Abstract
Left ventricular (LV) dysfunction is a risk factor for adverse outcomes in older children and adults with repaired Tetralogy of Fallot (rToF). Pulmonary regurgitation (PR), right ventricular (RV) dilation, and dysfunction have been shown to result in abnormal LV myocardial mechanics and dysfunction. The aim of our study was to evaluate LV rotational mechanics, especially apical rotation in young children with rToF with and without RV dilation. This is a retrospective, single center study in 28 asymptomatic young children with rToF (16 with RV dilation; 12 without RV dilation); 29 age-matched normal controls. RV and LV systolic and diastolic function was studied using conventional two-dimensional echocardiography (2DE) and speckle tracking echocardiography (STE). Rotational mechanics studied included basal and apical rotation (BR, AR), peak twist (calculated by difference between the apical and basal rotation), twist rate (TR), and untwist rate (UnTR). The mean age of the cohort was 4.7 years (± 2.3). Abnormal AR, BR, TR, and UnTR were noted in patients with rToF. The abnormalities were significant in magnitude as well as the direction of rotation; more pronounced in the absence of RV dilation. LV systolic and diastolic dysfunction as evidenced by abnormal AR and degree of untwist is inherent in rToF and not associated with RV dilation in rToF children. Abnormal BR may reflect a lack of maturation to adult type of rotational mechanics. Further longitudinal studies are required to study the progression of these abnormalities and their correlation with clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Left ventricular (LV) systolic and diastolic dysfunction has a significant impact on morbidity and survival in adults with repaired Tetralogy of Fallot (rToF) [1,2,3,4,5,6]. LV dysfunction is thought to be the result of systolic and diastolic ventricular–ventricular interactions. Abnormal LV myocardial longitudinal and rotational mechanics have been demonstrated by speckle tracking echocardiography (STE) in older children and adults with significant pulmonary regurgitation, right ventricular (RV) dilation, and RV systolic dysfunction [7,8,9]. It is unclear how early these abnormalities manifest and whether early RV dilation has an impact on LV response. Apical rotation and untwist rate have been validated as surrogates for LV contractility and for early diastolic function, respectively [10,11,12,13]. Additionally, there are maturational changes in direction of basal rotation (BR) which progresses from counterclockwise in infancy, to neutral in early childhood and finally becoming clockwise by adolescence. Conversely, apical rotation (AR) remains counterclockwise with increasing rotational magnitude from infancy to adolescence [14,15,16]. We aimed to assess the prevalence of systolic dysfunction and impaired relaxation in children with rToF by measurement of apical rotation and untwist rate. We hypothesized that abnormal apical rotation and untwist would be inherent in rToF and independent of RV dilation.
Methods
This was a retrospective, single center cross sectional study. The study was approved by the institutional review board. The subjects were divided into three groups: group 1 included patients with rToF with dilated RV, group 2 included patients with rToF with non-dilated RV, and group 3 included age-matched normal controls. Our echocardiography-reporting database was queried for Tetralogy of Fallot during period of 1/1/2009 to 06/30/2015. We included all children within the age group of 1–10 years of age with rToF. Exclusion criteria included pulmonary stenosis and/or residual right ventricular outflow tract (RVOT) gradient of greater than 20 mmHg, incomplete demographic information, and sub-optimal images for myocardial deformation analysis. For the normal cohort, subjects were excluded if the images were inadequate for analysis, if they had acquired or congenital heart disease as determined by history, physical examination, chest X ray, echocardiogram or ECG, corrected gestational age < 37 weeks, BMI > 95th percentile for children > 2 year of age or weight for length z score > 2 based on WHO standards for < 2 years old children, acute or systemic disorder with cardiovascular manifestation, documented history of 1st degree relative with cardiomyopathy (non-ischemic) and congenital heart disease, thoracic or spinal deformities. Body surface area (BSA) was estimated using the Haycock method.
The variables studied were LV rotational parameters for systolic and diastolic function measured by LV basal and apical rotation, LV twist, twist rate, and untwist rate.
