so-called linear, no-threshold (LNT) hypothesis, which is based on the assumptions that (1) any radiation dose—no matter how small—may cause an increase in risk and (2) the probability of this increase is proportional to the dose absorbed in the tissue. Although the risk evaluated at low dose levels is thus hypothetical, it is prudent to assume that it exists and that the LNT model represents an upper bound for it. It is for this reason that current radiation protection standards as well as risk assessments are based on the LNT hypothesis [10].
In line with this philosophy, current radiation protection recommendations and directives [e.g. 12–14] require that
-
all new types of radiodiagnostic procedures shall be justified in advance before being generally adopted;
-
all individual medical exposures shall be justified in advance taking into account the specific objectives of the exposure and the characteristics of the individual involved;
-
all procedures shall be optimized to keep doses as low as reasonably achievable (ALARA principle) consistent with obtaining the required diagnostic information;
-
diagnostic reference levels (DRLs) shall be established and used both for common and for dose-intensive types of radiodiagnostic procedures.
Estimation of radiation doses and risks to patients in SPECT/CT
Fundamental dose quantities
It is generally assumed that the probability of detrimental radiation effects depends on the energy deposited by ionizing radiation in a specified organ or tissue, T. Therefore, the fundamental physical dose quantity is the absorbed dose D T (given in the unit gray, 1 Gy = 1 J/kg), which is defined as the radiation energy absorbed in a small volume element of matter divided by its mass. For radiological protection purposes, the absorbed dose is averaged over an organ or tissue and weighted by a dimensionless radiation-weighting factor, w R, to reflect the difference in biological effectiveness of radiation with a low and high linear energy transfer (LET). The resulting weighted dose is designated as the organ equivalent dose H T = w R D T (given in the unit sievert, Sv = 1 J/kg). For low LET radiation, such as X-rays and gamma radiation, w R is equal to 1.
Tissues and organs are not equally sensitive to the effects of ionizing radiation. For this reason, tissue-weighting factors, w T , are provided by the ICRP for a reference population of equal numbers of both sexes, covering a wide range of ages [10]. These factors indicate the relative proportion of each organ or tissue in total health detriment resulting from uniform irradiation of the whole body. If the body is exposed in a non-uniform manner, as for example in a patient undergoing a SPECT/CT examination, the sum of the products of the sex-averaged organ doses and the corresponding tissue-weighting factors determined for each of the various organs or tissues exposed has to be computed according to the following equation:
The resulting quantity is denoted as effective dose E (in Sv). Based on this dose quantity, it is possible to compare and add the probability of stochastic radiation effects resulting from different radiation exposures—as for example a SPECT or CT examination yielding a different pattern of dose distribution in the body. It should be noted, however, that the concept of effective dose facilitates only a generic assessment of stochastic radiation risks since the age and sex of exposed individuals are not taken into account. Nevertheless, it provides a rational framework for the justification and optimization of radiological imaging procedures.
Based on the latest available scientific information, the tissue-weighting factors, w T , were modified in 2007 by the ICRP [10]. The most significant changes from the previously held values [15] relate to breast (0.05 → 0.12), gonads (0.2 → 0.08) and the remainder tissues (0.05 → 0.12 using a simplified additive system).
Measurable dose-related quantities
In practice, neither organ doses nor effective doses can be measured directly. In order to overcome this difficulty, dose-related quantities are defined for radiodiagnostic procedures, which can easily be measured and documented for each patient examination. Examples are the activity (A) of a specific radiopharmaceutical administered for nuclear medicine diagnostics or the computed tomography dose index (CTDI) and the dose-length product (DLP) in CT. These quantities are not only used to compare different SPECT and CT protocols but they also form the basis for estimating organ and effective doses.
The weighted CTDI (CTDI w given in mGy) indicates the average dose inside an irradiated slice that would result if the axial dose profile was entirely concentrated in a rectangular profile of width equal to the nominal slice thickness. It is measured using a standardized CT dosimetry phantom, thus taking into account the effect of both scan parameters (e.g. tube voltage, current-time product) and system-specific factors (e.g. beam filtration, geometry, overbeaming). Whenever an extended axial body region is scanned continuously instead of acquiring data from only a single slice, as is usually the case in spiral CT, the dose for a particular slice may be increased or reduced depending on the table feed. In this case, the average dose is given by the volume CTDI
with p being the pitch factor that characterizes the degree of packing of the slice profiles. For p < 1 the slices overlap, resulting in an increase of local dose. Besides this dose quantity, the length (L) of the scan region is the second important parameter that determines radiation exposure of a patient undergoing a CT procedure. Therefore, the DLP
(given in mGy cm) is used as an additional dose descriptor to characterize the integral dose delivered to the patient. Both the CTDI vol and DLP value of a CT scan have to be displayed at the operator’s console of the device.
