Abstract
Purpose
Graft choice for anterior cruciate ligament (ACL) reconstruction is crucial, however the optimal graft source remains a topic of controversy. The purpose of this study is to compare subjective and functional patient-reported outcomes (PRO) after single-bundle ACL reconstruction using quadriceps tendon (QT) or hamstring tendon (HT) autografts for single-bundle ACL reconstruction. We hypothesize that there is no difference in patient-reported functional outcomes after ACL reconstruction using either HT- or QT autograft.
Methods
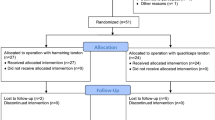
All data were extracted from a prospectively collected ACL registry. A total of 80 patients with at least 2-year follow-up were included in this study. A total of 40 patients with primary ACL reconstruction using a QT autograft harvested via a minimally invasive technique were matched by sex, age and pre-injury Tegner and Lysholm score to 40 patients who received HT autografts. Subjective and functional PRO scores including Lysholm score, Tegner activity level and visual analogue scale for pain were obtained at 6, 12 and 24 months after index surgery.
Results
No significant difference between the QT and the HT group was seen at any follow-up in regard to any of the PRO scores for function or pain. 24 months post-surgery the mean Tegner activity score of the HT group was significantly (p = 0.04) lower compared to the pre-injury status. At final follow-up, 27 patients (67.5%) in the QT group and 32 patients (80.0%) in the HT returned to their pre-injury activity level (n.s.). A total of 37 patients (92.5%) of the QT cohort and 35 patients (87.5%) of the HT cohort reported “good” or “excellent” results according to the Lysholm score (n.s.). “No pain” or “slight pain” during severe exertion was reported by 33 patients (82.5%) with QT autograft and 28 patients (82.4%) with HT autograft (n.s.).
Conclusion
There is no significant difference between PRO 2 years post-operative using either QT or HT autografts. Both QT and HT grafts show acceptable and comparable PRO scores making the QT a reliable graft alternative to HT for primary ACL reconstruction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Graft choice for anterior cruciate ligament (ACL) reconstruction is crucial, but the optimal graft source remains a topic of controversy. Besides good anatomical and biomechanical graft properties, surgeons demand grafts with an easy harvest procedure, low donor site morbidity, and early graft–bone integration [4, 42]. Autografts are the first choice in ACL surgery, with bone–patellar tendon–bone (BPTB) grafts and hamstring tendon (HT) grafts being the most popular [10, 46]. Currently, the perfect graft for ACL reconstruction does not exist with all grafts having advantages and disadvantages.
HT grafts have good biomechanical qualities, are easy to harvest, show excellent clinical outcomes and are therefore among the most widely used grafts for ACL reconstruction [31]. Recognized disadvantages are slower graft incorporation due to ligament to bone healing and an elevated risk of tunnel widening [4, 25, 38]. Reduced knee flexor strength with weakening of ACL agonists and an increased post-operative knee laxity are further potential drawbacks [15, 20, 34]. Moreover, the preoperative prediction of the size and length of the graft is still challenging [42].
Recently the quadriceps tendon (QT) autograft has presented itself as a potential graft alternative. Previous studies have demonstrated good anatomic and biomechanical characteristics of the QT graft regarding ultimate load to failure, stiffness, graft length and size [14, 37, 46, 47, 50, 51]. Further benefits include low donor site morbidity, reduced post-operative pain and analgesic consumption, and the preservation of the HT anatomy and its function as an ACL agonist [3, 7, 8]. Clinical outcomes comparing BPTB to QT grafts with respect to donor site morbidity show favourable results for the latter [5, 7, 8, 13, 22, 26, 29, 46, 47].
While there is an abundance of literature on ACL reconstruction analysing BPTB and HT grafts, to the best of our knowledge, this is the first study to compare minimally invasive harvested QT autograft and single-bundle HT autograft for primary ACL reconstruction. The purpose of this matched-pair analysis was to compare patient-reported functional outcomes after ACL reconstruction using QT- and HT autografts for single-bundle ACL reconstruction. It was hypothesized that there is no significant difference in patient-reported functional outcomes after ACL reconstruction using either HT- or QT single-bundle autografts.
