Abstract
Objectives
This study evaluates the correlation between the bone end and soft tissue end of the quadriceps tendon–patellar bone autograft (QPA) size and pre-operative MRI measurements of the quadriceps tendon along sections to be included in the graft harvest in adolescents. We also assessed association between graft diameter and anthropometric measures (height, weight, and BMI), age, and sex.
Methods
Patients (10–18 years) who underwent QPA ACL reconstruction and had a pre-operative MRI were considered for inclusion. Age, height, and weight, tibial and femoral side graft diameter, and patellar bone block dimensions were collected. Using a pre-operative 2D sagittal plane MRI, we measured the quadriceps at 10-mm increments above the patella, up to 40 mm. We assessed correlation between the bone-end graft diameter and the AP measure at 10 mm above the patella, and correlation between the soft-tissue end graft diameter and the most proximal AP measure.
Results
A total of 103 patients were included. A significant correlation between the soft-tissue side graft diameter and most proximal AP measurement was observed (rs = 0.51; p < 0.001). However, measurements significantly underestimated the soft-tissue end graft diameter (9.6 ± 0.8 vs. 7.4 ± 1.1; p < 0.001). There was no correlation between the bone-end graft diameter and AP measurement 10 mm above the patella. Anthropometric measures were not associated with graft size. Skeletal maturity was associated with smaller graft size (p = 0.08).
Conclusion
Soft-tissue end graft diameter is associated with the AP measure of the quadriceps at 20–40 mm above the superior pole of the patella.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) tears are increasingly common among young people [1,2,3]. For young, active patients, ACL reconstruction (ACLR) is recommended soon after injury to prevent further chondral or meniscal damage [3, 4]. Thus, many physeal-respecting anatomic ACL reconstruction techniques using either a hamstring tendon or quadriceps tendon autograft have been developed [5,6,7]. Low failure rates, good patient-reported outcomes, and high return to sport rates have been associated with both graft types in adolescents and adults [6, 8,9,10,11,12]. Although superiority of hamstring or quadriceps tendon autograft has not been definitively determined, a benefit of choosing the quadriceps graft over a hamstring graft for young patients is the ease of harvesting a more reliably sufficient graft size [8, 10,11,12,13,14].
Small graft diameter (less than 8 mm) has been associated with hamstring tendon graft failure. Although the quadriceps tendon has been shown to yield a larger graft diameter compared to the hamstring tendon in young patients, pre-operative confirmation of adequate quadriceps tendon girth for graft harvest may still benefit surgeons and their patients [15,16,17,18,19]. Pre-operative planning for graft size may be particularly important prepubescent or small patients whose tendon girth is not yet well developed.
MRI-based and anthropometric measures (height, weight, BMI), as well as age and sex, have been correlated with both the quadriceps and hamstring autograft size among adults, although these techniques have not been assessed in young patients [14, 20,21,22,23]. Understanding predictive measures of graft size may in young patients will help providers determine the most appropriate graft choice for each case, especially when adequate tendon girth is in question. Thus, the purpose of our study is to assess the reliability of using an anterior–posterior (AP) measure of the quadriceps on a sagittal plane of a 2D MRI taken preoperatively to predict the harvested diameter of the quadriceps tendon–patellar bone autograft in adolescent patients. We hypothesized a strong correlation between MRI measurement and harvested graft size.
Methods
Patient selection and medical record review
After institutional review board approval, we reviewed a single provider’s surgical cases to identify all patients ages 10–18 who underwent ACL reconstruction in 2017. Patients who did not have a pre-operative MRI available in the medical records (n = 10), did not receive the QPA graft (n = 4), and had undergone a lower limb surgery on the involved limb (n = 6) were excluded. From the medical chart, we recorded sex, age, height, and weight, and body mass index at the time of surgery. From the pre-operative MRI, we determined skeletal maturity at the knee based on physeal status.
