Abstract
The aim of the study is to determine the utility of echocardiography in the assessment of diastolic function in children and young adults with restrictive cardiomyopathy (RCM). RCM is a rare disease with high mortality requiring frequent surveillance. Accurate, noninvasive echocardiographic measures of diastolic function may reduce the need for invasive catheterization. Single-center, prospective, observational study of pediatric and young adult RCM patients undergoing assessment of diastolic parameters by simultaneous transthoracic echocardiogram (TTE) and invasive catheterization. Twenty-one studies in 15 subjects [median (IQR) = 13.8 years (7.0–19.2), 60% female] were acquired with median left ventricular end-diastolic pressure (LVEDP) 21 (IQR 18–25) mmHg. TTE parameters of diastolic function, including pulmonary vein A wave duration (r s = 0.79) and indexed left atrial volume (r s = 0.49), demonstrated significant positive correlation, while mitral valve A (r s = −0.44), lateral e′ (r s = −0.61) and lateral a′ (r s = −0.61) velocities showed significant negative correlation with LVEDP. Lateral a′ velocity (≤0.042 m/s) and pulmonary vein A wave duration (≥156 m/s) both had sensitivity and specificity ≥80% for LVEDP ≥ 20 mmHg. In pediatric and young adult patients with RCM, lateral a′ velocity and pulmonary vein A wave duration predicted elevated LVEDP with high sensitivity and specificity; however, due to technical limitations the latter was reliably measured in 12/21 patients. These noninvasive parameters may have utility in identifying patients that require further assessment with invasive testing. These findings require validation in a multicenter prospective cohort prior to widespread clinical implementation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Restrictive cardiomyopathy (RCM) is a rare and frequently fatal disease, representing 2–5% of all cardiomyopathy cases. Unlike other cardiomyopathies, diagnosis relies on functional classification as opposed to anatomic or morphological features [1, 2]. In the majority of cases, RCM has no identifiable cause, and the range of potentially identifiable etiologies is broad. Primary amyloidosis has been recognized as a cause of RCM, along with other systemic diseases, while environmental exposures such as radiation therapy and chemotherapy have also been implicated. The genetics of RCM are only starting to be investigated, and there can be clinical overlap with other types of cardiomyopathy, including hypertrophic cardiomyopathy [1].
Because the diagnostic criteria for RCM are functional or physiologic in nature, care decisions often focus on longitudinal changes in invasive measures of function. Systolic performance, as measured by conventional transthoracic echocardiography (TTE) indices such as ejection fraction, is generally preserved throughout the disease course. Diastolic function, on the other hand, deteriorates progressively and often rapidly as a hallmark of the diagnosis [1]. Unlike assessment of systolic function, diastolic function is more difficult to assess noninvasively and has limited evidence validating its role in most pediatric disease states.
Cardiac catheterization and TTE are two important tools in the diagnosis and monitoring of diastolic function in patients with RCM. Given the need for serial assessment of diastolic function in this patient population, a reliable noninvasive approach to evaluation would reduce patient burden while providing valid data to monitor disease progression. Although cardiac catheterization is the gold standard for determination of diastolic parameters, TTE is the preferred method for serial assessment of adult RCM patients given its noninvasive nature [3–9]. Importantly, RCM pathophysiology observed in adult-onset disease may not be characteristic of pediatric and adolescent disease, as the etiologies of myocardial disease may differ between these groups [10–12]. In this prospective study, we sought to characterize the relationship between invasive and TTE-derived noninvasive measures of diastolic function in pediatric and young adult patients with RCM.
Methods
Patient Enrollment
This was a single-center, prospective, observational study of pediatric and young adult patients with RCM enrolled from August 2012 to May 2014. Eligible patients were those previously diagnosed with genetically determined or familial RCM and followed in a specialty cardiomyopathy clinic at Cincinnati Children’s Hospital Medical Center. Patients referred for clinically indicated hemodynamic catheterization were approached for study enrollment, and parents and/or patients provided written informed consent and/or assent, depending on the age of the patient. The Cincinnati Children’s Hospital Medical Center Institutional Review Board approved this study.