Materials and methods
All data were extracted from a prospectively collected ACL registry. Between 2010 and 2014, 40 patients with primary ACL reconstruction using QT autograft met the inclusion criteria and were included in the study. This cohort was matched with respect to sex, age, pre-injury Tegner and Lysholm score to 40 patients with primary ACL injuries who were treated concurrently with single-bundle HT autografts. Informed consent was obtained from each patient prior to inclusion in the study. Subjective and functional outcomes from all patients were obtained at 6, 12 and 24 months after index surgery. Preoperative magnetic resonance imaging (MRI) was used to confirm ACL rupture. Plain radiographs (antero-posterior and lateral view) were used preoperatively to exclude any bone injury and severe osteoarthritis according to the Kellgren–Lawrence scale. Post-operative radiographs were used to assess the correct placement of the femoral button and to evaluate the direction of the femoral and tibial bone tunnel. Strict inclusion and exclusion criteria were applied to create a homogeneous study population and minimize the effect of potentially confounding variables (Table 1).
Surgical techniques
All ACL reconstructions were performed under general anaesthesia by three experienced orthopaedic surgeons familiar with both surgical techniques. Apart from the harvesting technique, the surgical procedure was identical for both graft choices.
Harvest of the QT
The minimally invasive harvesting technique of the quadriceps tendon has been described previously in detail [7]. Briefly a small 2–3-cm transverse skin incision was made over the proximal patellar boarder and the QT was exposed (Fig. 1a). With a 10–12-mm-wide double knife (Fig. 1b), a tendon separator (Fig. 1c, d) and a special tendon cutter (Fig. 1e) (Karl Storz, Tuttlingen, Germany) an approximately 6-cm-long, 10–12-mm-wide and 5-mm-thick tendon strip was harvested from of the central part of the quadriceps tendon. With an oscillating saw and a chisel, a rectangular-shaped bone block—approximately 1.5–2 cm long and as wide as the tendon graft—was created. After graft preparation, the bone block is fixed to a flip button device (e.g. EndoButton™ [Smith&Nephew, Andover, USA]) by strong non-absorbable sutures (No. 2 FiberWire [Arthrex, Naples, USA]) (Fig. 2a). Finally the tendon defect was closed with Vicryl sutures.
Minimally invasive QT harvest technique: a a 2–3-cm transverse incision is made over the superior boarder of the patella and the surface of the QT is exposed. b Subcutaneous advancement of the tendon knife (Karl Storz, Tuttlingen, Germany). The cutting edges are spaced at the desired graft width (10–12 mm). c Insertion and advancement of the 5-mm tendon separator (Karl Storz, Tuttlingen, Germany). d Subcutaneous advancement of the quadriceps tendon cutter (Karl Storz, Tuttlingen, Germany)
a QT graft with an approximately 20-mm-long rectangular bone block. Proximal fixation with 2.0 fibre wire sutures (Arthrex, Naples, USA) looped through and a Fliptak (Karl Storz, Tuttlingen, Germany). b Four-strand semitendinosus graft. Proximal fixation with an Endobutton CL (Smith&Nephew, Andover, USA)
Harvest of the HT
The ST was harvested in a standard manner through an antero-medial tibial portal, armed using whip-stich sutures (No. 2 FiberWire [Arthrex, Naples, USA]) and quadrupled over a continuous loop EndoButton™ (Smith&Nephew, Andover, USA) (Fig. 2b).
ACL reconstruction technique
After routine diagnostic arthroscopy, the ACL remnants were removed while preserving the tibial and femoral footprints. The femoral bone socket was drilled via an antero-medial portal with the tunnel size equal to the graft diameter (7–9 mm). The tibial bone tunnel was then positioned within the native ACL footprint with the drill guide set at 55° [48]. The graft was inserted retrograde via the tibial tunnel and fixed in the femoral socket using the respective flip button device. On the tibial site a hybrid fixation with a resorbable interference screw matching the size of the bone tunnel was used. The sutures were then tied over either a cortical bone bridge (HS) or an Endotack® (Karl Storz, Tuttlingen, Germany) (QT).
