Abstract
Purpose
The purpose of the study was to examine the most adequate cut-off point for median nerve cross-sectional area and additional ultrasound features supporting the diagnosis of carpal tunnel syndrome (CTS).
Material and methods
Forty wrists from 31 CTS patients and 63 wrists from 37 asymptomatic volunteers were evaluated by ultrasound. All patients were women. The mean age was 49.1 years (range: 29–78) in the symptomatic and 45.1 years (range 24–82) in the asymptomatic group. Median nerve cross-sectional area was obtained using direct (DT) and indirect (IT) techniques. Median nerve echogenicity, mobility, flexor retinaculum measurement and the anteroposterior (AP) carpal tunnel distance were assessed. This study was IRB-approved and all patients gave informed consent prior to examination.
Results
In CTS the median nerve cross-sectional area was increased compared with the control group. Median nerve cross-sectional area of 10 mm2 (DT) and 9 mm2 (IT) had high sensitivity (85% and 88.5%, respectively), specificity (92.1% and 82.5%) and accuracy (89.3% and 82.5%) in the diagnosis of CTS. CTS patients had an increased carpal tunnel AP diameter, flexor retinaculum thickening, reduced median nerve mobility and decreased median nerve echogenicity.
Conclusion
Ultrasound assists in the diagnosis of CTS using the median nerve diameter cut-off point of 10 mm2 (DT) and 9 mm2 (IT) and several additional findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS) is a common entrapment neuropathy of the median nerve. CTS is characterised by pain and sensory disturbance along the distribution of the median nerve, as well as thenar muscle atrophy in the advanced stages. The diagnosis may be made clinically [1] and with electromyography (EMG) [2]. Ultrasound may also be valuable in the diagnosis of CTS [3]. Several studies [2, 4–6] have demonstrated that the combination of carpal tunnel ultrasound in combination with clinical features and EMG were more sensitive and specific than clinical evaluation or EMG in isolation. Ultrasound has proved to be able to depict normal and pathologic nerves, including anatomical variants [7, 8] and abnormalities associated with CTS [9].
Prior studies [10–12] have attempted to establish cut-off values for the median nerve cross-sectional area and have described ultrasound features such as median nerve echogenicity, mobility and flexor retinaculum bulging that can be useful in the diagnosis of patients with CTS. However, there is a lack of consensus in the medical literature regarding some of these topics, mainly the median nerve cut-off point.
The purpose of this study was to evaluate the best cut-off value for the cross-sectional area of the median nerve and to describe additional ultrasound features that may assist in the diagnosis of CTS.
Material and methods
Study population
This is a prospective case-control study comprising of 68 participants and 103 wrists that was carried out between September 1999 and October 2000. All participants were women. The patients’ mean age was 49.1 years (range: 29–78) and that of the controls 45.1 years (range: 24–82). The 40 CTS were diagnosed clinically and with EMG. They were considered to be candidates for surgery. There were 21 right and 19 left wrists. Of the 63 asymptomatic wrists, 30 were on the right and 33 on the left. All patients had been referred by the hospital’s Department of Orthopaedic Surgery in a non-consecutive fashion. Participants were eliminated from the study if they had a history of underlying diseases (such as gout, rheumatoid arthritis and diabetes mellitus), pregnancy, previously performed wrist surgery or fracture, expansive lesions within the carpal tunnel and variants of the carpal tunnel (such as accessory muscles, bifid median nerve and persistent median artery). Among the originally evaluated 125 wrists 22 were excluded due to anatomical variations. Institutional Review Board approval was obtained for this study. Informed consent was provided by all participants prior to examination.
Ultrasound imaging
Studies were done using a Logic-700 (General Electric, Milwaukee, WI, USA) with a linear array transducer ranging from 9 to13 MHz. A board certified radiologist (RAS) with expertise in musculoskeletal imaging and 6 years of practical experience performed all examinations.