Two-Dimensional Transthoracic Echocardiography (2D TTE)
The rToF group was allocated to group 1 or 2 based on the initial echocardiographic reports. The allocation of each subject was then confirmed by published American Society of Echocardiography (ASE) guidelines used for determination of RV size and function [17] and additional published criteria for RV dilation namely indexed RV end diastolic area (RVEDAi), annular tilt, RV diameter at the base and mid ventricular level [18]. RV Myocardial Performance Index (MPI) or Tei index was calculated using Doppler tissue imaging tracing at the tricuspid valve annulus [19]. Tricuspid annular peak systolic excursion (TAPSE) was measured from RV focused apical four-chamber (4C) view using M-mode imaging. RV end diastolic area (RVEDA) and RV end systolic area (RVESA) were measured by tracing the RV in the two different phases from the RV focused apical 4C view. Fractional area change for the RV was calculated using the formula (RVEDA − RVESA/RVEDA) × 100. RV diameter was measured at end-diastole at mid-ventricular level and at the base, from RV focused apical 4C view [18]. Annular tilt was calculated in degree for the angle of the tricuspid valve plane relative to the mitral valve plane at end-diastole in the apical 4-chamber view [20]. Measured LV diastolic function parameters included tissue Doppler indices (TDI) at the septum and lateral annulus of the mitral valve. Measured RV diastolic function indices included pulse wave Doppler (PW) inflow velocities and TDI at the tricuspid valve annulus. Other evidence of RV restrictive physiology included the presence of antegrade atriosystolic pulmonary artery (PA) flow on pulsed wave Doppler in the main pulmonary artery in all recorded cardiac cycles (> 5).
Speckle Tracking Echocardiography (STE)
The required echocardiographic images were obtained from our digital archive. We selected patients who had analyzable images of 1. The RV from RV focused apical 4-chamber (C) view; 2. The LV from apical 4C, 3-chamber (3C), 2-chamber (C); 3. The LV from parasternal short axis (PSAX) of the LV base and apex (smallest cavity past the level of the papillary muscles). The clips were stored as DICOM files and transferred to vendor independent TOMTEC software (Image arena version 4.6, build 4.6.3.9, Unterschleissheim, Germany) for myocardial deformation analysis [21]. All measurements were performed by a single observer (RK). The RV average systolic longitudinal strain (RV l ε) was measured by tracing the endocardial border manually starting from the tricuspid annulus. The septal segments were excluded from analysis, and the average longitudinal strain was calculated only for RV free wall. For the LV average systolic longitudinal strain (LV l ε), the endocardial border was manually traced in three apical views (4C, 3C, 2C). For rotational parameters, PSAX views for the base and apex were used. The endocardial border was traced for the base and the apex. The optimal tracing and analysis was accepted after visual inspection for each of the above measurements. The 2D CPA (version 1.2.3.6) from TOMTEC exported text files containing rotational displacement in degree for one complete heart cycle and the text files were then imported into a custom excel spreadsheet and plotted as graphs. The data were normalized to 100% to adjust for discrepancies in heart rate. The basal and apical rotation, twist, and untwist rates were calculated from these graphs. Peak twist (degrees) was calculated as the difference between the apical and basal rotation during systole. The peak untwist rate was taken as the initial deflection during the first third of diastole (Fig. 1a) [15].
A second independent analysis of the outcome measures was conducted by a second observer (SSR) for inter-observer agreement in randomly selected 13 patients and on 10 patients by the same first observer for analysis of intra-observer agreement.
Statistical Analysis
The results of the study were expressed as mean ± standard deviation (SD) for continuous variables. The categorical data were described as numbers and percentages. F tests from one-way ANOVA were used to test for differences in the mean values of each parameter among the three groups (dilated, non-dilated, control). For those parameters where the F test was significant, post hoc testing was done with the Tukey’s studentized range method to account for multiple comparisons. Inter- and intra-observer agreement was calculated using interclass correlation coefficients (ICC). Pearson correlation coefficients for continuous variables and Spearman correlation coefficients for categorical variables were calculated.
All analyses were performed using SAS version 9.4.
Results
Patient Characteristics
A total of 110 subjects with rToF were identified, of which only 28 met the inclusion criteria as mentioned above. The normal cohort consisted of 29 age-matched subjects. The mean age for the whole study cohort was 4.7 years (SD-2.3 years, median age 5.5 years). The baseline demographics are described in Table 1. The rToF patients were divided into two groups based on ASE guidelines and above mentioned criteria—16 were included in the group of dilated RV (group 1) and 12 in the group of non-dilated RV (group 2) (Table 2).