Rehabilitation
Post-operatively, both groups followed a similar rehabilitation programme focusing on reduction of pain, inflammation and swelling as well as early full extension. A knee brace limiting flexion up to 90° was used starting with the first post-operative day, and partial weight bearing was allowed immediately after surgery with crutches used for at least 2 weeks. Thereafter, full weight bearing and unrestricted range of motion was allowed. After a 2-day inpatient stay, patients attended outpatient physical therapy 2–3 times per week for at least 8–12 weeks.
Clinical evaluation
All patients were examined preoperatively and post-operatively at 6, 12 and 24 months. Lysholm score, Tegner activity level and visual analogue scale for pain (VAS) were answered separately and independently by the patient before surgery and at each time of follow-up. If a patient was dismissed prior to 24 month of follow-up and unavailable for personal post-operative examination, outcome information was obtained via mail service. Non-responders were followed by personal phone contact.
Statistical analysis
All data were analysed using SPSS v.22 (IBM Corp.). For continuous and normal distributed data, the Student’s T test was applied to determine differences between both groups. For ordinal or non-normally distributed data, the Mann–Whitney U test was used. Related pre- and post-operative data were compared using the Wilcoxon signed-rank test. A Pearson Chi-square test was performed to compare dichotomous variables. Significance level was set to 0.05 (two-sided) with 95% confidence intervals (CI). Sample size was calculated using G-Power 3.1.9.2 (Paul Franz, Kiel, Germany) using the repeated measure ANOVA as main analysis. This study included a total of 80 patients. The estimated total sample size was 82 with an effect size (f) of 0.25, alpha level of 0.05, a target power of 0.80, with two one between-subject factor (group) on two levels and one within factor (time) on four levels, and assuming a correlation between measures of 0.5.
Results
Patient demographics
Patient demographics and concomitant injuries are presented in Table 2. ACL rupture was confirmed by radiology in all patients. Patients had neither major bony injuries nor a Kellgren–Lawrence score greater than grade II. At 24 months, 72 patients (90%) were available for final follow-up.
Patient-reported outcomes
Complete results of the Lysholm score are presented in Table 3. No significant difference in Lysholm score between the QT and the HT group was seen at any time. No statistical difference was observed within the groups 2 years after surgery (n.s.). At final follow-up, 37 patients (92.5%) with QT autograft and 35 patients (87.5%) in the HT group reported “good” or “excellent” results.
VAS scores for subjective outcome and pain interpretation are presented in Table 4. No significant differences between QT autografts and HT autografts were determined at any follow-up visit. The mean VAS score for pain at final follow-up was 0.6 ± 1 for the QT cohort and 0.8 ± 1.2 for the HT cohort. At 24 months after index surgery, 33 patients (82.5%) with QT autograft and 28 patients (82.4%) with HT autografts reported no or only slight pain during severe exertion showing no significant difference (Table 5).
While stair climbing, 39 patients (97.5%) with QT grafts and 33 patients (97.1%) with HT graft reported no difficulties at 24 months after ACL reconstruction.
Activity level
Complete results of the Tegner activity level score are presented in Table 6. No significant differences between the groups were seen at any follow-up. At 24 months post-surgery, the Tegner activity score of the HT group was significantly lower (p = 0.04) compared to the pre-injury status, while no statistical difference was detected in the QT group (n.s.).
Regarding functional outcomes, 27 patients (67.5%) in the QT group and 32 patients (80.0%) in the HT group returned to their pre-injury Tegner activity level at final follow-up. There was no statistical difference between both groups (n.s.).
Graft rupture and donor site morbidity
Throughout the 2 years of follow-up, one graft rupture occurred in the HT group, while no re-ruptures were registered in the QT group (n.s.). The re-rupture occurred as a result of player contact while playing soccer. During the QT graft harvest process, no joint capsule opening or patellar fracture was observed. Post-operatively no major quadriceps bleeding or haematoma were reported or noted. None of the QT patients reported tenderness, numbness or irritation over the graft harvest site.