Echocardiography and Cardiac Catheterization
Enrolled subjects underwent routine invasive assessment with cardiac catheterization and simultaneous TTE, performed immediately following acquisition of the invasive hemodynamic data. Care was taken not to alter the steady-state conditions between invasive and noninvasive assessments, i.e., sedation/anesthesia was not altered until all data were acquired. Procedural sedation or anesthesia was provided according to the institutional clinical protocol and optimized for the individual patient. Cardiac catheterization was performed according to the standard institutional clinical protocol. Right and left heart catheterization was performed using fluid-filled catheters and digital transducers, without exposure to radiographic contrast. Cardiac output was determined by Fick and thermodilution methods, utilizing either measured or assumed oxygen consumption [13]. Echocardiography was performed using a Phillips iE33 machine (Phillips Medical Systems, Best, The Netherlands), and quantification performed according to published guidelines [14]. The TTE measures of diastolic function included: left atrial volume, indexed (ml/m2); pulmonary vein A wave duration (m/s−1); pulmonary vein S:D; mitral valve E velocity (m/s); mitral valve A velocity (m/s); mitral valve E:A; mitral valve lateral e′ velocity (m/s); mitral valve lateral a′ velocity (m/s); mitral valve septal e′ velocity (m/s); mitral valve septal a′ velocity (m/s); mitral valve lateral E:e′; mitral valve septal E:e′; and left ventricular isovolumic relaxation time (m/s−1). Myocardial tissue measurements were taken using color Doppler imaging, while all other values were spectral Doppler. Subjects with more than one cardiac catheterization during the study period underwent simultaneous catheterization and TTE studies on each occasion. Repeat studies were separated by a minimum of 6 months in all cases.
Statistical Analysis
Two readers (PCM and RAM) analyzed all echocardiographic studies, and a single reviewer (BHG) analyzed all invasive hemodynamic studies. Reviewers were blinded to clinical and outcome data. Descriptive statistics were provided for study characteristics. Spearman correlation coefficients were examined between LVEDP, and each of the echocardiographic measures detailed above. Inter-observer variability in echocardiographic measurements was assessed for measures found to have a significant correlation with LVEDP. The inter-observer relationship was presented as an intra-class correlation coefficient. Area under the curve was examined by plotting receiver operating characteristic (ROC) curves between clinically significant LVEDP elevation and echocardiographic measures that showed significant correlations with LVEDP. Sensitivity analyses were conducted to assess whether multiple echocardiographic parameters could be combined to improve ROC performance. The level of significance for all statistical tests was two-sided with p ≤ 0.05. All analyses were performed using SAS version 9.3 (Cary, NC, USA).
Results
Patient Demographics and Study Data
Twenty-one simultaneous catheterization and TTE studies were performed in 15 RCM subjects. Patients had a median age of 13.8 [interquartile range (IQR) 7–19.2] years, with 60% female (Table 1). Systolic function (as measured by shortening fraction and ejection fraction on TTE) and cardiac index (thermodilution) were normal for all participants (Table 2). The median LVEDP was elevated at 21 (IQR 18–25) mmHg.
Correlation of Echocardiographic Indices and Left Ventricular End-Diastolic Pressure
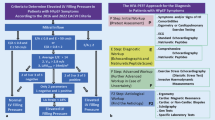
The coefficients of correlation between LVEDP- and TTE-derived measures of diastolic function are displayed in Table 3 and Fig. 1. Among the TTE parameters, pulmonary vein A wave duration (r s = 0.79) and indexed left atrial volume (r s = 0.49) demonstrated significant positive correlation with LVEDP. Due to technical limitations including artifact and background noise contaminating the signal, measurement of a reliable pulmonary vein A wave duration was achieved in only 12 of the 21 patients in which it was attempted. Mitral valve A (r s = −0.44), lateral e′ (r s = −0.61) and lateral a′ (r s = −0.61) velocities showed significant negative correlation with LVEDP. Inter-observer correlation for each of these TTE parameters was very strong, ranging from 0.88 to 0.99 (Supplement Table 1). There was no significant correlation between LVEDP and the following: mitral valve E velocity; mitral valve E:A; mitral valve septal e′ or a′ velocity; mitral valve E:e′; pulmonary vein S:D; or isovolumic relaxation time.
Correlation of left ventricular end-diastolic pressure (LVEDP) and select echocardiographic parameters. The intersection of the superimposed lines represent cutoff values to detect LVEDP ≥ 20 mmHg at sensitivity = 80% based on data from receiver operating characteristic curves. FN false negative, FP false positive, TN true negative, TP true positive
Selection of Echocardiographic Indices that Best Predict Elevated Left Ventricular End-Diastolic Pressure
Receiver operating characteristic curves were created for the echocardiographic measurements demonstrated to have significant correlation with LVEDP (Fig. 2). Cutoff values for echocardiographic parameters were generated to allow for detection of LVEDP ≥ 20 mmHg at a sensitivity of at least 80%. Values delineated included: left atrial volume ≥41 ml/m2; mitral valve A wave velocity ≤0.51 m/s; lateral e′ wave velocity ≤0.083 m/s; lateral a′ wave velocity ≤0.042 m/s; and pulmonary vein A wave duration ≥156 m/s (Fig. 1; Table 4). Lateral a′ velocity and pulmonary vein A wave duration cutoff values also demonstrated a specificity ≥80% for LVEDP ≥ 20 mmHg. All parameters tested had area under the curve ≥0.75, with lateral e′ velocity, lateral a′ velocity and pulmonary vein A wave duration all >0.8 (Fig. 2; Table 4). Sensitivity analyses combining pulmonary vein A wave duration and left atrial volume did not improve the area under the curve compared with pulmonary vein A wave duration alone (data not shown); other combinations could not be stably modeled.