In group 1, all patients had moderate to severe pulmonary regurgitation (PR), as compared to group 2 patients, where all had less than mild PR. 75% of the patients in group 1 had either a trans-annular patch or RV-PA conduit as their repair as compared to 91.6% of patients in group 2 who underwent non-trans-annular patch repair. The age at initial surgery was statistically different in the two groups, with group 1 undergoing surgical repair earlier as compared to group 2 (Table 1). However, one patient in group 1 was palliated with a BT shunt and underwent complete repair later at 2 years of age.
The average QRS duration was statistically different among all groups. QRS duration was longest in group 1, followed by group 2 and shortest in group 3.
RV Size and Function
Group 1 and group 2 were differentiated based on echocardiographic estimate of RV dilation (Table 2). The functional assessment using TAPSE, FAC, and Tei index was not statistically different between the two groups. The average RV l ε showed a trend of being lower among the rToF patients as compared to the normal controls, but was not statistically different between the groups (Fig. 2a). RV diastolic function was also abnormal in the entire rToF cohort but was not different between the dilated and non-dilated groups (Table 3).
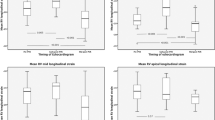
LV Systolic Function
Systolic function assessment with LV ejection fraction (EF) was not different among the sub-groups of rToF (Table 2). The average LV l ε was lowest in group 2 (Fig. 2b). Rotational mechanics with respect to both magnitude and direction were abnormal in group 2 more than in group 1. LV apical rotation was statistically lower and reversed (clockwise) in group 2 (Fig. 3a; Table 4). LV basal rotation did not differ statistically, although reversed rotation (counterclockwise) was observed in most of the patients in group 2 (Fig. 3b; Table 4). Twist and twist rate were also abnormal in group 2 (Fig. 3c, d). Group 1 who had moderate or more PR and RV dilation was very similar to the normal cohort. The distribution for the abnormal rotation in each group is shown in Table 4.
LV Diastolic Function
Septal E′ was statistically lower in those with no RV dilation and less than mild PR (group 2) as compared to normal controls, but similar for the rToF cohort. There was no difference in LV lateral wall E′. Average E/E′ (average for septal and lateral) was higher in group 2 as compared to normal controls. There was no statistical difference in isovolumic relaxation time (IVRT) among the 3 groups (Table 3). We did observe a trend with prolonged IVRT and lower septal E′ with reversed untwist rate which did not reach statistical significance. Untwist rate was significantly lower and reversed in direction in group 2 (Fig. 3e). Untwist rate correlated negatively with apical rotation in rToF, r = 0.5 and p = 0.004 (Fig. 4a) and positively with basal rotation, r = 0.5, p = 0.01 (Fig. 4b).
RV–LV Function Interaction
There was moderate positive correlation between RV l ε and LV l ε among rToF patients (r = 0.5). The RV l ε had no correlation with LV rotational mechanics. RV dilation though was associated with preserved direction of apical rotation and untwist rates (Fig. 4b; Table 4).
Reproducibility
Inter-observer Variability
ICC was good for apical rotation and twist (0.9), modest for basal rotation (0.75).
Intra-observer Variability
Good correlation for apical rotation (ICC 0.8) and modest for basal rotation (0.6).
Discussion
Abnormalities in LV myocardial deformation in rToF have been attributed to adverse ventricular interactions resulting from RV volume load and dysfunction. This is the first study that suggests that rotational abnormalities may be inherent in a subset of rToF and can be detected in early childhood. Contrary to prior publications describing rotational mechanics in rToF [7, 8], we noted that LV apical rotation was independent of RV dilation and RV strain. The LV untwist rate, a measure of early diastolic recoil, was also abnormal in children without significant RV dilation.