Discussion
This study demonstrates that QT autografts and single-bundle HT autografts show comparable patient-reported functional outcomes 2 years following primary ACL reconstruction.
Until now QT autografts have been used mainly in revision ACL surgery [36]. Lately, however, the quadriceps tendon (QT) autograft is receiving more attention for the use in primary ACL surgery for its potential advantages, especially in areas where traditional grafts show weaknesses [7, 13].
Numerous studies attribute good anatomical and biomechanical characteristics to the QT graft, with graft length, graft thickness and graft volume comparable to BPTB and HT autografts. Stäubli et al. [49] reported a mean cross-sectional area of 64.4 ± 8.4 mm2 of a 10-mm-wide, full-thickness quadriceps tendon, which is significantly greater than the cross-sectional area of the patellar tendon (36.8 ± 5.7 mm2) or a quadrupled hamstring tendon strand (52.9 ± 5.3 mm2) [12]. It has been shown that a large cross-sectional area is desirable to reduce the bungee and windshield effect as well as the tunnel–graft mismatch, which is believed to cause inflow of synovial fluid and cytokines with subsequent bone resorption and tunnel widening [13, 39]. Moreover, the QT is significantly longer (87.0 ± 9.7 vs. 51.6 ± 6.9) and has a larger bony attachment area and a significantly higher ultimate tensile failure load compared to an unconditioned patellar tendon (2.173 ± 618 vs. 1953 ± 325 N).
In the present study, a partial-thickness (5 mm) quadriceps tendon with rectangular-shaped bone block was harvested. ACL grafts with a bone block offer the advantage of bone-to-bone healing, which is believed to offer a faster and better osteointegration compared to ligament-bone healing and is widely accepted as the strongest form of healing in ACL reconstruction surgery [11]. Moreover, a biomechanical study performed by Herbort et al. [16] demonstrated that ACL reconstruction using a QT graft with an rectangular bone block and rectangular femoral bone tunnel results in significant lower anterior tibial translation in low knee flexion angles compared to a HT graft using a round femoral bone tunnel. They postulated that due to a lager insertion side of the rectangular-shaped QT graft, the postero-lateral fibres of the ACL and therefore the knee stability near extension would be restored more than by an HT graft using a round femoral bone tunnel [15, 16, 30].
While there is an abundance of literature comparing BPTB and HT autografts as well as BPTB and QT autografts, little is known about the relation between QT and HT autografts [6, 18, 28, 35]. A biomechanical study comparing ACL reconstruction techniques using QT and HT autografts showed no significant differences between the two grafts with respect to both anterior tibial translation (0° and 30° of knee flexion) nor in internal tibial rotation [43]. Both autografts restored knee function to the preoperative level and could produce similar in situ forces compared to the native ACL [43].
Without any doubt, anatomical, histological and biomechanical data are necessary. However, post-operative functional and clinical outcomes as well as patient satisfaction should be the main criteria when measuring the success of ACL reconstruction [40]. Despite this fact, clinical and functional outcomes after ACL reconstruction comparing QT autografts to HT autografts are rare.
Recently, Lee et al. [25] demonstrated similar clinical and functional post-operative results with favourable muscle strength recovery for the QT when compared to the HT. Hereby no difference in extensor muscle strength but significant less flexor muscle strength was observed in the HT group as compared to the QT group [25]. Chen et al. [4] reported a mean Lysholm score of 93 ± 7.9 4–7 years after ACL reconstruction using QT autograft. Kim et al. [22] described mean score values of 92.4 2 years after surgery, with no statistical differences between the QT and the BPTB groups. Other authors published Lysholm scores ranging from 70.7 to 94.0 in ACL reconstructions using QT autografts [9, 13, 23, 26, 27, 44, 47] while score values for patients with HT autografts were similar ranging between 80 and 94 [19, 21, 28, 31, 41, 42]. Despite these studies, different study methods and harvesting techniques, variable injury-to-operation intervals as well as different operation methods and rehabilitation protocols hinder the comparability among these studies.