For ten radiopharmaceuticals frequently used for SPECT examinations in Germany, typical activities administered to adult patients are given in Table 1. Representative values of CTDI vol, DLP and L are summarized in Table 2 for fully diagnostic CT scans of five body regions. The median values and interquartile intervals of the measurable dose-related quantities given in both tables are based on the evaluation of a large number of SPECT and CT examinations carried out in a wide range of hospitals and private practices in Germany. The variation of the considered quantities (described as deviation of the quartiles from the median) is somewhat greater for the CT scans (CTDI vol < 42 %, DLP < 58 %) than for the activities applied for SPECT examinations (< 32 %).
Estimation of organ and effective doses
Organ doses from the intake of radiolabelled compounds, such as SPECT radiopharmaceuticals, cannot be measured; they can only be estimated on the basis of biokinetic and dosimetric models [16]. Biokinetic models describe the uptake and retention of incorporated radionuclides in source regions of the body where they accumulate as well as their excretion from the body. They are used to calculate the numbers of nuclear transformations in the source regions which are needed to calculate the dose to target tissues by dosimetric models. In general, biokinetic models are formulated as compartment models. If the tracer is intravenously injected, the starting compartment represents the blood pool from where the radiopharmaceutical is transported by active or passive processes to other tissue compartments, representing the source regions where it accumulates, and is excreted (mainly) via urine and faeces. In general, the retention in a compartment can be described by a biological half-life, i.e. by a period of time within which half of the material is removed from the compartment. Dosimetric models are used to calculate the dose to a target tissue due to a nuclear transformation in the considered source regions. For this purpose, absorbed fractions AF(r T ← r S ) are determined, i.e. the fraction of the energy emitted in a source region r S which is absorbed in a target tissue r T . For penetrating gamma radiation, absorbed fractions are calculated by Monte Carlo methods based on anthropomorphic body phantoms which describe the position and the form of the source regions and target tissues. Combining the results from both biokinetic and dosimetric models, dose coefficients h(r T ) (in μSv/MBq) are computed that give the equivalent dose H T to an organ T per unit activity intake. Once these dose coefficients are available, organ equivalent doses and the effective dose can simply be estimated for a particular SPECT examination from the administered activity by
respectively. In this equation, h E is the dose coefficient for the effective dose.
The preliminary h E values summarized in Table 1 for ten SPECT tracers are computed by means of the biokinetic models developed by the ICRP [17–19] assuming a bladder voiding interval of 3.5 h. It should be noted that the given dose coefficients differ by between −30 % (99mTc-DTPA, 99mTc-bisphosphonates) and +60 % (99mTc-red blood cells) from the data given in the three mentioned ICRP publications due to the use of the new body reference phantoms (see below) and tissue-weighting factors specified in ICRP Publication 103 [10]. For the considered SPECT tracers, the calculated h E values vary between about 3 and 120 μSv/MBq. As the physical half-life of the nuclide used for radiolabelling is a major determinant of patient exposure, the dose coefficients estimated for the 99mTc-labelled radiopharmaceuticals are markedly lower (h E < 17 μSv/MBq) than for the compounds labelled with 111In, 201Tl and 123I (h E > 40 μSv/MBq).
Monte Carlo methods based on anthropomorphic body phantoms can in principle also be used to compute organ doses for any CT scan from the measured dose-related parameters CTDI vol and DLP. However, this time-consuming approach is not practicable given the large variety of CT systems and the variability of scan parameters applied in routine clinical practice. Therefore, organ and effective doses computed for only a few CT systems and parameter settings are used and corrected properly to be applicable to other CT systems and protocols [20]. This task is supported by easy-to-handle software programs [e.g. 21–23]. Alternatively, effective doses can be very roughly estimated from the DLP by
with K E being a body region-specific conversion factor. In the European Guidelines for Multislice Computed Tomography [24] conversion factors are given (in mSv/mGy/cm) for the head (0.0023), neck (0.0054), chest (0.019), abdomen (0.017), pelvis (0.017) and legs (0.0008). However, these values were derived by using the old tissue-weighting factors given in ICRP Publication 60 [15]. When an automatic exposure control is used, the effective CTDI vol or DLP indicated by the system after the scan can be used as surrogate parameter to take the variation of the tube current into account approximately [25].
