Abstract
The aim of the study was to present our cases of calcific discitis, analyze the imaging findings, and review the literature in an attempt to formulate a possible etiology. We reviewed the imaging and clinical findings in nine patients with calcific discitis and accomplished a literature review of the condition. There were nine patients, five males and four females. Age range was 5–13 years with a mean of 9.7 years. Twenty-three discs were involved, nine cervical and fourteen thoracic. Four cervical discs were not calcified but merely swollen. One patient presented with abnormal magnetic resonance (MR) signal changes within a vertebral body. Our literature search revealed another such patient and brought up the possibility that the insult to the disc might be secondary to vertebral body involvement and disruption of the tenuous vascular/nutritional support of the intervertebral disc from the adjacent vertebral body. In the early stages of calcific discitis, only swelling and expansion of the disc are seen. More recently, with MR imaging, vertebral body involvement has been demonstrated to also occur. As a result, it may be that the initial insult (vascular compromise) is to the vertebral body (nutritional support for the disc) rather than to the disc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcific discitis of childhood often presents as an acute, painful problem of the neck. It is characterized by swelling/calcification of intervertebral discs, pain, and in a few cases, fever. Trauma is often suggested as a possible cause, but seldom is trauma present in the history of these patients. In fact, the etiology of this condition is not known. Because of this, we undertook our study where we reviewed the imaging findings in our patients and those in the existing literature in an attempt to come up with a possible etiology for this condition.
Materials and methods
The imaging and clinical findings in our patients were retrospectively reviewed and recorded in Table 1. The patients were collected over a period of 15 years. The location of the calcifications, number of discs involved, and swelling of the discs was documented. In addition, the age and sex of the patients were documented. Symptoms including pain, torticollis, and fever also were documented. The literature on the subject was reviewed.
Results
Our results are presented in Table 2. There were a total of nine patients and a total of 23 discs involved. Nine were cervical and 14 were thoracic. Pain was present in eight patients and torticollis in six. In one patient, calcification of a thoracic disc presented as an incidental finding. Fever was not present in any of the patients. The age range was 5–13 years with a mean of 9.7 years. The male to female ratio was 5:4. Nine discs demonstrated swelling: five on plain films with associated calcification and four on magnetic resonance (MR) imaging, two with associated calcification and two without calcification. Five discs demonstrated disc narrowing with calcification, all in the upper thoracic spine. One patient demonstrated abnormal signal within a vertebral body on MR. Our review of the literature discovered one other such case and brought up the possibility of a vascular insult to the vertebral body as being the primary etiologic factor in the development of calcific discitis.
Discussion
Calcific discitis is a relatively uncommon childhood condition characterized by neck pain, torticollis, and calcification of the intervertebral discs. The onset usually is very acute and, thus, these patients often present to the emergency room for evaluation of a possible more serious condition. In such cases, when calcification of the disc is clearly visible on plain films, the diagnosis is readily secured. However, if calcification of the discs has not yet developed, the findings are more subtle consisting primarily of biconvex expansion (bulging) of the involved intervertebral disc into the adjacent vertebral bodies [1].
Both the nucleus pulposus and anulus fibrosus can be calcified, but in the majority of the cases, the nucleus pulposus is the main part of the disc which becomes calcified. Involvement, as noted in the literature, occurs predominately in the cervical spine with secondary occurrences in the upper thoracic spine [2, 3]. However, in our study, more thoracic discs were involved than cervical discs. Symptomatic patients most commonly present with neck pain and torticollis and in the majority of patients, symptoms resolve within 6 months with no recurrence [2], but calcifications may take years to disappear [2, 3]. More recently, however, a case where calcification disappeared within 2 weeks has been documented [4].
Presentation with fever and an elevated erythrocyte sedimentation rate is rare [3, 5]. None of our patients presented with these findings. Other patients may be entirely asymptomatic [2]. Associated anterior or posterior disc herniation can occur [6–8] and may result in difficulty with swallowing or symptoms of spinal cord compression. However, in most cases, this does not occur.