In the present study, a median Lysholm score of 95 was obtained at final follow-up for the QT- and the HT autograft. These values are consistent with previous findings reported above and represent normal Lysholm scores for patients over 18 years with uninjured knees [2]. No significant difference was seen between the QT and HT groups at any follow-up.
Adding the Tegner activity scale to the Lysholm score is recommended and has shown good responsiveness to evaluate patients’ ability to participate in work and sports after ACL reconstruction [1]. Long-term prospective randomized studies comparing BPTB and HT autografts found no significant differences in the Tegner score [28, 32, 33]. The present study shows comparable findings regarding the QT and HT grafts with no statistical difference between the groups. Although a statistically significant difference between the preoperative and 24-month post-operative states was outlined, the mean difference of 0.3 in the Tegner activity score within the HT group may be clinically insignificant might not be clinically or attributable to a natural decline in physical performance.
Sport activity is often limited due to post-operative anterior knee or other donor site morbidities [28, 29, 41, 42, 52]. Anterior knee pain ranges from 25 to 48% in patients with BPTB autografts and from 6.6 to 20% in patients with HT autografts [8, 19, 41, 45, 52]. It is reported that patients with QT autografts suffer less from anterior knee pain and donor site morbidity compared to patients with BPTB graft [8, 22]. Geib et al. [8] showed a 26.7% incidence in the BPTB autograft group compared to only 4.6% incidence in the QT autograft group. Lee et al. [27] reported that 88% of the patients with QT autograft had minimal or no symptoms by participating in strenuous activities. Moreover, pain and analgesic consumption in the immediate post-operative period is less in patients with QT autografts compared to patients with HT autografts [3].
In the present study, 82.1% of the patients with QT autograft reported no or only slight symptoms during severe exertion. None of the patients complained about post-operative tenderness, numbness or irritation over the graft harvest site. Thanks to special designed harvesting knifes, a partial-thickness QT graft could be harvested with great accuracy and no intraoperative joint opening or post-operative haematoma was registered. Furthermore, the minimal invasive QT graft harvest technique showed favourable outcomes in terms of wound and skin cosmetics compared to the conventional harvesting technique.
By reviewing the current literature, it is clear that no perfect graft exists for ACL reconstruction. This increases the importance of surgeons’ familiarity with different graft choices to provide appropriate treatment for each patient [13]. The present study shows that patient with QT autografts have good patient-reported functional and clinical outcomes and low donor site morbidity 2 years after primary ACL. This suggests a role for QT as a reliable alternative to traditional grafts.
Some limitations apply to the present study. First, patient-reported data always carry a risk for potential bias or misunderstanding of the questionnaire. Nonetheless, all questionnaires used in this study were previously validated for psychometric parameters and good responsiveness in reporting functional outcome after ACL reconstruction [1]. Furthermore, all patients were briefed and instructed prior of the compilation of the first questionnaire to ensure all questions were understood. Second, this study focuses only on patient-reported functional and clinical data. While objective data and clinical measurements (e.g. arthrometers) would be favourable and are surely important, it has been shown that patient-derived assessment of symptoms and function is as important and often more robust than clinical measurements when evaluating outcomes after ACL reconstruction [17, 24]. Third, while all patients underwent radiological imaging before surgery, imaging by MRI was not performed after surgery.
Conclusion
It can be concluded that there is no significant difference between patient-reported outcomes 2 years post-operatively using either QT or HT autografts. Both QT and HT autografts show good and comparable patient-reported functional outcomes, making the quadriceps tendon a reliable graft alternative to hamstring tendons even for primary ACL reconstruction.
