Abstract
Objective
Enchondromas are benign lesions that may present with nonspecific features on imaging in children. Correlation of histology with imaging findings is often required to make the final diagnosis of a benign lesion. The aim of this study was to review imaging and pathological findings of enchondromas in children.
Materials and methods
Imaging examinations of 12 enchondromas in 11 patients (median age 14 years) were retrospectively reviewed. Imaging evaluation included an assessment of lesion size, relationship to the growth plate, mineralization, matrix and periosteal reaction, intrinsic MR signal characteristics, and intraosseous and soft-tissue edema. Pathological findings were reviewed.
Results
Lesions were located in the phalanx in 33% (4 out of 12), metacarpal in 25% (3 out of 12), femur in 33% (4 out of 12) and tibia in 8% cases (1 out of 12). The mean size was 28 mm (range, 11–70 mm). Matrix mineralization in a typical “rings-and-arcs” pattern was observed in 20% of the lesions with available radiographs/CT (2 out of 10). Lesions were expansive with endosteal scalloping in 75% of cases (9 out 12) and contacted the growth plate in 50% of cases (6 out of 12). All enchondromas in which MR imaging was available (5 out of 5) demonstrated typical cartilaginous matrix of lobules of high T2 signal, low T1 signal, and peripheral enhancement.
Conclusion
Enchondromas in children are relatively large lesions, with frequent endosteal scalloping and rare matrix mineralization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pediatric neoplasms of bone are relatively uncommon, with benign bone tumors more commonly encountered than malignant ones [1, 2]. Benign pediatric cartilaginous tumors include osteochondromas, enchondromas, periosteal chondromas, chondroblastomas, and chondromyxoid fibromas [2]. Enchondroma, a benign intramedullary tumor, is the second most common benign cartilaginous bone tumor in childhood, after osteochondroma, accounting for up to 24% of all benign bone tumors found in children or adolescents [1–3].
In adults, enchondromas are found in the hands in about 50% of cases, typically in the middle and distal part of the metacarpals, and in the proximal part of the phalanges [4, 5]. Other locations include the proximal and distal shafts of the femur, humerus and feet [4–6]. Enchondromas are typically nonpainful, and are usually discovered in the 3rd or 4th decades of life [5]. In the majority of cases, long bone enchondromas are found as incidental findings on standard radiographs for unrelated trauma or joint disease [5, 6].
About 25% of enchondromas are discovered in children, mostly in the 2nd decade of life [1, 5, 7]. Jaffe hypothesized that embryonic cartilaginous cells derived from the epiphyseal plate are displaced in the metaphysis during growth, and these cells develop into enchondromas [8]. This hypothesis has not been confirmed and recent molecular studies have found enchondromas to be associated with mutations in the genes IDH1 and IDH2 [9]. The purpose of this study was to describe the imaging and pathological findings of enchondromas in children.
Material and methods
The study was approved by the institutional review board and complied with HIPAA guidelines. The requirement for informed consent was waived for this retrospective study.
Patients of 19 years and younger, as defined by the International Childhood Cancer Registry [3] with non-Ollier-related enchondromas diagnosed between January 2004 and January 2009 were retrospectively identified through the consultation of radiological reports using our institution’s picture archiving and communication system. During this period, 11 patients with 12 lesions were identified who had imaging studies and pathological material available for review. There were 6 boys and 5 girls with a median age of 14 (range, 6–19 years; Table 1). Five patients were skeletally mature at the time of biopsy.
