Abstract
Objective
We aim to discuss the association of isolated atrophy of the abductor digiti quinti muscle in patients with rheumatoid arthritis as well as review the anatomy and imaging findings of this condition on MRI.
Materials and methods
A consecutive series of 55 patients diagnosed with rheumatoid arthritis according to the 2010 ACR/EULAR classification criteria were recruited. MRI of the clinically dominant feet was performed using a 1.5-T scanner.
Results
The study population was predominantly female (94.5%), and the age range was 31–79 years (mean 57.5 ± 11). A total of 55 ankles were examined by MRI, and 20 patients (36.3%), all females, showed abductor digiti quinti denervation signs. Seven patients demonstrated severe fatty atrophy of the abductor digiti quinti, corresponding to Goutallier grade 4, 2 patients showed moderate fatty atrophy (Goutallier grade 3), and the remaining 11 patients showed less than 50% fatty atrophy, corresponding to a Goutallier grade 2. Substantial agreement was found for both intra- and interobserver agreement regarding the Goutallier grading system.
Conclusion
Prevalence of signs of abductor digiti quinti denervation on MRI was high in the studied population, suggesting that rheumatoid arthritis may be associated with inferior calcaneal nerve compression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The inferior calcaneal nerve (ICN), also referred to as Baxter nerve, is the first branch of the lateral plantar nerve and provides motor innervation to the abductor digiti quinti (ADQ) and sometimes to the flexor digitorum brevis and lateral half of the quadratus plantae [1, 2]. Chronic compression of this nerve structure results in denervation signs of ADQ in the MRI, characterized by atrophy and fatty infiltration [3]. Clinically, it is manifested by pain and paresthesia of the calcaneus and can also cause weakness of the ADQ that can be difficult to detect clinically. These findings are part of Baxter neuropathy, which may be the cause of up to 20% of cases of pain in the calcaneus and is often misdiagnosed [4, 5].
The known causes of ICN entrapment are advanced age, calcaneal spurs, plantar fasciitis, masses/vascular compression, muscular hypertrophy, obesity and foot hyperpronation [1, 4, 6, 7]. The literature does not mention rheumatoid arthritis (RA) as a possible cause of this condition.
In this article, we discuss the association of isolated atrophy of the ADQ muscle in patients with RA and review the anatomy and imaging findings of this condition on MRI.
Materials and methods
Patients
A consecutive series of 55 patients diagnosed with RA were recruited from the rheumatology outpatient clinic of the University Hospital Cassiano Antonio Moraes between February and December 2014. The present study expands upon a larger work from our laboratory that examined the correlation between disease activity and MRI scores in rheumatoid arthritis patients. We included patients of all ages with an established diagnosis of RA according to the 2010 ACR/EULAR classification criteria. Exclusion criteria involved patient’s refusal to participate in the study, concomitance of RA with other rheumatic diseases with arthropathy and contraindication for an MRI scan. Ethical approval for the project was obtained from the Local Ethics Committee. Written informed consent was obtained from all subjects prior to inclusion.
Magnetic resonance imaging
MRI of the clinically dominant foot was performed using a 1.5-T scanner (Achieva, Philips, The Netherlands, Best), according to the parameters detailed in Table 1. To determine the degree of fatty infiltration of the ADQ, MRI studies were read in consensus by two experienced musculoskeletal radiologists (RAFM and RBL, 12 and 11 years of experience, respectively), using the grading system described by Goutallier et al. [8]. This system is a five-tiered classification based on the proportion of fat within the muscle tissue: grade 0, normal muscle; grade 1, mild fatty infiltration with some fatty streaks; grade 2, more muscle tissue than fat; grade 3, moderate infiltration with equal fat and muscle tissue; grade 4, greater than 50% fatty muscle infiltration. The entire muscle volume was considered for grading, not just a single slice, using coronal T1-weighted images. To assess inter- and intraobserver agreement, all studies were independently analyzed a second time by both radiologists, blinded to each other's results.
Statistical analysis
Cohen’s kappa (k) statistics were used to calculate intra- and interobserver agreement between the two readers for the ADQ fatty atrophy grading. Agreement was interpreted as determined by Landis and Koch [9]: poor (k < 0.00), slight (k = 0.00–0.20), fair (k = 0.2–0.4), moderate (k = 0.41–0.60), substantial (k = 0.61–0.80) and almost perfect (k = 0.81–1.00). After obtaining formal permission from Recht et al. [10], we used two-tailed Fisher’s exact test to compare their data with our results regarding the frequency of ADQ atrophy. Data evaluation and statistical analysis were performed using SPSS software, version 22 (SPSS, Chicago, IL, USA).