For a long time, mathematical phantoms have been used for dose computations describing organs and tissues in the human body by simple geometric objects. They are now being replaced by much more realistic voxel phantoms derived from MRI or CT images of real persons. For purposes of radiation protection, voxel phantoms are adjusted to the dimensions of the ICRP reference persons [26]. Reference voxel phantoms for an adult man (body weight 74 kg, body mass index 24 kg/m2) and woman (60 kg, 23 kg/m2) are published in ICRP Publication 110 [27] and should be used for the estimation of organ and effective doses.
Independent of the particular biokinetic and dosimetric model used for dose estimation, the resulting dose values always hold for a reference person. Since the particular stature, anatomy, physiology and metabolism of individual patients are not taken into account, dose estimates are generic rather than patient specific.
For the ten SPECT and five fully diagnostic single-phase CT examinations listed in Tables 1 and 2, respectively, effective doses have been calculated from the median values of the corresponding measurable dose-related quantities. Effective doses for SPECT tracers that are intravenously injected (i.e. not inhaled) are between about 2 and 10 mSv, thus varying much less than the corresponding dose coefficients, h E. The higher doses per activity when imaging compounds labelled with the longer-lived isotopes 111In, 201Tl and 123I are thus compensated by lower activities administered to the patients. CT scans of the brain yield the highest local dose levels (CTDI vol) but only relatively low effective doses because the irradiated tissues have a low tissue-weighting factor. In contrast, examinations of the abdomen result in much lower local doses but in high effective doses due to both an extended scan range and higher tissue-weighting factors of the exposed tissues.
The average values of the effective dose determined in this study for patient examinations performed in a large number of hospitals and private practices using conventional SPECT and CT devices are compared in Table 3 with data obtained in two recent single-centre studies [28, 29] for patient examinations carried out using second-generation hybrid SPECT/CT systems. The results agree reasonably well taking into account the differences in study design and dosimetry (multi-centre evaluation of a large number of scans, solely diagnostic CTs, dosimetric concepts of ICRP Publication 103 versus single-centre evaluations of a limited number of scans, both low-dose and diagnostic CTs, dosimetric concepts of ICRP Publication 60).
The effective dose from a combined SPECT/CT examination is, of course, the sum of the effective doses arising from all scan components. According to the values given in Tables 1 and 2 for the effective dose associated with representative SPECT and CT examinations, respectively, diagnostic CT scans acquired as part of a combined SPECT/CT examination contribute considerably to, and for some applications even dominate, total patient exposure.
Assessment of radiation risks to patients in SPECT/CT
The effective dose is neither recommended for epidemiological evaluations nor should it be used for detailed specific retrospective investigations of individual radiation risks [10]. For the estimation of the potential consequences of a radiation exposure to individual patients, it is necessary to use specific data characterizing the exposed individual.
The standard approaches to generate age-, sex- and organ-specific risk estimates are based on excess relative risk (ERR) or excess absolute risk (EAR) models. The ERR model assumes that the excess risk is proportional to the baseline risk, i.e. the risk for a person to develop a specific cancer in the absence of radiation. The EAR model expresses the risk in terms of differences between the total risk and the baseline risk. Both approaches are used to model the organ-specific absolute rate ar T
that gives the total absolute risk of a person of sex s, after exposure to an absorbed organ dose D T , at age e, to develop cancer at age a. In these equations, r o,T , err T and ear T are the baseline rate, the excess relative rate and the excess absolute rate, respectively. For example, an err = 1 means that the additional, radiation-related cancer risk is as high as the normal cancer risk. Estimates of excess risk for specific organs are usually derived from cancer incidence data of the LSS, where linear dose dependence is commonly assumed for solid tumours, while a linear-quadratic approach provides better results for leukaemia. The most recent models are summarized in the BEIR VII report [6].
The organ-specific excess absolute lifetime risk or lifetime attributable risk, LAR, is calculated by summing up all ear T (e,a,s,D T ) values between e+Δt (with Δt being the minimum latency period) and the age of, e.g. 85 years, commonly used for lifetime risk estimates. The ear should be corrected for competing risks by the conditional probability P(e,a), i.e. the probability that a person of age e survives beyond the age a
with ear T = r o,T err T in the case of the ERR model. The minimum latency period Δt is the time during which radiation-induced cancer typically does not show clinical symptoms. A Δt of about 5 years for solid cancer and about 2 years for leukaemia is widely applied for incidence data. To determine the total LAR, all organ-specific LAR T estimates have to be summed up.