Participants were seated with the forearm lying on a table, wrist in supination and extended fingers during the examination. Axial and transverse images were obtained at the proximal and distal carpal tunnel. All examinations followed the same protocol: a quick overview of the volar side was performed to rule out expansive lesions and anatomical variations. Subsequently, a detailed evaluation of the carpal tunnel was performed. Within the carpal tunnel, the median nerve was identified as a rounded hypoechoic structure with hyperechoic dots inside. The median nerve was qualitatively assessed considering its echogenicity. Meanwhile, the quantitative evaluation assessed median nerve cross-sectional area, flexor retinaculum thickness, median nerve mobility, and carpal tunnel anteroposterior (AP) distance.
The median nerve cross-sectional area was obtained at the level of the pisiform bone using the direct (DT) and indirect (IT) technique. The DT was defined by tracing a continuous line around the inner hyperechoic rim of the median nerve with electronic calipers [4] (Fig. 1); and it was performed in all symptomatic (40 out of 40) and asymptomatic wrists (63 out of 63). Meanwhile, the IT resulted from the AP measurement (D1) and transverse distance (D2) of the inner median nerve calculated through the ellipsoid formula \( {\left[ {\pi {{\left( {{\text{D1}} \times {\text{D2}}} \right)}} \mathord{\left/ {\vphantom {{{\left( {{\text{D1}} \times {\text{D2}}} \right)}} {\text{4}}}} \right. \kern-\nulldelimiterspace} {\text{4}}} \right]} \) [5] (Fig. 2). The IT was performed in 65% of symptomatic wrists (26 out of 40) and 100% of asymptomatic wrists (63 out of 63). The radiologist obtained three measurements of the median nerve for each technique. The mean value was used for statistical analysis. Median nerve mobility was calculated by measuring the distance between the radial margin of the median nerve and the radial margin of the ulnar artery, with and without passive flexion of the fingers (Fig. 3). Median nerve mobility was assessed in 65% of the symptomatic (26 out of 40) and 100% of the asymptomatic wrists (63 out of 63). In addition, the AP distance of the flexor retinaculum (arched hyperechoic strip anterior to the median nerve) and the AP diameter of carpal tunnel (between the cortical bone of the capitate and the external border of the flexor retinaculum) were obtained during examinations (Fig. 4).
Ultrasound shows the AP and transverse distances to calculate the median nerve area using the indirect technique through the ellipsoid formula \( {\left[ {\pi {{\left( {{\text{D1}} \times {\text{D2}}} \right)}} \mathord{\left/ {\vphantom {{{\left( {{\text{D1}} \times {\text{D2}}} \right)}} {\text{4}}}} \right. \kern-\nulldelimiterspace} {\text{4}}} \right]} \), in a patient without carpal tunnel syndrome. (Median nerve cross-sectional area = 0.062 cm2)
A 52-year-old woman with a clinical and electromyographic diagnosis of carpal tunnel syndrome. Median nerve mobility was calculated by measuring the distance between the radial margin of the median nerve and the radial margin of the ulnar artery, a with and b without passive flexion of the fingers. Measurements acquired were 0.69 cm and 0.62 cm respectively. MN median nerve, A ulnar artery
Same patient as in Fig. 3, demonstrating the AP distance of carpal tunnel measured between the capitate cortex and the external border of the flexor retinaculum. C capitate, FR flexor retinaculum
Statistical analysis
The cross-sectional area of the median nerve, thickness of the flexor retinaculum and AP diameter of the carpal tunnel of symptomatic and asymptomatic wrists were compared using a Mann–Whitney test. An unpaired Student’st test was used for comparing the mobility of the median nerve. The echogenicity of median nerve and the cut-off value established by DT and IT were evaluated with a Fisher’s statistic test. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy demonstrated the efficacy of the IT values, using 15 mm2 as the cut-off value [2]. The coefficient of correlation was used to evaluate the relationship between DT and IT measurements. Various cut-off values were calculated to determine the best median nerve cross-sectional area. A significance level of 0.05 was used.