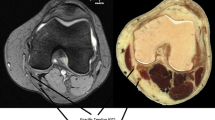
The QPA graft harvest and reconstruction has been described in detail [7]. In short, a 1 cm wide by 1.5 cm long by 1 cm deep trapezoidal bone block is cut from the patella and removed with a curved 3/8th inch osteotome. As the bone block is excised and elevated, a 10-mm-wide central section of the quadriceps tendon is separated from the remaining quadriceps fibers until the entire graft reaches 65 mm in length including the bone block. The graft is prepared, and the diameters of the soft-tissue and the bone-block ends are each measured to the nearest 0.5 mm. The intraoperative graft diameter measurements were completed with a sizing block and recorded as the smallest hole each end of the graft could fit through. Of note, the bone-end side of the graft was measured at the soft tissue immediately proximal to the bone block. The soft tissue diameter immediately proximal to the bone block does necessarily match the size of the bone block for each patient. After graft preparation, the patellar-bone block is seated into the femoral tunnel and the soft-tissue end is seated into the tibial tunnel.
Imaging review
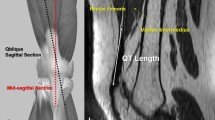
Two board-certified, pediatric musculoskeletal radiologists who were blinded to patient information, the operative report, and each other’s measurements, independently reviewed each 2D pre-operative MRI. The raters identified the sagittal image that showed the thickest portion of the quadriceps tendon and measured the anterior–posterior width of the quadriceps tendon at 10-mm increments, up to 40 mm as able based on the field-of-view, superior to the central aspect proximal pole of the patella (Fig. 1), as demonstrated previously by Zakko et al. Because the quadriceps autograft differs in diameter at the soft-tissue end (which becomes the tibial end of the neoligament) and the bone-end (which becomes the femoral end of the neoligament), the average measure at 10 mm superior to the patella was used to predict the bone-end diameter, and the average most proximal available measure was used to predict the soft-tissue end.
Statistical analysis
Continuous variables are presented as means (standard deviations), and categorical variables are presented as the number included and corresponding percentage. We analyzed the correlation between the two radiologist’s measurements for each mark (10, 20, 30, and 40 mm) using Pearson correlation coefficients. If these values were > 0.8, we elected to use the average measure between the two raters at each location.
We then examined the correlation between the bone-end graft diameter and the MRI-measured diameter 10 mm above the patella using a Spearman rho (rs) correlation coefficient, given the non-normal distribution of the ACL graft diameter. We performed the same correlation analysis between the soft-tissue end ACL graft diameter and the most proximal available MRI measurement (50% at 40 mm, 22% at 30 mm, 18% at 20 mm; 10% at 10 mm). In addition, we calculated the individual differences between the harvested graft diameter at both the bone-end and soft-tissue end and the predicted diameter based on MRI on each end of the graft. We classified the accuracy of the MRI measurement (defined as within 1 mm of the harvested graft diameter).
Finally, in order to assess the demographic and anthropometric predictors (height, weight, and BMI) of the harvested soft-tissue end graft diameter, we constructed a multivariable regression model. All statistical tests were two-sided and performed using Stata Statistical Software: Version 15 (College Station, TX: StataCorp, LLC).
Results
A total of n = 122 patients were considered for inclusion in our analysis. We removed n = 20 (n = 10 with no preoperative MRI available, n = 6 who had a previous surgery to the involved limb, n = 4 who had a non-QPA graft). There were no significant differences between those who were included and excluded in the proportion of females (55% vs. 31%; p = 0.11), proportion of skeletally mature patients (73% vs. 45%; p = 0.08), or in the mean age (15.9 ± 1.9 vs. 15.1 ± 4.4 years; p = 0.18). Thus, our analyzed sample included n = 102 patients. Among those included in the sample, the average time between the MRI and ACLR surgery was 44 days (95% confidence interval: 32–56 days). Age at surgery, anthropometric data, and surgical information is presented in Table 1.
The inter-rater correlation for the MRI measurements of the quadriceps completed by the two radiologists was high at 10 mm (r = 0.82), 20 mm (r = 0.87), 30 mm (r = 0.88), and 40 mm (r = 0.88) proximal to the superior pole of the patella. Thus, when comparing MRI measurements to the harvested graft diameter, we used the average of each radiologist’s measurement at each level.