Results
Demographic and clinical features
The study population was predominantly female (94.5%), and the age range was 31–79 years (mean 57.5 ± 11). Further characteristics are summarized in Table 2.
MRI findings
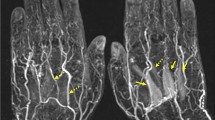
A total of 55 ankles were examined by MRI, and 20 patients (36.3%), all females, showed ADQ denervation signs (Figs. 1, 2). Seven patients demonstrated severe fatty atrophy of the ADQ, corresponding to Goutallier grade 4, 2 patients showed moderate fatty atrophy (Goutallier grade 3), and the remaining 11 patients showed less than 50% fatty atrophy, corresponding to a Goutallier grade 2 (Table 3). Substantial agreement was found for both intra- and interobserver agreement regarding the Goutallier grading system. The interobserver agreement between both radiologists was 76%, with a kappa of 0.672 (95% CI: 0.526–0.819). Intraobserver agreement was 80%, with a kappa of 0.703 (95% CI: 0.552–0.854). Associated MRI findings are shown in Table 4, and we grouped edema/erosions/synovitis as “hindfoot arthritis” since patients showed mixed degenerative and inflammatory lesions in the hindfoot.
Coronal (a) and sagittal (b) T1 images of the left hindfoot of a 60-year-old female patient with rheumatoid arthritis, showing severe atrophy and fatty infiltration selectively involving the ADQ (Goutallier grade 4). Signal intensity of the ADQ (arrows) is similar to that of the adjacent subcutaneous fat, with no signs of edema
We also compared our results with those described by Recht et al. [10] regarding patients with and without fatty degeneration of the ADQ. Our sample demonstrated 36.3% of patients with fatty degeneration in contrast to 6.3% from Recht’s patients, a statistically significant difference, resulting in a two-tailed Fisher’s exact test P value of less than 0.0001.
Discussion
Patients with neuropathies of the ankle may demonstrate a variety of clinical symptoms and exhibit a confusing clinical presentation [7, 11, 12], reported to be underdiagnosed or misdiagnosed as plantar fasciitis or other clinical entities related to heel pain, such as fat pad atrophy, apophysitis and calcaneal stress fracture [13,14,15]. Clinical history, physical examination and electrodiagnostic testing are routinely employed in the investigation of neuropathies, but have been shown not always to be reliable [7].
MR imaging and MR neurography, with its superior soft tissue contrast, allow comprehensive evaluation of the nerves as well as the surrounding soft tissues and adjacent osseous structures. As pointed out by Kim et al. [3], MRI will not be able to confirm the nerve entrapment directly in some cases, but even so, it will be able to demonstrate the muscle signal alterations related to the denervation [3, 7, 14, 16]. MRI signal intensity patterns will differ depending upon the duration and severity of the denervation. Acute and subacute muscle denervation will present with high signal intensity on images from with fluid-sensitive sequences, such as T2-weighted or STIR/SPAIR images, and normal signal intensity on T1-weighted images [17]. In chronically denervated muscles, as present in the cases shown here, different grades of atrophy and fatty replacement will be encountered, demonstrating reduced muscle volume and high signal intensity on T1-weighted images [18].
The ICN, also known as Baxter nerve, is typically the first branch of the lateral plantar nerve, coursing vertically between the abductor hallucis and quadratus plantae muscles and then taking a 90° turn from a vertical to horizontal position as it courses from the medial foot to the ADQ muscle beneath the calcaneus [1, 7, 19, 20]. In some cases, this nerve may take off directly from the posterior tibial nerve [2, 21]. Different studies have shown many causes of ICN nerve entrapment, including hypermobile pronated feet [22], plantar fasciitis, calcaneal spurs, abductor hallucis or quadratus plantae hypertrophy, accessory musculature, obesity, stretching and tethering of the lateral plantar nerve in patients with a cavus-type foot [1, 13, 23]. Three known sites of ICN entrapment have been described: deep to or adjacent to the fascial edge of a hypertrophied abductor hallucis muscle, at the point where the nerve turns 90° along the medial edge of the quadratus plantae muscle and more distally adjacent to the medial calcaneal tuberosity because of calcaneal spurs or soft-tissue inflammatory changes (plantar fasciitis) [1, 7, 24].
Rheumatoid arthritis is a systemic disease that often affects the foot and ankle. Some studies have shown that involvement of the feet is as prevalent as in the hands [25] and that this involvement is usually severe and precedes the hand [26]. Approximately 20% of patients with rheumatoid arthritis present initially with foot and ankle symptoms, and most patients will eventually develop foot and ankle symptoms [27]. Many studies have shown that involvement of the hindfoot in patients with RA increases with a longer disease duration [28,29,30]. As noted by Spiegel and Spiegel [31], when disease duration was less than 5 years, only 8% of patients had hindfoot deformity, increasing to 25% when the disease duration was longer than 5 years, which was the case in our patient sample.