We had hypothesized that LV apical rotation would be independent of RV dilation. This finding was also noted by Menting et al. in their study in 82 rToF patients with a mean age of 33 years. They found that reduced apical rotation was associated with larger LV dimensions and decreased biventricular systolic function, but was independent of degree of PR and RV dilation [22]. Reduced LV apical rotation is a surrogate and a preclinical marker for systolic dysfunction [10, 11]. The LV basal rotation has been noted to be reversed or abnormal secondary to the abnormal septal position or RV dysfunction [7, 22]. In our cohort, basal rotation was reversed and this pattern was more prevalent in those with less than mild PR, minimal RV dilation and in those with a non-trans-annular patch repair (group 2). Apical rotation was reduced and also reversed in the same group. RV function in this study as assessed by FAC and strain was normal for both groups of rToF. This suggests that abnormalities in basal and apical rotation precede or are independent of abnormalities in RV size and function in young children.
Prior studies evaluating maturational changes of LV rotational mechanics have demonstrated that the adult pattern of clockwise basal rotation and increased twist and untwist is achieved by adolescence [15, 16, 23]. Apical rotation has been shown to have a preserved counterclockwise pattern throughout and this results in changing of the LV twist from being unidirectional in infancy to a “wringing motion” by early childhood [16, 23]. We saw similar findings in our normal cohort of young children with some still having counterclockwise basal rotation. In our study, children with rToF who had significant PR and RV dilation had clockwise basal rotation, which is opposite to the expected maturational pattern. In contrast, those with less RV dilation had normal expected counterclockwise pattern. One possible explanation is that either the early surgery or the RV dilation resulted in compensatory transition of the LV to achieve a more effective twist. However, apical rotation, which is a surrogate for LV contractility, was also reduced and was more likely to be clockwise (abnormal) in group 2, suggesting that either this is a compensation for counterclockwise basal rotation to preserve the twist or that this pattern of LV remodeling may be more susceptible to developing early LV systolic and diastolic dysfunction.
LV diastolic abnormalities have been described in rToF with restrictive RV physiology and have been attributed to increased RV dimensions [6, 24]. In our study, RV and LV diastolic function was impaired in the entire rToF cohort as assessed by pulsed wave and tissue Doppler imaging. RV restrictive physiology defined by forward atriosystolic flow in the pulmonary artery was noted in only a few patients in the entire cohort. Our study corroborates prior findings of coexistence of both RV and LV diastolic dysfunction when assessed by conventional indices [6] and can be seen even earlier in children < 10 years of age and is independent of type of surgery and RV size.
Untwist is a measure of early diastolic recoil [13]. In our patient cohort abnormal untwist had a strong negative correlation with apical rotation and positive correlation with basal rotation. This supports the concept that systolic and diastolic phases are interdependent and early recognition of either form of dysfunction may be pertinent to long-term outcomes.
There is some debate regarding impairment of LV myocardial mechanics secondary to mechanical dyssynchrony from right bundle branch in rToF [25, 26]. In our study, although the QRS duration was significantly longer in those with dilated RV as expected, the LV rotational abnormalities were in fact more prominent in those without significant RV dilation. We did not find any correlation of the rotational parameters with QRS duration. This finding has been confirmed by another study, in which QRS duration did not correlate with reversed counterclockwise basal rotation on multivariate analysis [7].
We did find age at initial repair to be significantly different, with those with a non-trans-annular patch repaired at mean age of 148 days as compared to trans-annular patch repair who were repaired earlier (mean age of 77 days). Additional studies are required to determine if a later repair has any role in causing the abnormal LV mechanics.
LV dysfunction is independently associated with increased morbidity and sudden death [1,2,3]. This study emphasizes that even in the absence of RV dilation there can be significant abnormalities in the LV contractility and early diastolic recoil. These abnormalities may be inherent in a subset of rToF patients. Early detection with close monitoring of those without significant RV dilation is probably as crucial as it is for those with RV dilation. Further follow-up will be necessary to learn whether early detection and follow-up of rToF patients with abnormal LV rotation in the absence of significantly increased RV size influences long-term outcomes.
Limitations
This is retrospective study with inherent selection bias. Our sample size was small, limiting our ability to perform a multivariate analysis to determine factors causing the abnormal patterns. We acknowledge the limitation of assessing RV volumes accurately by 2D echocardiography, which may add a limitation in purely defining our rToF sub-groups. The reproducibility of the rotational parameters was sub-optimal but could be related to technical reasons and difference in level of experience of the two observers.
