Abstract
Symptomatic disc calcifications have been reported, especially in the pediatric population, and remain of unknown etiology. Such a condition has been very rarely reported in adults. The aim of this paper is to present a case report of calcific discitis in an adult patient with intravertebral migration and spontaneous calcification resorption. The clinical presentation was that of back pain with an abrupt onset, not related to trauma or to physical activity. No fever or neurological deficits were present. Blood count, erythrocyte sedimentation rate, routine urine, and urine culture were negative. The pain regressed in 20 days with analgesic therapy. Findings of thoracic calcific discitis are illustrated with X-rays, CT, MRI, and bone scintigraphy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intervertebral disc calcification (IDC) represents a common incidental finding on radiographic examinations. The prevalence of IDC in the general adult population has been reported to be 5 % on chest radiographs and 6 % of abdominal radiographs [1–3]. A study in cadavers showed that IDC prevalence is even higher in elderly persons and it increases with age and with the extent of disc space loss [4]. IDC in the elderly population is more frequently seen in the annulus fibrosus and in the lower thoracic spine [4].
Symptomatic disc calcifications are considered rare and have been reported, particularly in the pediatric population [5, 6]. Painful disc calcification in children typically involves the nucleus pulposus and is more frequently seen in the cervical spine [5]. There is little information on symptomatic calcific discitis in the adult population, the literature in this respect being restricted to a few case reports.
The aim of this paper is to present a case of symptomatic calcific discitis with intravertebral migration of the calcification and spontaneous calcification resorption in an adult patient.
Case report
A 40-year-old man had had acute back pain at the thoracolumbar transition for 15 days. Pain had an abrupt onset not related to physical activity or trauma. Symptoms were worse in the upright and in the seated positions. At physical examination patient showed a flexed antalgic position. No fever or neurological deficits were present. Blood count, erythrocyte sedimentation rate, routine urine and urine culture were negative. Abdominal ultrasound was negative.
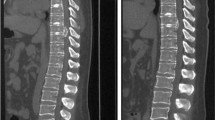
Initial lateral view X-ray showed nucleus pulposus calcification within the disc space at the T9–T10 level (Fig. 1). Technetium bone scan showed increased uptake at the T9 vertebra (Fig. 2). Computed tomography (CT) confirmed the calcified nucleus pulposus and depicted migration of the calcification into the T9 vertebral body with adjacent reactive bone sclerosis (Fig. 3). CT also demonstrated focal calcification within the T10–T11 intervertebral disc. MRI showed the disc calcification as a region of very low signal within the nucleous pulposus of the T9–T10 intervertebral disc and demonstrated bone marrow edema in the adjacent T9 vertebral body (Fig. 4). No abnormalities were identified in the sacroiliac joints by X-rays or by nuclear medicine.
a Sagittal CT reconstruction demonstrated intravertebral migration (black arrowhead) of the calcified nucleus pulposus (black arrow) through of the inferior T9 endplate. b Coronal CT reconstruction also showed intravertebral herniation of the calcified material from the nucleus pulposus (black arrow) through endplate discontinuity and the adjacent reactive bone sclerosis (black dashed arrow). Calcified focus in T10–T11 intervertebral disc (white dashed arrow)
a Sagittal T1-weighted MRI showed low signal intensity of the T9 vertebral body consistent with marrow edema and the low-signal intensity focus in the nucleus pulposus corresponding to the calcification (arrow). b Sagittal T1-weighted fat-suppressed MRI post-gadolinium injection also depicted intervertebral disc calcification (white arrow). The subchondral bone region showed low signal intensity related to bone sclerosis and calcification migration (black arrow) and the rest of the vertebral body demonstrated post-contrast enhancement consistent with reactive bone marrow edema
Only symptomatic analgesic medication was used and the patient returned after 20 days without pain. Follow-up conventional radiographs were obtained and showed almost complete resolution of the calcification (Fig. 5).
Discussion
Painful discal calcification has been reported mainly in the pediatric population and it may be associated with torticollis, fever, leukocytosis, and elevation of the erythrocyte sedimentation rate [5, 6]. The prognosis is excellent since pain resolves with conservative treatment in a few days or weeks in most cases. Two thirds of children are free of symptoms within 3 weeks and 95 % within 6 months [5].
Most common theories suggest a possible role of viral infection or trauma in the etiology of this condition, but these theories have been contradicted by other studies [5, 6]. A vascular insult of the vertebral body was also hypothesized as a possible cause of calcific discitis [6]. The etiology of calcific discitis remains unknown.
There are few reports of calcific discitis in adult patients [7–11], one case report being of calcification migration to the intervertebral foramen [7] and two case reports documented calcification migration into the vertebral body [8, 12]. Lower thoracic spine segments were involved in those few case reports on adult patients.