Archived pathological material (hematoxylin and eosin-stained glass slides) was available for review for all lesions. Pathological samples were obtained by curettage in 7 cases, by resection in 2 cases, and by needle biopsy in 3 cases. Bone pathologists (GPN, AER) reviewed all cases to confirm the diagnosis of enchondroma. The cellularity of the lesion, relationship of the neoplastic cartilage to adjacent tissue, matrix quality, and chondrocyte size, distribution, and cytological features were evaluated. Diagnosis of enchondroma was based on morphological recognition of a cytologically benign-appearing cartilaginous lesion with variable cellularity and the absence of permeative growth pattern, marked cytological atypia, or other signs of malignancy. Confirmed cases of enchondroma were characterized by the presence of chondrocytes with small, regular, euchromatic nuclei without prominent nucleoli located within individual lacunae and arranged in lobules of abundant hyaline cartilage matrix. None of the cases showed mitoses, significant cellular atypia, or a destructive growth pattern. The main differential diagnostic consideration was low-grade chondrosarcoma, an entity characterized by chondrocytes with larger, more hyperchromatic nuclei, the presence of multiple nuclei per chondrocyte and per lacuna, and importantly, permeation of the bone marrow with encasement of the preexisting trabecular bone.
For each patient, all imaging examinations were reviewed by two board-certified musculoskeletal radiologists in consensus (MAB, 11 years of experience; GB 5 years of experience). Radiographs were available for 10 lesions, CT for 2 lesions, Technetium-99 m (99mTc) bone scintigraphy for 2 lesions, and gadolinium-enhanced MR imaging for 5 lesions. Evaluation of radiographs and CT included assessment of lesion size, mineralization, matrix, endosteal scalloping, and periosteal reaction. The MR imaging evaluation consisted of the same features including intrinsic signal characteristics, intraosseous edema-like signal intensity (high signal on T2-weighted and low signal on T1-weighted images) surrounding the lesion, and soft-tissue edema. In one femoral metaphyseal lesion, follow-up radiographs and MR imaging over a 4-year period were available. Ratio of the lesion length/to the bone length of the involved bone was calculated on either radiographs (n = 10) or MRI imaging (n=2) of the entire bone to illustrate the relative size of the lesion in children.
Results
Imaging findings
Demographics and imaging findings are summarized in Table 1. Lesions were located in the hands in 58% (7 out of 12) and lower extremities in 42% of cases (5 out of 12). Within the hands, the phalanges were involved in 33% (4 out of 12) and the metacarpals in 25% of cases (3 out of 12). One patient demonstrated two enchondromas of the third ray. Whole body 99mTc bone scintigraphy demonstrated no additional lesions and he was felt to have sporadic enchondromas and not enchondromatosis. In the lower extremities, the femur was involved in 33% (4 out of 12) and the tibia in 8% of cases (1 out of 12). The mean enchondroma size was 28 mm (range, 11–70 mm). Lesions contacted the growth plate in 50% of cases (6 out of 12). Radiographs/CTs were available in 10 of the 12 lesions, and typical “rings-and-arcs”-like matrix mineralization was observed in 20% of cases (2 out of 10): 1 femoral lesion and 1 tibial lesion (40% of long bone lesions), but none in any hand lesions (Table 1). Endosteal scalloping was seen in 75% of lesions (9 out of 12): 7 hand lesions and 2 femoral lesions.
Lesions of the hands were expansive with endosteal scalloping and thinning in 100% of cases (7 out of 7; Figs. 1, 2, 3, 4). A pathological fracture was observed in 1 patient (1 out of 7, 14%; Fig. 2). Lesions contacted the growth plate in 57% of cases (4 out of 7). Larger lesions in the hands were located distant from the growth plate, not abutting it. The ratio of hand lesion size to bone length was 51%. No typical matrix mineralization was observed in any of the hand lesions for which radiographs or CT was available (n = 5; Fig. 1). All lesions with available MRI imaging (n = 5) showed a typical cartilaginous matrix of lobules of high T2 signal, low T1 signal, and peripheral enhancement (Figs. 3, 4). 99mTc bone scintigraphy was available in 2 lesions showing intense radiotracer uptake (Fig. 3).