Results
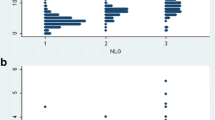
There was a statistically significant difference between the DT (15.1 ± 7.3 mm2 in symptomatic and 8.1 mm2 ± 1.6 in asymptomatic patients; p value = 0.001; Fig. 5) and IT (15.51 mm2 ± 9.89 in symptomatic and 8.04 mm2 ± 1.50 patients; p value = 0.001). The correlation between DT and IT was strong (r = 0.99). Using a cut-off value of 15 mm2 for IT resulted in a sensitivity of 34.6%, specificity of 100%, PPV of 100%, NPV of 78.8% and accuracy of 80.9% in diagnosing CTS. With a cut-off value of 9 mm2 for IT, the corresponding results were 88.5%, 82.5%, 67.7%, 94.6% and 82.5% respectively. With a cut-off value of 10 mm2 for DT the values were 85.0%, 92.1%, 87.2%, 90.6% and 89.3% respectively.
In 32 of the 40 symptomatic wrists (80%) the median nerve was hypoechoic (p = 0.001 and p = 0.004 for DT and IT respectively).
In addition, a statistically significant difference was found for the AP distance of the carpal tunnel (CTS = 1.28 ± 0.18 cm, control = 1.18 ± 0.1 cm; p = 0.003), the flexor retinaculum thickness (CTS = 0.88 ± 0.23 mm, control = 0.75 ± 0.1 mm; p = 0.018), and mobility of the median nerve (CTS = 0.96 ± 0.66 mm, range: 0.07–3.1 mm; control = 1.29 ± 0.7 mm, range: 0.13–3 mm; p = 0.041).
Discussion
This study demonstrates that a median nerve cross-sectional area of more than 10 mm2 (DT), and more than 9 mm2 (IT) are both sensitive and specific in diagnosing CTS. Furthermore, symptomatic wrists had a thicker flexor retinaculum, an increased AP diameter of the carpal tunnel, and reduced echogenicity and mobility of the median nerve, compared with the asymptomatic group.
The cross-sectional area of the median nerve (DT and IT) at the pisiform bone level was higher in symptomatic wrists compared with the asymptomatic group. These findings concur with previous studies [2, 4, 5]. In the present study both DT and IT were demonstrated to be accurate in diagnosing CTS, contrary to Duncan et al. [4] who reported that the DT had more accurate results than the IT. Moreover, a high correlation (r = 0.99) between the areas calculated through DT and IT, in symptomatic and asymptomatic wrists, was found in our analysis.
Kamolz et al. stressed the need for standardisation of median nerve cross-sectional area cut-offs [13]. The majority of previously published studies addressed values ranging from 9 mm2 to 12 mm2 [3, 4, 6, 10–12, 14–17]. Our results demonstrated that 10 mm2 (DT) is the most adequate cut-off value (specificity = 92.1) this corroborates previous findings [10, 15]. In addition, our study demonstrated that decreased echogenicity of the median nerve was found in 80% of symptomatic wrists. Only a few authors have considered qualitative changes of median nerve as a diagnostic criterion, mainly because the changes in the median nerve echogenicity are prone to angle beam artifacts, are operator- and equipment-dependent, and may be too subtle to be detected by all readers [2, 4, 18]. We believe that such changes should be included in the diagnosis of CTS.
To the best of our knowledge, this is the first series to demonstrate a difference in flexor retinaculum thickness and AP diameter of the carpal tunnel in symptomatic and asymptomatic wrists. Lee and colleagues [2] reported flexor retinaculum thickness and AP carpal tunnel distance measurements. However, they only reported values for asymptomatic wrists.
Nakamichi and Tachibana [19] described patients with CTS having decreased median nerve transverse sliding compared with the control group, indicating that there is a restricted physiological motion of the nerve. The results from our study concur with this finding.