For many cancer sites, there are substantial differences in the baseline risks between Japanese and Western populations and, consequently, also between organ-specific risks estimated by an ERR or EAR model. The approach used in the present study to deal with this problem is described in detail in reference [30]. A detailed discussion of the uncertainties associated with the estimation of radiation risks can be found in recent reviews [7, 8].
Using the presented approach for risk estimation as well as German disease and life table data [31, 32], total LARs were estimated (with a dose and dose-rate effectiveness factor of 1) for the SPECT and CT examinations considered in detail in this paper based on organ doses calculated for representative values of the measurable dose-related quantities. The estimates are plotted in Figs. 1 and 2 for both sexes and different ages at exposure. The risk related to a specific SPECT/CT examination is the sum of the LARs determined for the separate SPECT and CT scan(s). As a general result, the figures reveal that the LAR decreases markedly for all examinations with increasing age at exposure and is—in particular at younger ages—markedly higher for women than for men (even though the differences in the plots may be overestimated to a small extent, since the risks were estimated using sex-averaged and not sex-adapted measurable dose-related quantities). The estimated risks can be compared with the lifetime baseline cancer risk, i.e. the ‘normal’ risk of developing cancer during the remaining lifetime from, e.g. from age 20 years. In Germany, the lifetime baseline cancer risk for all cancers (excluding skin cancer) is about 39 % for women and about 47 % for men [32].
Values of lifetime attributable risks (LAR) resulting from administration of some SPECT radiopharmaceuticals to adult male (left column) and female (right column) patients at different ages. 99mTc-labelled compounds (upper row): MIBI (800 MBq, rest), tetrofosmin (800 MBq, rest), bisphosphonates (600 MBq), MAA (160 MBq), technegas (400 MBq, 10 % lung uptake) and DTPA (950 MBq, 4 % lung uptake). Non-99mTc-labelled compounds (lower row): 111In-octreotide (170 MBq), 201Tl-chloride (75 MBq) and 123I-FP-CIT (180 MBq). Risks were estimated from absorbed organ doses computed for reference voxel phantoms using BEIR VII models as well as German life tables and cancer incidence rates. If the amount of activity administered to a patient is deviant from the value given above, the corresponding LAR can simply be derived by assuming a linear relationship between risk and activity
Lifetime attributable risks (LAR) for fully diagnostic single-phase CT examinations of the brain, chest, upper abdomen, abdomen and pelvis performed at different ages in adult male (left) and female (right) patients. Risks were estimated for the median CTDI vol and DLP values given in Table 2 using BEIR VII models as well as German life tables and cancer incidence rates
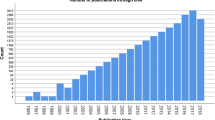
For different SPECT examinations frequently performed in Germany in routine clinical practice, the age distribution of the respective patients is characterized in Fig. 3. The plot reveals that between 53 % (parathyroid imaging using MIBI) and 70 % (lung ventilation studies using DTPA) of the patients are older than 60 years and thus run only a marginal risk of developing an examination-related cancer in their remaining life. The vast majority (78 %) of heart studies is performed in patients aged between 46 and 75 years. In patients with lung dysfunctions this percentage is markedly lower (61 %). SPECT examinations of the lungs are performed to a considerable fraction not only in older (24 %) but in particular also in younger (15 %) patients. The highest percentage of very young patients (16–30 years) occurs in cases of lung ventilation studies using technegas (6.4 %).
Age distribution of patients for 11 frequently performed nuclear medicine studies (cf. Table 1). Data were evaluated on the basis of nearly 140,000 procedures carried out in 48 hospitals and private practices in Germany in 2007/2008
The following two concrete examples demonstrate how the presented data are used to estimate radiation risks of combined SPECT/CT examinations:
-
A ventilation and perfusion (V/Q) SPECT using 99mTc-labelled technegas (400 MBq, 10 % lung uptake) and MAA (160 MBq), respectively, in combination with a diagnostic CT of the chest in a 25-year-old male/female patient with lung dysfunction yield a total effective dose of about 8.5 mSv and a total LAR of 0.10 %/0.24 %. This corresponds to 1 excess cancer in approximately 1,000/420 examined men/women.