Radiograph in a 15-year-old male subject shows a pathological fracture (arrow) in an enchondroma of the middle phalanx of the long finger. The patient had undergone surgery at the growth plate for radial deviation at the age of 9, likely accounting for the expansive appearance of the proximal aspect of the phalanx
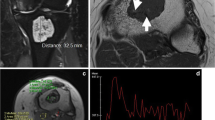
Enchondromas in the third proximal phalanx and metacarpal in a 14-year-old female subject. a 99mTc bone scintigraphy demonstrates increased uptake of the two lesions (black arrows). On MR imaging, the lesion (white arrow) demonstrates b low signal on a sagittal T1-weighted image, c lobules of high signal on a sagittal fat-suppressed T2-weighted image and d enhancement on a gadolinium-enhanced sagittal fat-suppressed T1-weighted image
Enchondroma of the second proximal phalanx in a 19-year-old male subject. a Radiograph shows a nonmineralized lytic expansive lesion (arrow) with endosteal scalloping. On MR imaging, the lesion (white arrow) demonstrates low signal intensity on b a coronal T1-weighted image, c marked enhancement on a contrast-enhanced coronal fat-suppressed T1-weighted image, and d lobules of high signal intensity on an axial fat-suppressed T2-weighted image
Of the 4 femoral lesions, 2 were located in the proximal metaphysis, 1 in the distal diaphysis, and 1 in the proximal epiphysis (Table 1). The ratio of femoral lesion to bone length was 20%. Cortical thinning and scalloping were present in 50% of cases (2 out of 4; Fig. 5). Only the epiphyseal lesion contacted the growth plate. The diaphyseal lesion had a typical cartilaginous matrix of “rings-and-arcs” and periosteal reaction, while no matrix mineralization was seen in the other 3 femoral lesions. In the case of a metaphyseal lesion with available follow-up radiographs and MR imaging examination, radiographs showed progressive growth of the lesion over time, with development of cortical thickening and endosteal scalloping that raised concerns for the potential risk of a pathological fracture. MR imaging demonstrated a typical cartilaginous pattern with lobules of high T2 signal with enhancement in a “rings-and-arcs” pattern following contrast medium administration. Adjacent intramedullary bone edema and soft tissue edema were only observed in this lesion (Fig.5).
Follow-up imaging of an enchondroma of the right femur in a 6 year-old female subject. a Initial radiograph and b follow-up radiograph 4 years later show ill-defined nonmineralized lytic lesion of the proximal femur (arrow; a). Follow-up radiograph (b) demonstrates an increase in lesion size and progressive cortical thickening and cortical scalloping. Cortical thickening corresponded to reactive bone formation on pathology following curettage and was thought to represent healing from prior injury (stress changes/stress fracture; see Fig. 7 c). c MR imaging at the time of the second radiograph demonstrates low signal intensity of the lesion (arrow) on a coronal T1-weighted image, d lobules of high signal on a sagittal fat-suppressed T2-weighted image with adjacent bone marrow edema (asterisk), and e enhancement on coronal and f axial gadolinium-enhanced fat-suppressed T1-weighted images with adjacent marrow enhancement (asterisk) and adjacent soft tissue edema (arrowhead)
The tibial lesion was located in the metaphysis, abutted the growth plate, and demonstrated typical “rings-and-arcs” mineralization on radiographs and CT (Fig. 6). The ratio of lesion to bone length was 20%.
Pathological findings
The histological diagnosis of enchondroma was confirmed in all cases. Importantly, none of the 12 cases examined demonstrated an infiltrative or destructive growth pattern.
Enchondromas of the larger bones (femur and tibia) showed the typical histological features in 60% of cases (3 out of 5). This was characterized by the presence of a lobulated, hypocellular cartilaginous tissue containing small, banal-appearing chondrocytes arranged in clustered lacunae with a background of abundant hyaline cartilage matrix (Fig. 7). Chondrocyte nuclei were small and round with dark chromatin and inconspicuous nucleoli. Binucleation, significant hyperchromasia, and mitoses were absent. An increase in overall cellularity and focal chondrocyte binucleation was seen in 40% of long bone cases (2 out of 5), both in the femur. One of these cases also showed reactive fibrosis, reactive woven bone formation, and focal chondrocyte necrosis suggestive of healing from prior injury. The other case demonstrated a mild degree of myxoid change of the matrix.