Conclusion
This study emphasizes that characterization of LV myocardial mechanics is complex; rotational abnormalities are detected early in rToF and are independent of degree of pulmonary insufficiency, RV dilation, and systolic dysfunction. Abnormalities in apical rotation and untwist rates as measures of LV contractility and early diastolic recoil may present very early after successful ToF repair and are not a result of ventricular interactions. Further longitudinal studies in a larger subset are needed to identify the progression of these abnormalities and their association with clinical outcomes.
References
Valente AM, Gauvreau K, Assenza GE, Babu-Narayan SV, Schreier J, Gatzoulis MA, Groenink M, Inuzuka R, Kilner PJ, Koyak Z, Landzberg MJ, Mulder B, Powell AJ, Wald R, Geva T (2014) Contemporary predictors of death and sustained ventricular tachycardia in patients with repaired tetralogy of fallot enrolled in the INDICATOR cohort. Heart 100:247–253
Geva T, Sandweiss BM, Gauvreau K, Lock JE, Powell AJ (2004) Factors associated with impaired clinical status in long-term survivors of tetralogy of fallot repair evaluated by magnetic resonance imaging. J Am Coll Cardiol 43:1068–1074
Ghai A, Silversides C, Harris L, Webb GD, Siu SC, Therrien J (2002) Left ventricular dysfunction is a risk factor for sudden cardiac death in adults late after repair of tetralogy of fallot. J Am Coll Cardiol 40:1675–1680
Babu-Narayan SV, Diller GP, Gheta RR, Bastin AJ, Karonis T, Li W, Pennell DJ, Uemura H, Sethia B, Gatzoulis MA, Shore DF (2014) Clinical outcomes of surgical pulmonary valve replacement after repair of tetralogy of fallot and potential prognostic value of preoperative cardiopulmonary exercise testing. Circulation 129:18–27
Knauth AL, Gauvreau K, Powell AJ, Landzberg MJ, Walsh EP, Lock JE, del Nido PJ, Geva T (2008) Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of fallot repair. Heart 94:211–216
Friedberg MK, Fernandes FP, Roche SL, Grosse-Wortmann L, Manlhiot C, Fackoury C, Slorach C, McCrindle BW, Mertens L, Kantor PF (2012) Impaired right and left ventricular diastolic myocardial mechanics and filling in asymptomatic children and adolescents after repair of tetralogy of fallot. Eur Heart J Cardiovasc Imaging 13:905–913
Dragulescu A, Friedberg MK, Grosse-Wortmann L, Redington A, Mertens L (2014) Effect of chronic right ventricular volume overload on ventricular interaction in patients after tetralogy of fallot repair. J Am Soc Echocardiogr 27:896–902
Cheung EWY, Liang XC, Lam WWM, Cheung YF (2009) Impact of right ventricular dilation on left ventricular myocardial deformation in patients after surgical repair of tetralogy of fallot. Am J Cardiol 104:1264–1270
Takayasu H, Takahashi K, Takigiku K, Yasukochi S, Furukawa T, Akimoto K, Kishiro M, Shimizu T (2011) Left ventricular torsion and strain in patients with repaired tetralogy of fallot assessed by speckle tracking imaging. Echocardiography 28:720–729
Kim WJ, Lee BH, Kim YJ, Kang JH, Jung YJ, Song JM, Kang DH, Song JK (2009) Apical rotation assessed by speckle-tracking echocardiography as an index of global left ventricular contractility. Circ Cardiovasc Imaging 2:123–131
Toumanidis ST, Kaladaridou A, Bramos D, Skaltsiotes E, Agrios JN, Vasiladiotis N, Pamboucas C, Kottis G, Moulopoulos SD (2013) Apical rotation as an early indicator of left ventricular systolic dysfunction in acute anterior myocardial infarction: experimental study. Hell J Cardiol 54:264–272
Park SJ, Miyazaki C, Bruce CJ, Ommen S, Miller FA, Oh JK (2008) Left ventricular torsion by two-dimensional speckle tracking echocardiography in patients with diastolic dysfunction and normal ejection fraction. J Am Soc Echocardiogr 21:1129–1137
Burns AT, La Gerche A, Prior DL, MacIsaac AI (2009) Left ventricular untwisting is an important determinant of early diastolic function. JACC Cardiovasc Imaging 2:709–716
Sengupta PP, Khandheria BK, Narula J (2008) Twist and untwist mechanics of the left ventricle. Heart Fail Clin 4:315–324