The correlation between the bone-end graft diameter and the MRI AP measure (mm) of the quadriceps at 10 mm above patella was weak and non-significant (Fig. 2; rs = − 0.03; p = 0.76). The MRI diameter significantly underestimated bone-end graft diameter (7.3 ± 1.1 mm vs. 10.6 ± 0.3 mm; p < 0.001). The correlation between the soft-tissue side graft diameter and the MRI-predicted graft diameter at the most proximal available measurement above the patella was strong and significant (Fig. 3; rs = 0.51; p < 0.001). As with the bone-end, however, the MRI measurement significantly underestimated the harvested soft-tissue graft diameter (7.4 ± 1.1 vs. 9.6 ± 0.8; p < 0.001).
On the bone-end of the graft, the difference between the harvested graft diameter and MRI measurement was 3.3 ± 1.2 mm, while the difference on the soft-tissue end was 2.2 ± 1.0 mm. Defining an accurate MRI measurement as within 1 mm of the true graft size, the MRI was accurate 5% of the time on the bone-end, and 11% of the time on the soft-tissue end.
The multivariable regression model indicated that skeletal maturity was significantly associated with a smaller soft-tissue end graft diameter, but that no other demographic characteristics were significantly associated with tibial side graft diameter (Table 2).
Discussion
The results from our investigation indicate a moderately strong, significant linear correlation between the soft-tissue side graft diameter and the MRI-measured graft diameter at the most superior measurement above the patella, although the MRI underestimated the graft size. Our technique for estimating the soft-tissue end graft diameter significantly underestimated the harvested diameter by about 2.2 mm. This inaccuracy is favored to reflect the inherent limitation of a single 2-dimensional AP measurement to estimate size of the 3-dimensional autograft, without the ability to measure cross-sectional area. Measurements of a three-dimensional MRI may yield a more accurate representation of the autograft thickness by accounting for the radial quadriceps tendon thickness [14]. As well, the consistency of the surgical technique for harvesting a 10 mm wide by 10 mm deep by 15 mm long bone plug and elevating the bone block with attached fibers likely dictates the bone-end graft size. This surgical technique explains the lack of correlation and inaccuracy of the MRI measured quadriceps thickness at 10 mm above the patella and the actual harvested bone-end diameter. The morphology of the quadriceps tendon is variable from patient to patient, creating difficulty to account for the linearity of the tendon fibers on MRI. Interestingly, Zakko et al. [20] accurately predicted quadriceps graft size with a similar technique using the average of quadriceps thickness measurements from a sagittal view at 10 mm, 20 mm, and 30 mm. Furthermore, the quadriceps autograft predicted in Zakko et al. [20] was not specified as a free graft or with an attached bone plug, which may explain differences in the results of our studies.
A limitation of this study includes the use of 2-dimensional MRI as mentioned above, which does not allow volumetric reconstruction of image planes aligned with the quadriceps tendon axis. While both the high inter-rater agreement and strong correlation of the graft soft tissue end with the most proximal quadriceps tendon measurement are promising for the value of MRI measures, the accuracy may be improved by using 3-dimensional image data in order to perform more robust area measurements of the tendon and therefore account for the radial thickness of the autograft [14].
Other studies have identified anthropometric measures that are correlated with quadriceps tendon graft size [20, 24]. Both Xerogeanes et al. [24] and Zakko et al. [20] found height to be a strong predictor of quadriceps tendon graft thickness in adults. Height, weight, and BMI were not associated with graft thickness in our cohort of adolescent patients. However, skeletal maturity was a predictor of smaller soft-tissue end tendon size, which was unexpected considering the normal hypertrophy of muscle girth that most often accompanies the onset of puberty. It is possible this finding among our cohort would become nonsignificant with a larger sample size. As well, the normal distribution of soft-tissue tendon size overlaps considerably between the skeletally mature and skeletally immature patients included in the analysis, and we do not feel this statistically significant finding bears clinical significance as well.
Conclusion
Pre-operative planning for expected diameter at the soft-tissue end quadriceps tendon–patellar bone autograft may help providers determine if an increased width of graft harvested is needed to be obtained for small patients when tendon girth is in question. Our method of measuring the pre-operative MRI did not directly yield an accurate measurement without adjustment. For this technique, consideration of adjusting the most superior available AP MRI measurement of the quadriceps tendon by approximately 2 mm may help to predict the soft-tissue end diameter of the QPA graft in young patients. Future research is necessary to determine the minimal quadriceps tendon–patellar bone graft diameter associated with low failure rates.