References
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37(5):890–897
Briggs KK, Steadman JR, Hay CJ, Hines SL (2009) Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med 37(5):898–901
Buescu CT, Onutu AH, Lucaciu DO, Todor A (2017) Pain level after ACL reconstruction: a comparative study between free quadriceps tendon and hamstring tendons autografts. Acta Orthop Traumatol Turc. doi:10.1016/j.aott.2017.02.011
Chen CH, Chuang TY, Wang KC, Chen WJ, Shih CH (2006) Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: clinical outcome in 4–7 years. Knee Surg Sports Traumatol Arthrosc 14(11):1077–1085
DeAngelis JP, Fulkerson JP (2007) Quadriceps tendon—a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 26(4):587–596
Eriksson K, Anderberg P, Hamberg P, Lofgren AC, Bredenberg M, Westman I, Wredmark T (2001) A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 83(3):348–354
Fink C, Herbort M, Abermann E, Hoser C (2014) Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech 3(4):e509–e513
Geib TM, Shelton WR, Phelps RA, Clark L (2009) Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy 25(12):1408–1414
Gorschewsky O, Klakow A, Putz A, Mahn H, Neumann W (2007) Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 15(11):1284–1292
Group M, Group M (2014) Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med 42(10):2301–2310
Gulotta LV, Rodeo SA (2007) Biology of autograft and allograft healing in anterior cruciate ligament reconstruction. Clin Sports Med 26(4):509–524
Hamner DL, Brown CH Jr, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81(4):549–557
Han HS, Seong SC, Lee S, Lee MC (2008) Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res 466(1):198–204
Harris NL, Smith DA, Lamoreaux L, Purnell M (1997) Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biomechanical evaluation. Am J Sports Med 25(1):23–28
Herbort M, Michel P, Raschke MJ, Vogel N, Schulze M, Zoll A, Fink C, Petersen W, Domnick C (2016) Should the ipsilateral hamstrings be used for anterior cruciate ligament reconstruction in the case of medial collateral ligament insufficiency? Am J Sports Med 10(1177/0363546516677728):363546516677728
Herbort M, Tecklenburg K, Zantop T, Raschke MJ, Hoser C, Schulze M, Petersen W, Fink C (2013) Single-bundle anterior cruciate ligament reconstruction: a biomechanical cadaveric study of a rectangular quadriceps and bone–patellar tendon–bone graft configuration versus a round hamstring graft. Arthroscopy 29(12):1981–1990
Herrington L (2013) Functional outcome from anterior cruciate ligament surgery: a review. OA Orthop 1(2):1–12
Holm I, Oiestad BE, Risberg MA, Aune AK (2010) No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon–bone autograft: a randomized study with 10-year follow-up. Am J Sports Med 38(3):448–454
Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA (2005) Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy 21(4):412–417
Imran A, O’Connor JJ (1998) Control of knee stability after ACL injury or repair: interaction between hamstrings contraction and tibial translation. Clin Biomech (Bristol, Avon) 13(3):153–162
Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI (2007) A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med 35(5):729–739
Kim SJ, Kumar P, Oh KS (2009) Anterior cruciate ligament reconstruction: autogenous quadriceps tendon–bone compared with bone–patellar tendon–bone grafts at 2-year follow-up. Arthroscopy 25(2):137–144
Kim SJ, Lee SK, Choi CH, Kim SH, Kim SH, Jung M (2014) Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am J Sports Med 42(1):166–172
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32(3):629–634
Lee JK, Lee S, Lee MC (2016) Outcomes of anatomic anterior cruciate ligament reconstruction: bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med 44(9):2323–2329
Lee S, Seong SC, Jo CH, Han HS, An JH, Lee MC (2007) Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. J Bone Joint Surg Am 89(Suppl 3):116–126
Lee S, Seong SC, Jo H, Park YK, Lee MC (2004) Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy 20(8):795–802
Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J (2007) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 35(5):740–748
Lund B, Nielsen T, Fauno P, Christiansen SE, Lind M (2014) Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy 30(5):593–598
Mae T, Shino K, Matsumoto N, Maeda A, Nakata K, Yoneda M (2010) Graft tension during active knee extension exercise in anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 26(2):214–222
Magnussen RA, Carey JL, Spindler KP (2011) Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 19(3):462–472
Mohtadi N, Chan D, Barber R, Oddone Paolucci E (2015) A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at a minimal 2-year follow-up. Clin J Sport Med 25(4):321–331
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. doi:10.1002/14651858.CD005960.pub2(9):CD005960