-
Tumour imaging in a 65-year-old male/female patient with a suspected neuroendocrine tumour by means of 111In-labelled octreotide SPECT (170 MBq) and a diagnostic CT of the abdomen results in a total effective dose of 19.7 mSv and a total LAR of 0.15 %/0.20 %, which corresponds to 1 excess cancer in approximately 670/500 examined men/women.
In the given examples, the diagnostic CT scan contributes with 67 and 49 % to the total effective dose of the lung and cancer study, respectively. Whereas the total effective dose of the lung study is markedly lower compared to the tumour study, exposure results in a higher radiation risk to the young female patient, thus requiring a particularly strict medical justification (regarding the need for a CT scan in V/Q imaging see [33]).
Justification and optimization of SPECT/CT examinations
Generic and individual justification
A strong indication for the generic justification of SPECT/CT for various diagnostic issues is given by the growing number of studies demonstrating an added diagnostic benefit when using the hybrid imaging technology as compared to SPECT alone [34] and the usually acceptable (although not completely negligible) procedure-related radiation risk. Generally speaking, the possible spectrum of clinical indications for SPECT/CT—having a major impact on the age distribution of the patients and, in turn, on the examination-related radiation risk—is defined by the nuclear medicine imaging method. Nevertheless, questions remain regarding the broad applicability of SPECT/CT to all traditional SPECT applications [28]. It is, therefore, essential to carefully justify any individual SPECT/CT examination by considering the benefits and risks associated with adding CT to a SPECT scan.
Since there is no clinical indication for a SPECT/CT examination unless a SPECT scan has been indicated, the issue on justification comes basically down to the question of whether it is really necessary to additionally acquire a low-dose CT for anatomical localization of tracer uptake or even a fully diagnostic CT. In many cases, it may be sufficient to acquire a low-dose CT scan (E, 1–4 mSv depending on the axial field of view [34, 35]) as part of the combined SPECT/CT. This holds particularly true when a separate high-quality CT (or MRI) has been performed during the clinical work-up of the patient. By using a low-dose CT protocol, overall patient exposure is in most situations dominated by internal radiation from the emission scan and is—at least in cases of partial-body CTs—not extensively increased as compared to a conventional SPECT study. In this context it also has to be considered that (low-dose) CT data are necessary for attenuation and scatter correction of the acquired emission data, allowing superior quantification of radiotracer uptake. Nevertheless, any additional exposure has to be justified.
Generally, SPECT examinations should not be performed in pregnant women. In the rare instance that a SPECT examination is still clinically indicated, it is essential to keep activity as low as possible without compromising the image quality. If at all possible, a CT should not be added or at least limited to body regions far away from the shielded uterine region. In the case of a SPECT/CT examination performed in a female patient unknowingly pregnant, an individual risk assessment is mandatory. In situations involving the administration of radiopharmaceuticals to women who are lactating, an interruption of breastfeeding is advised for some of the SPECT tracers listed in Table 1 (99mTc-MAA and 99mTc-red blood cells, 12 h; 201Tl-chloride, 48 h; 123I-ioflupane, 3 weeks) [19].
Technique- and technology-related measures for dose reduction
There are a number of effective measures to optimize radiation protection of patients undergoing SPECT/CT examinations. With respect to an intended SPECT examination, the following technique-related aspects must be considered:
-
99mTc-Labelled radiopharmaceuticals should be preferred if available and clinically applicable due to the favourable physical properties of the radionuclide. Its physical half-life of about 6 h is sufficiently long to allow for the radiochemistry as well as for physiological uptake and distribution but short enough to limit radiation exposure after the study is completed.
-
When applying radiopharmaceuticals labelled with longer-lived gamma emitters, generally resulting in a higher effective dose to patients per unit of administered activity, h E, the activity injected in patients has to be reduced accepting a loss in image quality (noise, spatial resolution) and, as the case may be, a longer acquisition time.
-
The amount of activity administered has to be adjusted to the patient’s size, particularly in the case of children [36].
-
To reduce the biological half-life of an applied radiopharmaceutical, urinary or faecal excretion should be forced by oral hydration with water or, when indicated, by administration of a diuretic or laxative.
CT protocols need to be carefully tailored to the clinical situation to balance radiation exposure and diagnostic needs. The most important technique-specific strategies for dose reduction are [37–40]:
-
Limiting the body region to be scanned by CT to findings on the planar scintigram or tomographic emission images, in particular in follow-up studies. However, SPECT-guided CT requires that emission images can be reconstructed and analysed prior to the CT, which may not be possible with all SPECT/CT systems on the market [28, 29].