In comparison with the study by Recht et al. [10] in a large patient sample that showed that selective atrophy of ADQ is not a rare finding and described it on 6.3% of ankle MRIs, we found a statistically significantly higher prevalence among our RA patients (36.3%). Our prevalence was also higher than that found by Schmid et al. [32] in asymptomatic individuals (5–6% in volunteers and 4–11% in patients). We postulate that due to the long disease duration of our sample, hindfoot deformities were more likely and could lead to abnormal mechanical stresses, facilitating ICN entrapment.
In the study by Oh et al. [33] regarding the grading system for fatty degeneration of rotator cuff muscles, they found relatively low interobserver reliability, although they included both CT and MRI images in their analysis and the grading was performed by radiologists and orthopedic surgeons with unequal levels of experience. Our results, using only MRI images and analyzed exclusively by experienced radiologists, showed a substantial agreement for both inter- and intraobserver reliability.
In another study by Mizuno et al. [34], they described sex differences in the branching level of the ICN showing that it branched below the malleolar-calcaneal axis in half of female feet and none of the male feet and that this difference may be a cause of the female predominance of nerve damage. Considering that all of our patients with ADQ atrophy were female, this branching pattern may have contributed to a higher incidence of ICN denervation, possibly due to increased mechanical extension and compression in cases where the ICN nerve branches below the malleolar-calcaneal axis.
In our review, our study was the first to demonstrate this relationship between RA and ADQ denervation, and considering that foot and ankle pain is often misdiagnosed, proper use of imaging techniques and familiarity with the MRI findings of nerve entrapment are desired. Prompt diagnosis and appropriate treatment will help avoid or delay severe disability, which could have an impact on both a patient’s employment and sports activities.
Patients with chronic RA do not only suffer from erosions and synovitis. Thus, regarding implications for patient care, this description of increased prevalence of ADQ denervation raises suspicion for other diagnoses that may cause symptoms and limitations, even in the absence of inflammatory activity. This reinforces the need for multidisciplinary care for the rheumatoid patient, including specialized foot orthopedists and specialists in the treatment of chronic pain.
Finally, we emphasize the fact that MRI allows identification of non-inflammatory pathologies (such as the ADQ denervation), which may be symptomatic and misinterpreted from a clinical point of view, sometimes mistakenly considered as higher disease activity, inducing overtreating with potential side effects. The recognition of the higher prevalence of this entity in this group of patients alerts us to the possibility of other diagnoses that may coexist with the joint damage resulting from the underlying disease.
Our study had limitations. We were unable to properly evaluate hindfoot deformity since many MRI studies had no adequate coronal images to measure the tibio-calcaneal angle because of either anatomic variations or the short segment of the tibia being included on ankle MRI. Another limitation was that although the selection of our patients was consecutive, we recruited a lower proportion of men than expected. Therefore, it is not possible to make any inference regarding gender and the frequency of ADQ atrophy in RA. Subsequent studies stratified by sex may help clarify this question.
In conclusion, rheumatoid arthritis patients show a high prevalence of signs of abductor digiti quinti denervation on MRI, suggesting that rheumatoid arthritis may be associated with inferior calcaneal nerve compression. Further research could be performed to evaluate mechanical and inflammatory changes of the hindfoot in rheumatoid arthritis patients to elucidate their relationship with inferior calcaneal nerve entrapment.
References
Baxter DE, Thigpen CM. Heel pain—operative results. Foot Ankle. 1984;5:16–25.
del Sol M, Olave E, Gabrielli C, Mandiola E, Prates JC. Innervation of the abductor digiti minimi muscle of the human foot: anatomical basis of the entrapment of the abductor digiti minimi nerve. Surg Radiol Anat. 2002;24:18–22.
Kim SJ, Hong SH, Jun WS, et al. MR imaging mapping of skeletal muscle denervation in entrapment and compressive neuropathies. Radiographics. 2011;31:319–32.
Chundru U, Liebeskind A, Seidelmann F, Fogel J, Franklin P, Beltran J. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skelet Radiol. 2008;37:505–10.
Lui TH. Endoscopic decompression of the first branch of the lateral plantar nerve. Arch Orthop Trauma Surg. 2007;127:859–61.
Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49:S1–19.
Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30:1001–19.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Recht MP, Grooff P, Ilaslan H, Recht HS, Sferra J, Donley BG. Selective atrophy of the abductor digiti quinti: an MRI study. AJR Am J Roentgenol. 2007;189:W123–7.
Allen JM, Greer BJ, Sorge DG, Campbell SE. MR imaging of neuropathies of the leg, ankle, and foot. Magn Reson Imaging Clin N Am. 2008;16:117–31.