More RC, Karras BT, Neiman R, Fritschy D, Woo SL, Daniel DM (1993) Hamstrings—an anterior cruciate ligament protagonist. An in vitro study. Am J Sports Med 21(2):231–237
Mulford JS, Hutchinson SE, Hang JR (2013) Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc 21(8):1882–1888
Noyes FR, Barber-Westin SD (2006) Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon–patellar bone autograft. Am J Sports Med 34(4):553–564
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66(3):344–352
Otsuka H, Ishibashi Y, Tsuda E, Sasaki K, Toh S (2003) Comparison of three techniques of anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft. Differences in anterior tibial translation and tunnel enlargement with each technique. Am J Sports Med 31(2):282–288
Paessler HH, Mastrokalos DS (2003) Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon–graft with press-fit fixation without hardware. A new and innovative procedure. Orthop Clin N Am 34(1):49–64
Renstrom PA (2013) Eight clinical conundrums relating to anterior cruciate ligament (ACL) injury in sport: recent evidence and a personal reflection. Br J Sports Med 47(6):367–372
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33(9):1337–1345
Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K (2006) A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med 34(12):1933–1940
Sasaki N, Farraro KF, Kim KE, Woo SL (2014) Biomechanical evaluation of the quadriceps tendon autograft for anterior cruciate ligament reconstruction: a cadaveric study. Am J Sports Med 42(3):723–730
Schulz AP, Lange V, Gille J, Voigt C, Frohlich S, Stuhr M, Jurgens C (2013) Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access J Sports Med 4:243–249
Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB (2002) A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 30(2):214–220
Shelton WR, Fagan BC (2011) Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 19(5):259–264
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31(3):541–554
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Ciszkowska-Lyson B, Siebold R (2015) Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc 23(11):3143–3150
Staubli HU, Schatzmann L, Brunner P, Rincon L, Nolte LP (1996) Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults. Knee Surg Sports Traumatol Arthrosc 4(2):100–110
Staubli HU, Schatzmann L, Brunner P, Rincon L, Nolte LP (1999) Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults. Am J Sports Med 27(1):27–34
Xerogeanes JW, Mitchell PM, Karasev PA, Kolesov IA, Romine SE (2013) Anatomic and morphological evaluation of the quadriceps tendon using 3-dimensional magnetic resonance imaging reconstruction: applications for anterior cruciate ligament autograft choice and procurement. Am J Sports Med 41(10):2392–2399
Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP (2006) Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 14(11):1060–1069
Acknowledgements
We thank Filippo Piana for his help within the data acquisition and Kevin Boehm for his help with the manuscript.
Authors’ contribution
AR was involved in the conception or design, acquisition, analysis, interpretation of data, drafting of the manuscript and final approval; GW was involved in the analysis, interpretation of data, drafting of the manuscript, critical revision of the manuscript and final approval; EH was involved in the analysis, interpretation of data, critical revision of the manuscript and final approval; CH was involved in the acquisition, analysis, interpretation of data, critical revision of the manuscript and final approval; MH was involved in the analysis, interpretation of data, critical revision of the manuscript and final approval; PG was involved in the conception or design, critical revision of the manuscript and final approval; CH was involved in the conception or design, critical revision of the manuscript and final approval; CF was involved in the conception or design, critical revision of the manuscript and final approval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christan Fink received royalties from Karl Storz and consultancies from Karl Storz and Medacta. All other authors declare that they have no conflict of interest.
Funding
None.
Ethical approval
All procedures performed in studies involving human participants as well as the used registry were in accordance with the ethical standards of the institutional review board (IRB) of the Medical University of Innsbruck (AN2015-0050346/4.28) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all patients included in the study.
Rights and permissions
About this article
Cite this article
Runer, A., Wierer, G., Herbst, E. et al. There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26, 605–614 (2018). https://doi.org/10.1007/s00167-017-4554-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4554-2