-
Using a pitch greater than 1 in cases of spiral CT scanning where it is clinically appropriate.
-
Acceptance of a higher noise level when using a narrow slice collimation. Detailed contrast of small lesions is enhanced with narrow slice collimation due to the reduction of partial volume effects in the axial direction, whereby the contrast to noise ratio is considerably improved even in the presence of an increased noise level.
-
Shielding of radiation-sensitive organs.
Optimization of SPECT/CT scans can be further facilitated by technology-related measures. Up to now, however, innovative SPECT system and image reconstruction technologies [41–43] have been put into clinical practice primarily to reduce the acquisition times, since fast imaging provides immediate benefits in terms of patient throughput and comfort [41]. But whenever clinically possible, technological advances should be used, at least in part, to reduce patient exposure by decreasing the tracer activity to be injected. All CT manufacturers have meanwhile developed systems for automatic exposure control, which allow reducing the dose to patients by between 20 and 50 % (depending on the imaged body region) without sacrificing image quality [44]. The principal idea of this approach is to adapt the tube current to the changing anatomy of the patient both in the transverse plane and axial direction. Further CT solutions are under development or clinical evaluation—such as adaptive collimation [45], scatter reduction, adaptive post-processing image filtration [46] and, most promising, iterative image reconstruction [47].
Diagnostic reference levels
In its publication on Radiological protection in medicine [12] the ICRP recommends the use of DRLs for patient examinations as a measure of optimization of radiation protection. As a form of investigation level, DRLs apply to dose-related quantities that can easily be measured (CT: CTDI vol and DLP; SPECT: A) and are intended for use as a simple test for evaluating whether patient exposure is unusually high for a particular imaging procedure. It should be noted that reference levels do not apply to individual patients but rather to the mean value of the measurable dose-related quantities determined in practice for a suitable reference group (comprising at least ten patients) to compensate for differences in body stature. If the measurable dose-related quantities associated with a specific procedure are consistently exceeding the corresponding DRL, the procedures and equipment should be subject to a local review (clinical audit). Actions aimed at the reduction of dose levels should be taken, if necessary.
According to the Guidance on diagnostic reference levels for medical exposures issued by the European Commission [48], DRLs are applied differently in diagnostic radiology and nuclear medicine. For nuclear medicine procedures, reference levels are ‘optimum’ values necessary to obtain the diagnostic information in standard situations based on the experience of professional groups. Nevertheless, practitioners are encouraged to reach the same good outcome using lower administered activities, e.g. by using new equipment with higher detection efficiency. For CT examinations, reference levels are defined on the basis of data from surveys performed in hospitals and private practices in a particular region or state. Generally, the third quartile of the mean dose levels evaluated in these facilities for a particular X-ray procedure becomes the corresponding reference level. It is expected that these levels are not exceeded on average and that the dose in standard situations is well below.
Specific DRLs for combined SPECT/CT examinations have not yet been established. Instead, national DRLs established for conventional SPECT and CT scans should be applied to the components of a combined SPECT/CT examination. The actual German reference levels for SPECT are close to the median activities given in Table 1 and for fully diagnostic single-phase CT to the third quartile of the DLP values given in Table 2. The fraction of the amount of a SPECT radiopharmaceutical to an adult to be administered in paediatrics can be calculated from the child’s body weight according to the dosage card published by the European Association of Nuclear Medicine [36]. Age- or weight-adapted DRLs have also been established in most states for relevant paediatric CT examinations.
Conclusion
Combined SPECT/CT studies entail increased radiation exposure and risk to patients compared to SPECT alone. It is, therefore, indispensable to balance the diagnostic needs and radiation protection requirements by applying the principles of justification and optimization. Since the choice of an appropriate examination technology and technique depends on the individual clinical situation, the diagnostic physician plays a pivotal role in the process of justification and optimization. In any case, SPECT/CT studies have to be optimized, e.g. by adapting dose reduction measures from state-of-the-art CT practice, and should for standard situations not exceed the national DRLs.
References
Beyer T, Freudenberg LS, Townsend DW, Czernin J. The future of hybrid imaging−part 1: hybrid imaging technologies and SPECT/CT. Insights Imaging 2011;2:161–9.