Flanigan RM, DiGiovanni BF. Peripheral nerve entrapments of the lower leg, ankle, and foot. Foot Ankle Clin. 2011;16:255–74.
Ferkel E, Davis WH, Ellington JK. Entrapment neuropathies of the foot and ankle. Clin Sports Med. 2015;34:791–801.
Delfaut EM, Demondion X, Bieganski A, Thiron MC, Mestdagh H, Cotten A. Imaging of foot and ankle nerve entrapment syndromes: from well-demonstrated to unfamiliar sites. Radiographics. 2003;23:613–23.
Pomeroy G, Wilton J, Anthony S. Entrapment neuropathy about the foot and ankle: an update. J Am Acad Orthop Surg. 2015;23:58–66.
Beltran LS, Bencardino J, Ghazikhanian V, Beltran J. Entrapment neuropathies III: lower limb. Semin Musculoskelet Radiol. 2010;14:501–11.
Kamath S, Venkatanarasimha N, Walsh MA, Hughes PM. MRI appearance of muscle denervation. Skelet Radiol. 2008;37:397–404.
Fleckenstein JL, Watumull D, Conner KE, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology. 1993;187:213–8.
Davis TJ, Schon LC. Branches of the tibial nerve: anatomic variations. Foot Ankle Int. 1995;16:21–9.
Louisia S, Masquelet AC. The medial and inferior calcaneal nerves: an anatomic study. Surg Radiol Anat. 1999;21:169–73.
Govsa F, Bilge O, Ozer MA. Variations in the origin of the medial and inferior calcaneal nerves. Arch Orthop Trauma Surg. 2006;126:6–14.
Radin EL. Tarsal tunnel syndrome. Clin Orthop Relat Res. 1983;181:167–70.
Rodrigues RN, Lopes AA, Torres JM, Mundim MF, Silva LL, Silva BR. Compressive neuropathy of the first branch of the lateral plantar nerve: a study by magnetic resonance imaging. Radiol Bras. 2015;48:368–72.
Kenzora JE. The painful heel syndrome: an entrapment neuropathy. Bull Hosp Jt Dis Orthop Inst. 1987;47:178–89.
Boutry N, Lardé A, Lapègue F, Solau-Gervais E, Flipo RM, Cotten A. Magnetic resonance imaging appearance of the hands and feet in patients with early rheumatoid arthritis. J Rheumatol. 2003;30:671–9.
Resnick D, Niwayama G. Rheumatoid arthritis. In: Resnick D, editor. Diagnosis of bone and joint disorders. 3rd ed. Philadelphia: W B Saunders; 1995. p. 966–70.
Jaakkola JI, Mann RA. A review of rheumatoid arthritis affecting the foot and ankle. Foot Ankle Int. 2004;25:866–74.
Cracchiolo A 3rd. Rheumatoid arthritis. Hindfoot disease. Clin Orthop Relat Res. 1997;(340):58–68. https://www.ncbi.nlm.nih.gov/pubmed/9224240.
Mann RA, Horton GA. Management of the foot and ankle in rheumatoid arthritis. Rheum Dis Clin N Am. 1996;22:457–76.
Seltzer SE, Weissman BN, Braunstein EM, Adams DF, Thomas WH. Computed tomography of the hindfoot with rheumatoid arthritis. Arthritis Rheum. 1985;28:1234–42.
Spiegel TM, Spiegel JS. Rheumatoid arthritis in the foot and ankle--diagnosis, pathology, and treatment. The relationship between foot and ankle deformity and disease duration in 50 patients. Foot Ankle. 1982;2:318–24.
Schmid DT, Hodler J, Mengiardi B, Pfirrmann CWA, Espinosa N, Zanetti M. Fatty muscle atrophy: prevalence in the hindfoot muscles on MR images of asymptomatic volunteers and patients with foot pain. Radiology. 2009;253:160–6.
Oh JH, Kim SH, Choi J-A, Kim Y, Oh CH. Reliability of the grading system for fatty degeneration of rotator cuff muscles. Clin Orthop Relat Res. 2010;468:1558–64.
Mizuno D, Naito M, Hayashi S, Ohmichi Y, Ohmichi M, Nakano T. Sex differences in the branching position of the nerve to the abductor digiti minimi muscle: an anatomical study of cadavers. J Foot Ankle Res. 2015;8:22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Andrade Fernandes de Mello, R., Garcia Rondina, R., Valim, V. et al. Isolated atrophy of the abductor digiti quinti in patients with rheumatoid arthritis. Skeletal Radiol 46, 1715–1720 (2017). https://doi.org/10.1007/s00256-017-2741-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2741-3