Representative histology for enchondromas. a–c Micrographs demonstrate enchondromas of the femur. a is a high power view of benign-appearing hyaline cartilage with the low cellularity typical of lesions of long bones. b shows an enchondroma of the femur with increased cellularity, and c demonstrates increased cellularity, reactive bone formation, and fibrosis (patient from Fig. 5). d Micrograph of an enchondroma of the metacarpal shows the typically higher cellularity of enchondromas of the small bones, surrounded by a thin rim of reactive bone
Hypercellularity was characteristic of the enchondromas within the small bones of the hands. Chondrocytes demonstrated a range of sizes and binucleation was occasionally observed. A thin rim of bone frequently surrounded lobules of cartilage. Detached growth plate cartilage was seen in one case. Variable cellularity within a single lesion, with a mixture of hyper- and hypocellular areas, was also noted in one case of an enchondroma of the metacarpal.
Discussion
In our study, pediatric enchondromas were well-defined, geographical osteolytic lesions that were centrally located within the meta-diaphysis, abutting or approaching the growth plate, with rare matrix mineralization and frequent endosteal scalloping.
Enchondromas in adults are frequently located in the metaphysis and the diaphysis [5, 6]. In our study, lesions abutted the growth plate in 50%, which is comparable to results reported in a series of enchondromas in adult knees (43%) [10]. With the exception of the tibial lesion and 2 lesions of the hand, all enchondromas were located in the metaphysis. Lesions distant from the growth plate were larger than those abutting it, reflecting possible earlier development and migration, which allowed greater growth.
Endosteal scalloping, reflecting the lobular pattern of growth of cartilage with cortical thinning, was observed in 75% of overall cases in our study and in 100% of lesions of the hand. This finding is well recognized in small tubular bones in adults and is not considered a sign of malignancy [11, 12]. In addition to the hand lesions, endosteal scalloping was present in 2 femoral lesions (40% of long bone lesions). In long bones in adults, depending on the size or location within the bones (eccentric or central), endosteal scalloping can be encountered in 0 to 100% of enchondromas [10, 13]. Nevertheless, marked depth and extent of endosteal scalloping are considered worrisome features for chondrosarcomas [6].
A mineralized matrix is variably seen in adult enchondromas of the hands [4]. In this location, adult enchondromas can appear as nonmineralized, purely lytic lesions or show marked mineralization [11]. In our study, none of the hand enchondromas was mineralized. In long bones, mineralized enchondromas were reported in up to 100% of cases [6]. In our study, mineralization was only present in 1 femoral and 1 tibial lesion, representing 40% of all long bone enchondromas. Cortical thickening is a finding considered suspicious for chondrosarcoma in adults [6]. We observed this finding in one femoral lesion that was confirmed to be an enchondroma on histology.
In our study, enchondromas showed increased uptake on 99mTc bone scintigraphy in 2 out of 2 cases. Increased radiotracer uptake on 99mTc bone scintigraphy has been reported in benign enchondromas in adults [6].
Malignant degeneration of enchondromas is infrequent and occurs rarely before skeletal maturity. In addition, the overall prevalence of chondrosarcomas in children is very low (about 0.5/1,000,000) [3]. Some features that may suggest the diagnosis of chondrosarcomas in adults such as cortical thickening, pathological fractures, and absence of mineralization could be encountered in enchondromas in children [6]. Those findings could be even more difficult to interpret as the histological distinction between enchondroma and low-grade chondrosarcoma is often difficult owing to overlapping features [14].