Beyer T, Townsend DW, Czernin J, Freudenberg LS. The future of hybrid imaging−part 2: PET/CT. Insights Imaging 2011;2:225–34.
Hicks RJ, Hofman MS. Is there still a role for SPECT-CT in oncology in the PET-CT era? Nat Rev Clin Oncol 2012;9:712–20.
Wieder H, Freudenberg LS, Czernin J, Navar BN, Isral I, Beyer T. Variations of clinical SPECT/CT operations: an international survey. Nuklearmedizin 2012;51:154–60.
Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res 2007;168:1–64.
Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. National Research Council. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. Washington: National Academies Press; 2006.
Shah DJ, Sachs RK, Wilson DJ. Radiation-induced cancer: a modern view. Br J Radiol 2012;85:e1166–73.
Durand DJ, Dixon RL, Morin RL. Utilization strategies for cumulative dose estimates: a review and rational assessment. J Am Coll Radiol 2012;9:480–5.
Hendee WR, O’Connor MK. Radiation risks of medical imaging: separating fact from fantasy. Radiology 2012;264:312–21.
ICRP. Publication 103. The 2007 recommendations of the International Commission on Radiological Protection. Ann ICRP 2007;37:2–4.
United Nations Scientific Committee on the Effects of Atomic Radiation. Report to the General Assembly, with scientific annexes. Volume I: effects of ionizing radiation. New York: United Nations; 2006.
ICRP. Publication 105. Radiological protection in medicine. Ann ICRP 2007;37:6.
IAEA. Radiation protection and safety of radiation sources: international basic safety standards. General safety requirements part 3. No. GSR part 3 (interim). Vienna: IAEA; 2011.
Council of the European Union. Council directive 97/43/Euratom of 30 June 1997 on health protection against the dangers of ionizing radiation in relation to medical exposure, and repealing directive 84/466/Euratom. Document 397L0043. Official Journal NO. L 180, 09/07/1997 pp. 0022 – 0027; 1997.
ICRP. Publication 60. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP 1991;21:1−3.
Nosske D, Mattsson S, Johansson L. Dosimetry in nuclear medicine diagnosis and therapy. In: Kaul A, editor. Medical radiological physics. Landold-Börnstein. New series, group VIII, vol 7A. Berlin: Springer; 2012. p. 4–1–4.59.
ICRP. Publication 53. Radiation dose to patients from radiopharmaceuticals. Ann ICRP 1988;18:1–4.
ICRP. Publication 80. Radiation dose to patients from radiopharmaceuticals. Addendum to ICRP Publication 53. Ann ICRP 1998;28:3
ICRP. Publication 106. Radiation dose to patients from radiopharmaceuticals. Addendum 3 to ICRP Publication 53. Ann ICRP 2008;38:1–2.
Brix G, Lechel U, Veit R, Truckenbrodt R, Stamm G, Coppenrath EM, et al. Assessment of a theoretical formalism for dose estimation in CT: an anthropomorphic phantom study. Eur Radiol 2004;14:1275–84.
Kalender WA, Schmidt B, Zankl M, Schmidt M. A PC program for estimating organ dose and effective dose values in computed tomography. Eur Radiol 1999;9:555–62.
Stamm G, Nagel HD. CT-Expo − ein neuartiges Programm zur Dosisevaluierung in der CT. Fortschr Rontgenstr 2002;174:1570–6.
Imaging Performance Assessment of CT-Scanners Group. ImPACT CT patient dosimetry calculator v. 1.0.3. http://www.impactscan.org. Accessed 14 Mar 2013.
Bongartz G, Golding SJ, Jurik AG, Leonardi M, van Persijn van Meerten E, Rodríguez R, Schneider K, Calzado A, Geleijns J, Jessen KA, Panzer W, Shrimpton PC, Tosi G. European guidelines for multislice computed tomography. 2004. http://www.msct.eu/CT_Quality_Criteria.htm. Accessed 14 Mar 2013.
Lechel U, Becker C, Langenfeld-Jäger G, Brix G. Dose reduction by automatic exposure control in multidetector computed tomography: comparison between measurement and calculation. Eur Radiol 2009;19:1027–34.
ICRP. Publication 89. International Commission on Radiological Protection. Basic anatomical and physiological data for use in radiological protection: reference values. Ann ICRP 2002;32:3/4
ICRP. Publication 110. Adult reference computational phantoms. Ann ICRP 2009;39:2.