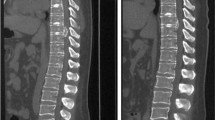
Imaging findings in calcific discitis initially center around plain films (Fig. 1) where oval, round, often fragmented calcifications of the intervertebral discs are seen [2, 3]. These calcifications themselves are difficult to date [3]. In addition, the involved discs often are swollen and bulge into the adjacent vertebral bodies. On MR study of these patients, when the disc is calcified, there is loss of signal on T1- and T2-weighted images. Prior to calcification, however, on plain films, only swelling and bulging of the disc is seen, but with MR imaging, signal loss within the involved disc is seen [1] (Fig. 2). However, in one of our patients, loss of signal in an adjacent vertebral body without loss of vertebral height was seen (Fig. 3) and interestingly, such vertebral involvement also has been documented by others [9]. All of the foregoing is important for now with MR readily available, there may be more forthcoming evidence that would support the concept of the vertebral body sustaining the initial insult. Disc involvement may be secondary.
Swollen discs: no calcification. a Note swollen biconcave discs at the C2–C3 and C6–C7 levels (arrows). b T2-weighted MR study demonstrates loss of signal in the markedly bulging discs (arrows) with encroachment on the adjacent vertebral bodies (with permission from [14])
Vertebral body involvement. a Plain film demonstrating a calcified disc at the C5–C6 level (arrow). Note that the vertebral body below it has slight loss of height and that the disc space between C6 and C7 is increased. b MR, T2-weighted study demonstrates loss of signal in the disc at the C5–C6 level (upper arrow), swelling of the disc with slight loss of central signal in the intervertebral disc between C6 and C7, and loss of signal in the vertebral body of C7 (lower arrow). Loss of signal in two upper thoracic discs also is seen. c Cervical spine, plain film 3 years later. Note persistent calcification of the disc between C5 and C6 (upper arrow). C7 appears normal (lower arrow). d MR, T2-weighted study obtained at the same time as the plain film in c. Note persistent loss of signal at the C5–C6 disc space with loss of height of the adjacent vertebral bodies. The disc space below, that is the one between C6 and C7 is expanded but signal is retained, although it has an irregular configuration. C7 (lower arrow) has recovered its normal signal but remains flattened. There is persistent loss of signal in the upper thoracic discs
In terms of disc calcification, it might be important to review why tissues calcify. Most commonly tissue calcification is related to tissue necrosis secondary to loss or impairment of blood supply. Next most common is calcification as a result of some hypercalcemic, metabolic state. The latter is not the problem in patients with calcific discitis. Therefore, one is left with possible interruption of blood supply to the intervertebral disc with resultant disc necrosis and swelling. This could be secondary to trauma, infection, inflammation, or vasculitis. There is nothing to clearly support any of these etiologies and certainly, trauma was neither present in any of our cases nor in most patients reported in the literature. Bacterial infection also can be excluded as with bacterial infection, the disc space becomes narrowed and destroyed and there is adjacent destruction of vertebral body end plates. This is not seen with calcific discitis. Viral infection, on the other hand, may be more plausible for with viral infections, vasculitis often is the problem. This could lead to impairment of blood supply, defective bone formation, and indeed, such an etiology often is proposed as the causative factor in rubella, cytomegalovirus, herpes simplex virus/HIV, and syphilis syndromes where metaphyseal bone destruction is seen [10, 11]. In addition, the problem is not a problem of chronic vasculitis such as seen with the collagen vascular diseases. Patients with calcific disetis present with one episode and then do not have problems later. Therefore, a chronic vasculitis etiology would seem to be unlikely.
In regards to the blood supply of the intervertebral discs, it has been shown that in children, the discs are supplied by small blood vessels through the cartilaginous vertebral end plates [12, 13]. However, beginning around the age of 8 years old, the vessels begin to obliterate [12, 13]. By 20 to 30 years, the blood vessels for the most part disappear [13]. After this sequence of events, disc nutrition occurs by nonvascular, probably osmotic passage of nutrients from the vertebral end plate to the nucleus pulposus. Obviously, in most instances, no problems result from this transition and it appears that the process is relatively smooth. On the other hand, it also has been noted that during this transition, there is a tenuous vascular relationship between the cartilaginous end plate of the vertebral body and the juxtaposed layer of the intervertebral disc [13]. It is possible therefore that in some patients during the critical period of nutrition transfer, some external factor or combination of factors could result in an abrupt, unprogrammed, and premature interruption of blood/nutrition to the disc/vertebral body complex. Indeed, it may be that the vertebral body becomes involved first, but in most cases, it escapes unharmed. On the other hand, it could also be that such vertebral body involvement could, in some cases, lead to interruption of the tenuous blood/nutrition supply from the vertebral body to the disc. As a result, the disc would become relatively ischemic, swell, and even become necrotic. Later, it would calcify. At the same time, because of its swelling, it would bulge into the adjacent vertebral body. Ordinarily, a bulging disc would bulge peripherally, or into the vertebral body as a Schmorl’s node. However, if the vertebral body were “softened” because of inflammation and vasculitis, the disc could easily bulge in a convex fashion into the vertebral body.