We recognise some of the limitations of this study. First, it was a single institution study with a relatively small sample size. Second, ultrasound examinations were performed by a single radiologist and inter-observer agreement of the ultrasound findings was not attempted. Finally, our sample was composed solely of female participants. However, previous studies did not demonstrate gender-related differences in the ultrasound cross-sectional area among male and female CTS patients [4, 11].
In conclusion, ultrasound assists in the diagnosis of CTS using the median nerve diameter (cut-off point of 10 mm2 [DT] and 9 mm2 [IT]) and several additional findings.
References
Phalen GS. The carpal-tunnel syndrome. Clinical evaluation of 598 hands. Clin Orthop Relat Res 1972; 83: 29–40.
Lee D, van Holsbeeck MT, Janevski PK, Ganos DL, Ditmars DM, Darian VB. Diagnosis of carpal tunnel syndrome. Ultrasound versus electromyography. Radiol Clin North Am 1999; 37: 859–872.
Wiesler ER, Chloros GD, Cartwright MS, Smith BP, Rushing J, Walker FO. The use of diagnostic ultrasound in carpal tunnel syndrome. J Hand Surg [Am] 2006; 31: 726–732.
Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol 1999; 173: 681–684.
Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med 1991; 10: 531–537.
Koyuncuoglu HR, Kutluhan S, Yesildag A, Oyar O, Guler K, Ozden A. The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electrodiagnostic tests. Eur J Radiol 2005; 56: 365–369.
Beekman R, Visser LH. High-resolution sonography of the peripheral nervous system—a review of the literature. Eur J Neurol 2004; 11: 305–314.
Silvestri E, Martinoli C, Derchi LE, Bertolotto M, Chiaramondia M, Rosenberg I. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology 1995; 197: 291–296.
Buchberger W, Judmaier W, Birbamer G, Lener M, Schmidauer C. Carpal tunnel syndrome: diagnosis with high-resolution sonography. AJR Am J Roentgenol 1992; 159: 793–798.
Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology 2004; 232: 93–99.
Ziswiler HR, Reichenbach S, Vogelin E, Bachmann LM, Villiger PM, Juni P. Diagnostic value of sonography in patients with suspected carpal tunnel syndrome: a prospective study. Arthritis Rheum 2005; 52: 304–311.
Yesildag A, Kutluhan S, Sengul N, et al. The role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol 2004; 59: 910–915.
Kamolz LP, Schrogendorfer KF, Rab M, Girsch W, Gruber H, Frey M. The precision of ultrasound imaging and its relevance for carpal tunnel syndrome. Surg Radiol Anat 2001; 23: 117–121.
Sarria L, Cabada T, Cozcolluela R, Martinez-Berganza T, Garcia S. Carpal tunnel syndrome: usefulness of sonography. Eur Radiol 2000; 10: 1920–1925.
Chen P, Maklad N, Redwine M, Zelitt D. Dynamic high-resolution sonography of the carpal tunnel. AJR Am J Roentgenol 1997; 168: 533–537.
Kele H, Verheggen R, Bittermann HJ, Reimers CD. The potential value of ultrasonography in the evaluation of carpal tunnel syndrome. Neurology 2003; 61: 389–391.
Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve 2003; 27: 26–33.
Buchberger W. Radiologic imaging of the carpal tunnel. Eur J Radiol 1997; 25: 112–117.
Nakamichi K, Tachibana S. Restricted motion of the median nerve in carpal tunnel syndrome. J Hand Surg [Br] 1995; 20: 460–464.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sernik, R.A., Abicalaf, C.A., Pimentel, B.F. et al. Ultrasound features of carpal tunnel syndrome: a prospective case-control study. Skeletal Radiol 37, 49–53 (2008). https://doi.org/10.1007/s00256-007-0372-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-007-0372-9