Because of the proximity to the physis, the metaphyseal and meta-diaphyseal areas of long bones are common locations for primary bone tumors in the pediatric population [15]. Besides cartilaginous tumors, metaphyseal or meta-diaphyseal lesions with central mineralization include fibrous dysplasia, calcified solitary bone cysts, bone infarct, lipoma of bone, and infection (Brodie’s abscess) [16]. On imaging examinations, Brodie’s abscess appears generally as well-defined osteolytic areas surrounded by a thin sclerotic zone, but can also be less defined and calcifying. Identification of cortical thickening and internal sequestrum can help to confirm the diagnosis [17]. Epiphyseal enchondromas can be mistaken for chondroblastomas. Nevertheless, the latter are frequently associated with peripheral edema on MR imaging, which is rare in enchondromas and presents frequently with pain, limitation of motion, and possible muscle wasting [18].
In conclusion, our study showed that enchondromas in children appear as relatively large lesions with frequent endosteal scalloping, but with rare mineralization compared with reported features in adults. In order to rule out malignancy, appreciation of the spectrum of pathological findings and correlation with imaging findings is mandatory.
References
Adler CP, Kozlowski K. Primary bone tumors and tumorous conditions in children. Berlin Heidelberg New York: Springer; 1993.
Van den Berg H, Slaar A, Kroon HM, Taminiau AHM, Hogendoorn P. Results of diagnostic review in pediatric bone tumors and tumorlike lesions. J Pediatr Orthop. 2008;28:561–4.
Parkin DM, Stiller CA, Draper GJ, Bieber CA. The international incidence of childhood cancer. Int J Cancer. 1988;42:511–20.
Dorfman H, Czerniak B. Bone tumors. Philadelphia: Mosby; 1998.
Unni K. Dahlin’s bone tumors: general aspects and data on 11,087 cases. Philadelphia: Lippincott-Raven; 1996.
Murphey MD, Flemming DJ, Boyea SR, et al. Enchondroma versus chondrosarcoma in the appendicular skeleton: differentiating features. Radiographics. 1998;18:1213–37.
Biermann JS. Common benign lesions of bone in children and adolescents. J Pediatr Orthop. 2002;22:268–73.
Jaffe HL, Lichtenstein L. Solitary benign enchondroma of bone. Arch Surg. 1943;46:480–93.
Amary MF, Bacsi K, Maggiani F, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol. 2011;224:334–43.
Walden MJ, Murphey MD, Vidal JA. Incidental enchondromas of the knee. AJR Am J Roentgenol. 2008;190:1611–5.
Cawte TG, Steiner GC, Beltran J, Dorfman HD. Chondrosarcoma of the short tubular bones of the hands and feet. Skelet Radiol. 1998;27:625–32.
Kendell SD, Collins MS, Adkins MC, Sundaram M, Unni KK. Radiographic differentiation of enchondroma from low-grade chondrosarcoma in the fibula. Skelet Radiol. 2004;33:458–66.
Bui KL, Ilaslan H, Bauer TW, et al. Cortical scalloping and cortical penetration by small eccentric chondroid lesions in the long tubular bones: not a sign of malignancy? Skelet Radiol. 2009;38:791–6.
Hasegawa T, Seki K, Yang P, et al. Differentiation and proliferative activity in benign and malignant cartilage tumors of bone. Hum Pathol. 1995;26:838–45.
Wootton-Gorges SL. MR imaging of primary bone tumors and tumor-like conditions in children. Magn Reson Imaging Clin N Am. 2009;17:469–87.
Amling M, Werner M, Pösl M, et al. Calcifying solitary bone cyst: morphological aspects and differential diagnosis of sclerotic bone tumours. Virchows Arch. 1995;426:235–42.
Schmit P, Glorion C. Osteomyelitis in infants and children. Eur Radiol. 2004;14(Suppl 4):L44–54.
Sailhan F, Chotel F, Parot R. Chondroblastoma of bone in a pediatric population. J Bone Joint Surg Br. 2009;91:2159–68.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bierry, G., Kerr, D.A., Nielsen, G.P. et al. Enchondromas in children: imaging appearance with pathological correlation. Skeletal Radiol 41, 1223–1229 (2012). https://doi.org/10.1007/s00256-012-1377-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-012-1377-6