Takahashi K, Al Naami G, Thompson R, Inage A, Mackie AS, Smallhorn JF (2010) Normal rotational, torsion and untwisting data in children, adolescents and young adults. J Am Soc Echocardiogr 23:286–293
Notomi Y, Srinath G, Shiota T, Martin-Miklovic MG, Beachler L, Howell K, Oryszak SJ, Deserranno DG, Freed AD, Greenberg NL, Younoszai A, Thomas JD (2006) Maturational and adaptive modulation of left ventricular torsional biomechanics: Doppler tissue imaging observation from infancy to adulthood. Circulation 113:2534–2541
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK, Lai WW, Geva T (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23:465–495 (quiz 576–7)
Valente AM, Cook S, Festa P, Ko HH, Krishnamurthy R, Taylor AM, Warnes CA, Kreutzer J, Geva T (2014) Multimodality imaging guidelines for patients with repaired tetralogy of fallot: a report from the AmericanSsociety of Echocardiography: developed in collaboration with the Society for Cardiovascular Magnetic Resonance and the Society for Pediatric Radiology. J Am Soc Echocardiogr 27:111–141
Rudski LG, Lai WW, Afilalo J, Hua LQ, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the american society of echocardiography endorsed by the european association of echocardiography, a registered branch of the european society of cardiology, and the canadian society of echocardiography. J Am Soc Echocardiogr 23:685–713
Punn R, Behzadian F, Tacy TA (2010) Annular tilt as a screening test for right ventricular enlargement in patients with tetralogy of fallot. J Am Soc Echocardiogr 23:1297–1302
Nagata Y, Takeuchi M, Mizukoshi K, Wu VCC, Lin FC, Negishi K, Nakatani S, Otsuji Y (2015) Intervendor variability of two-dimensional strain using vendor-specific and vendor-independent software. J Am Soc Echocardiogr 28:630–641
Menting ME, Eindhoven JA, van den Bosch AE, Cuypers JAAE., Ruys TPE, van Dalen BM, McGhie JS, Witsenburg M, Helbing WA, Geleijnse ML, Roos-Hesselink JW (2014) Abnormal left ventricular rotation and twist in adult patients with corrected tetralogy of fallot. Eur Heart J Cardiovasc Imaging 15:566–574
Sengupta PP, Tajik AJ, Chandrasekaran K, Khandheria BK (2008) Twist mechanics of the left ventricle principles and application. JACC Cardiovasc Imaging 1:366–376
Ahmad N, Kantor PF, Grosse-Wortmann L, Seller N, Jaeggi ET, Friedberg MK, Mertens L (2012) Influence of RV restrictive physiology on LV diastolic function in children after tetralogy of fallot repair. J Am Soc Echocardiogr 25:866–873
Fernandes FP, Manlhiot C, Roche SL, Grosse-Wortmann L, Slorach C, McCrindle BW, Mertens L, Kantor PF, Friedberg MK (2012) Impaired left ventricular myocardial mechanics and their relation to pulmonary regurgitation, right ventricular enlargement and exercise capacity in asymptomatic children after repair of tetralogy of fallot. J Am Soc Echocardiogr 25:494–503
Weidemann F, Eyskens B, Mertens L, Dommke C, Kowalski M, Simmons L, Claus P, Bijnens B, Gewillig M, Hatle L, Sutherland GR (2002) Quantification of regional right and left ventricular function by ultrasonic strain rate and strain indexes after surgical repair of tetralogy of fallot. Am J Cardiol 90:133–138
Acknowledgements
The authors would like to acknowledge Zhanna Roytman for data collection and Matthew’s Hearts of Hope Research Grant for financial support that was used towards statistical and Tomtec Software support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mr. Klas is a full time employee of TomTec Imaging Systems. No disclosures for other authors.
Rights and permissions
About this article
Cite this article
Karnik, R., Uppu, S.C., Tozzi, M. et al. Abnormalities in Left Ventricular Rotation Are Inherent in Young Children with Repaired Tetralogy of Fallot and Are Independent of Right Ventricular Dilation. Pediatr Cardiol 39, 1172–1180 (2018). https://doi.org/10.1007/s00246-018-1877-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1877-9