In our case spontaneous regression of symptoms and partial reabsorption of the disc calcification accompanied intraosseous migration of the calcification, which was documented on the CT multiplanar reconstruction (MPR) images. On CT MPR calcified dense material was identified in the subchondral bone in continuity with disc calcification (Fig. 3). The calcification migration into the T9 vertebral body was associated with an osteoblastic response as documented by CT and by nuclear medicine. The osteoblastic reaction in the vertebral body may be an indication that, in this case, the ongoing inflammatory process was superimposed on a chronic process. MRI and nuclear medicine did not show evidence of inflammatory changes anywhere else.
Hydroxyapatite crystal deposition disease was histologically confirmed in a previous case report similar to our case [10]. Bone involvement in association with hydroxyapatite crystal deposition disease has also been described for various anatomical regions other than the spine. The evolution of calcific tendinitis with calcification migration into the adjacent bone producing osteitis is well documented [11]. Bone involvement associated with calcific tendinitis may be difficult to appreciate on radiographs and MRI or CT could be better for showing bone marrow involvement [11].
Magnetic resonance imaging features of calcific discitis have been described for the pediatric population. The image findings in calcific discitis include disc swelling and vertebral body involvement [6]. Disc swelling may be seen before calcifications are visible on plain films [6]. In the present case MRI showed bone marrow edema and contrast enhancement in the vertebral body similar to that already described in cases of calcific discitis in the pediatric population [6].
The involvement of the vertebral body with bone marrow edema pattern may raise concern about the differential diagnosis with neoplasm, infection, or other inflammatory diseases. An expansive lesion in the vertebral body or in the paravertebral tissues would favor the diagnosis of a neoplasm. In cases of spondylodiscitis contrast enhancement would be also expected in the intervertebral disc, an aspect not evident in this case. Paravertebral soft tissue inflammation or abscesses when present would also favor bacterial infection. The fundamental imaging aspect in our case was to identify nucleus pulposus calcification and its extension to the vertebral endplate.
The main limitation of our case report is that no surgical or pathological confirmation was available. The pathology in question is benign and there was spontaneous regression of the clinical picture, such that biopsy was not necessary. For the same reason previous studies of intraosseous migration of calcific deposits were frequently based on the documentation with sectional imaging findings [11, 12].
In conclusion, radiologists should be aware of the imaging features of calcific discitis, since it may eventually be necessary to consider this in the differential diagnosis of bacterial discitis and of other infiltrative diseases of the vertebral body.
References
Bywaters EG, Hamilton EB, Willians R. The spine in idiopathic haemocromatosis. Ann Rheum Dis. 1971;30:453–65.
Cohen JA, Abraham E. The calcified intervertebral disc. J Med Soc NJ. 1973;70:459–60.
Weinberger A, Myers AR. Intervertebral disc calcification in adults: a review. Semin Arthritis Rheum. 1987;8:69–75.
Chanchairujira K, Chung CB, Kim JY, Papakonstantinou O, Lee MH, Clopton P, et al. Intervertebral disk calcification of the spine in an elderly population: radiographic prevalence, location and distribution and correlation with spinal degeneration. Radiology. 2004;230:499–503.
Sonnabend DH, Taylor TKF, Chapman GK. Intervertebral disc calcification syndromes in children. J Bone Joint Surg. 1982;64-B:25–31.
Swischuk LE, Jubang M, Jadhav S. Calcific discitis in children: vertebral body involvement (possible insight into etiology). Emerg Radiol. 2008;15:427–30.
Fransen P, Collignon F, Van Den Heule B. Foraminal disc herniation Th9-Th10 mimicking abdominal pain. Acta Orthop Belg. 2008;74:881–4.
Smith DM. Acute back pain associated with a calcified Schmorl’s node: a case report. Clin Orthop. 1976;117:193–6.
Bazzi J, Dimar JR, Glassman SD. Acute calcific discitis in adults. Am J Orthop (Belle Mead NJ). 2002;31:141–5.
Lipson SJ, O’Connell JX. Case 37–1991: a 47-year-old woman with back pain and a lesion in a vertebral body. N Engl J Med. 1991;325:794–9.
Flemming DJ, Murphey MD, Shekitka KM, et al. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181:965–72.
Rodacki MA, Castro CES, Castro DS. Diffuse vertebral body edema due to calcified intraspongious disk herniation. Neuroradiology. 2005;47:316–21.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nogueira-Barbosa, M.H., da Silva Herrero, C.F.P., Pasqualini, W. et al. Calcific discitis in an adult patient with intravertebral migration and spontaneous remission. Skeletal Radiol 42, 1161–1164 (2013). https://doi.org/10.1007/s00256-013-1602-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-013-1602-y