In view of the foregoing hypothesis, it may be that we have been placing more emphasis on the disc than the vertebral body in this condition. It may be, however, that the initial insult is to the vertebral body and that changes in the intervertebral discs are secondary. Further light on this will undoubtedly be cast as more MR studies are performed in these patients.
Conclusion
The findings in calcific discitis consist of more than just calcification of the intervertebral disc. They include disc swelling, which can occur before calcification is seen, and involvement of the vertebral bodies. The blood supply to the intervertebral disc is rather tenuous at a certain period in its development, and although it is not possible to be absolutely sure, the hypothesis of a viral induced vasculitis leading to disruption of blood/nutrition support to the intervertebral disc/vertebral body complex seems plausible. This is especially attractive since no other explanation for this condition, even remotely, seems to be at hand. With the advent of MR imaging, more lights may be shed on this disease entity and its etiology.
References
Swischuk LE, Stansberry SD (1991) Calcific discitis: MRI changes in disks without visible calcification. Pediatr Radiol 21:365–366, doi:10.1007/BF02011490
Sonnabend DH, Taylor TK, Chapman GK (1982) Intervertebral disc calcification syndromes in children. J Bone Jt Surg Br 64(1):25–31
Girodias JB, Azouz EM, Marton D (1991) Intervertebral disk space calcification: a report of 51 children with a review of the literature. Pediatr Radiol 21(8):541–546, doi:10.1007/BF02012591
Klekamp JW, Green NE, Arildson RC (1997) Paravertebral inflammation mistaken for neoplasm or abscess by MRI. J South Orthop Assoc 6:81–87
Furukawa K, Hoshino R, Hasue M, Kuramochi E (1997) Cervical intervertebral-disc calcification in a child: case report with seven-year follow-up. J Bone Jt Surg Am 59(5):692–693
Cronqvist S, Mortensson W (1975) Protrusion of calcified cervical discs into the spinal canal in children. A report of two cases. Neuroradiology 9(4):223–225 doi:10.1007/BF00346152
Heinrich SD, Zembo MM, King AG (1991) Calcific cervical intervertebral disk herniation in children. Spine 16:228–231
McGregor JC, Butler P (1986) Disc calcification in childhood: computed tomographic and magnetic resonance imaging appearances. Br J Radiol 59:180–182
Herring JA, Hensinger RN (1988) Instructional case cervical disc calcification. J Pediatr Orthop 8:613–616
Rabinowitz JF, Wolf BS, Greenberg El, Rausen AR (1965) Osseous changes in rubella embryopathy1 (Congenital Rubella Syndrome). Radiology 85:494–499
Reed GB Jr (1969) Rubella bone lesions. J Pediatr 74:208–213, doi:10.1016/S0022-3476(69)80068–5
Oda J, Tanaka H, Tsuzuki N (1988) Intervertebral disc changes with aging of human cervical vertebra. Spine 13(11):1205–1211, doi:10.1097/00007632-198811000-00001
Chandraraj S, Briggs CA, Opeskin K (1988) Disc herniations in the young and end-plate vascularity. Clin Anat 11:171–176 doi:10.1002/(SICI)1098-2353(1998)11:3<171::AID-CA4>3.0.CO;2-W
Swischuk LE (1991) Calcific discitis: MRI changes in disc without visible calcification. Pediatr Radiol 21:365–366
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swischuk, L.E., Jubang, M. & Jadhav, S.P. Calcific discitis in children: vertebral body involvement (possible insight into etiology). Emerg Radiol 15, 427–430 (2008). https://doi.org/10.1007/s10140-008-0739-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-008-0739-9