Larkin AM, Serulle Y, Wagner S, Noz ME, Friedman K. Quantifying the increase in radiation exposure associated with SPECT/CT compared to SPECT alone for routine nuclear medicine examinations. Int J Mol Imaging 2011;2011:897202.
Sharma P, Sharma S, Ballal S, Bal C, Malhotra A, Kumar R. SPECT-CT in routine clinical practice: increase in patient radiation dose compared with SPECT alone. Nucl Med Commun 2012;33:926–32.
Brix G, Berton M, Nekolla E, Lechel U, Schegerer A, Süselbeck T, Fink C. Cumulative radiation exposure and cancer risk of patients with ischemic heart diseases from diagnostic and therapeutic imaging procedures. Eur J Radiol 2013. doi:10.1016/j.ejrad.2013.07.015.
Statistisches Bundesamt. Statistisches Jahrbuch 2010 für die Bundesrepublik Deutschland. Stuttgart: Metzler-Poeschel; 2011.
Krebs in Deutschland 2005/2006. Häufigkeiten und Trends. 7. Ausgabe. Berlin: Robert Koch-Institut und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e. V; 2010.
Roach PJ, Gradinscak DJ, Schembri GP, Bailey EA, Willowson KP, Bailey DL. SPECT/CT in V/Q scanning. Semin Nucl Med 2010;40:455–66.
Buck AK, Nekolla S, Zielger S, Beer A, Krause BJ, Herrmann K, et al. SPECT/CT. J Nucl Med 2008;49:1305–19.
Brix G, Lechel U, Glatting G, Ziegler SI, Münzing W, Müller SP, et al. Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J Nucl Med 2005;46:608–13.
Lassmann M, Biassoni L, Monsieurs M, Franzius C, Jacobs F, EANM Dosimetry and Paediatrics Committees. The new EANM paediatric dosage card. Eur J Nucl Med Mol Imaging 2007;34:796–8.
Nagel HD, Galanski M, Hidajat N, Maier W, Schmidt T. Radiation exposure in computed tomography–fundamentals, influencing parameters, dose assessment, optimisation, scanner data, terminology. 4th ed. Hamburg: CTB Publications; 2002.
Catalano C, Francone M, Ascarelli A, Mangia M, Iacucci I, Passariello R. Optimizing radiation dose and image quality. Eur Radiol 2007;17 Suppl 6:F26–32.
Zacharias C, Alessio AM, Otto RK, Iyer RS, Philips GS, Swanson JO, et al. Pediatric CT: strategies to lower radiation dose. AJR Am J Roentgenol 2013;200:950–6.
Kalra MK, Singh S, Thrall JH, Mahesh M. Pointers for optimizing radiation dose in abdominal CT protocols. J Am Coll Radiol 2011;8:731–4.
Slomka PJ, Dey D, Duvall WL, Henzlova MJ, Berman DS, Germano G. Advances in nuclear cardiac instrumentation with a view towards reduced radiation exposure. Curr Cardiol Rep 2012;14:208–16.
Zoccarato O. Innovative reconstruction algorithms in cardiac SPECT scintigraphy. Q J Nucl Med Mol Imaging 2012;56:230–46.
Jin M, Niu X, Qi W, Yang Y, Dey J, King MA, et al. 4D reconstruction for low-dose cardiac gated SPECT. Med Phys 2013;40:022501.
Gudjónsdóttir J, Ween B, Olsen DR. Optimal use of AEC in CT: a literature review. Radiol Technol 2010;81:309–17.
Deak PD, Langner O, Lell M, Kalender WA. Effects of adaptive section collimation on patient radiation dose in multisection spiral CT. Radiology 2009;252:140–7.
Leander P, Söderberg M, Fält T, Gunnarsson M, Albertsson I. Post-processing image filtration enabling dose reduction in standard abdominal CT. Radiat Prot Dosimetry 2010;139:180–5.
Beister M, Kolditz D, Kalender WA. Iterative reconstruction methods in X-ray CT. Phys Med 2012;28:94–108.
European Communities. Guidelines on diagnostic reference levels (DRLs) for medical exposures. Radiation protection 109; 1991.
Acknowledgment
The support of U. Lechel and A. Schegerer is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brix, G., Nekolla, E.A., Borowski, M. et al. Radiation risk and protection of patients in clinical SPECT/CT. Eur J Nucl Med Mol Imaging 41 (Suppl 1), 125–136 (2014). https://doi.org/10.1007/s00259-013-2543-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2543-3