References
Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–24.
Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 Through 2014. JAMA Pediatr. 2017;171(8):808–10.
Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL Tears in school-aged children and adolescents over 20 years. Pediatrics. 2017; 139(3).
Newman JT, Carry PM, Terhune EB, Spruiell MD, Heare A, Mayo M, et al. Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med. 2015;43(2):282–8.
Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. A preliminary report. J Bone Joint Surg Am. 2003;85(7):1255–63.
Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89(12):2632–9.
Albright J, Lepon AK, Mayer S. Anterior cruciate ligament reconstruction in pediatric and adolescent patients using quadriceps tendon autograft. Sports Med Arthrosc Rev. 2016;24(4):159–69.
Lind M, Strauss MJ, Nielsen T, Engebretsen L. Quadriceps tendon autograft for anterior cruciate ligament reconstruction is associated with high revision rates: results from the Danish Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2019.
Lund B, Nielsen T, Fauno P, Christiansen SE, Lind M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy. 2014;30(5):593–8.
Gagliardi AG, Carry PM, Parikh HB, Albright JC. Outcomes of quadriceps tendon with patellar bone block anterior cruciate ligament reconstruction in adolescent patients with a minimum 2-year follow-up. Am J Sports Med. 2019:363546519885371.
Cavaignac E, Coulin B, Tscholl P, Nik MohdFatmy N, Duthon V, Menetrey J. Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med. 2017;45(6):1326–32.
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gfoller P, et al. There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):605–14.
Charlton WP, Randolph DA Jr, Lemos S, Shields CL Jr. Clinical outcome of anterior cruciate ligament reconstruction with quadrupled hamstring tendon graft and bioabsorbable interference screw fixation. Am J Sports Med. 2003;31(4):518–21.
Ashford WB, Kelly TH, Chapin RW, Xerogeanes JW, Slone HS. Predicted quadriceps vs. quadrupled hamstring tendon graft size using 3-dimensional MRI. Knee. 2018;25(6):1100–6.
Park SY, Oh H, Park S, Lee JH, Lee SH, Yoon KH. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1111–8.
Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34(12):1933–40.
Maeda A, Shino K, Horibe S, Nakata K, Buccafusca G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am J Sports Med. 1996;24(4):504–9.
Mariscalco MW, Flanigan DC, Mitchell J, Pedroza AD, Jones MH, Andrish JT, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013;29(12):1948–53.
Urchek R, Karas S. Biomechanical comparison of quadriceps and 6-strand hamstring tendon grafts in anterior cruciate ligament reconstruction. Orthop J Sports Med. 2019;7(10):2325967119879113.
Zakko P, van Eck CF, Guenther D, Irrgang JJ, Fu FH. Can we predict the size of frequently used autografts in ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3704–10.
Leiter J, Elkurbo M, McRae S, Chiu J, Froese W, MacDonald P. Using pre-operative MRI to predict intraoperative hamstring graft size for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):229–35.
Ho SW, Tan TJ, Lee KT. Role of anthropometric data in the prediction of 4-stranded hamstring graft size in anterior cruciate ligament reconstruction. Acta Orthop Belg. 2016;82(1):72–7.
Mardani-Kivi M, Karimi-Mobarakeh M, Mirbolook A, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K, et al. Predicting the hamstring tendon diameter using anthropometric parameters. Arch Bone Jt Surg. 2016;4(4):314–7.
Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE. Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med. 2013;41(10):2392–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Albright is a consultant and speaker for Arthrex Inc. and Gemini Mountain Medical LLC. Unrelated to this study, Dr. Howell has received research support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R03HD094560), the National Institute of Neurological Disorders And Stroke (R01NS100952, R03HD094560, and R43NS108823), and MINDSOURCE Brain Injury Network.
All other authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gagliardi, A.G., Howell, D.R., Stein, J.M. et al. Prediction of quadriceps tendon–patellar bone autograft diameter in adolescents with 2-dimensional magnetic resonance imaging and anthropometric measures. Skeletal Radiol 51, 619–623 (2022). https://doi.org/10.1007/s00256-021-03874-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03874-w