Discussion
In the present study, we investigated the utility of TTE-derived diastolic parameters in the assessment of diastolic function and restrictive physiology in a cohort of children and young adults with RCM, utilizing a prospective comparative TTE-catheterization approach. We identified 5 candidate TTE measures that showed a significant correlation with LVEDP in the clinically predicted manner. Pulmonary vein A wave duration and indexed left atrial volume had significant positive correlation with LVEDP, suggesting abnormal filling pressure in the left atrium. Pulmonary vein A wave duration was limited by inability to achieve a reliable signal in all patients for which it was attempted. Using ROC analyses, cutoff values were generated for potential use as noninvasive surrogates of LVEDP ≥ 20 mmHg. Mitral valve A and lateral e′ and a′ velocity showed significant negative correlation with LVEDP, indicating abnormal ventricular filling and relaxation. All 5 measures demonstrated excellent inter-observer correlation. To our knowledge, this is the first study in pediatric and young adult RCM patients to demonstrate important potential utility of TTE measures to noninvasively evaluate changes in LVEDP. These parameters could be used in conjunction with other markers of disease progression in RCM (serum biomarkers, symptoms) to determine whether additional studies, including invasive hemodynamics, are warranted.
Echocardiographic Indices with Utility in Pediatric and Young Adults Patients with Restrictive Cardiomyopathy
Weller et al. [15] previously described 18 pediatric patients with idiopathic RCM, in which LVEDP ranged from 14 to 40 mmHg with all but 2 being ≥20 mmHg. Four of those patients presented with low cardiac output and 14 developed low cardiac output during follow-up, with the average LVEDP 27 mmHg (range 16–40 mmHg). Based on these data, we attempted to pick a clinically important cutoff value for LVEDP that would warrant further invasive investigation, and thus chose a threshold set at LVEDP ≥ 20 mmHg for correlation studies. However, this is not to imply that we consider LVEDP <20 mmHg to be normal or not of concern, rather we wanted to identify noninvasive parameters at which we might change clinical course, e.g., obtain invasive data, in patients already known to have RCM and restrictive physiology. Moreover, for a patient with longstanding LVEDP >20 mmHg, meeting these echocardiographic criteria might not carry the same weight as in a patient previously <20 mmHg. Once invasive hemodynamic data are sought, additional factors such as pulmonary vascular resistance and cardiac index would be combined with end-diastolic pressure data to determine future clinical course, including whether evaluation for heart transplant is warranted.
In a prior study correlating invasively measured hemodynamics and TTE-derived diastolic parameters in pediatric patients with a variety of congenital heart disease diagnoses, Border et al. [16] demonstrated that pulsed Doppler indices correlated with Tau but not LVEDP, while color M-mode and Doppler tissue indices were correlated with LVEDP, although weakly in the case of the latter. In the current study, early diastolic filling (mitral valve E wave) was not affected while late filling (mitral valve A wave) was possibly explaining why the ratios of mitral E:A and mitral E:lateral e′ were not significant. One of the classic hemodynamic findings in RCM is a “square root sign” in the LVEDP waveform, suggesting the presence of poor ventricular compliance, which is represented by mitral valve a wave velocity [9]. The difference between Doppler tissue values of the septal versus lateral mitral valve was also noted and may be a result of the fact that the right ventricle, which for anatomic reasons affects the medial tissue Doppler signal did not manifest the same correlations, relative to RVEDP, as found on the left side. The latter result contrasts with the findings by Savage and Goldberg [10, 17], although those studies were performed in pediatric patients following cardiac transplantation, representing a distinct population from this RCM cohort.
Our data match prior studies of echocardiographic parameters of diastolic function in finding that no single TTE parameter is able to substitute for invasively measured ventricular diastolic function. In fact, we were unable to show significant correlation between LVEDP and echocardiographic parameters traditionally thought to be predictive for RCM (i.e., deceleration time, mitral valve E:A ratio, isovolumic relaxation time and mitral valve E:e′) [9]. However, in identifying multiple TTE measures that predictably correlate highly with LVEDP (defined as ≥20 mmHg), we believe that TTE can be utilized to triage pediatric and young adult RCM patients, to parse out those that may benefit from further investigation, including invasive hemodynamic assessment, from those that may be followed noninvasively. In particular, the cutoff values of lateral a′ velocity ≤0.042 m/s and pulmonary vein A wave duration ≥156 m/s both had high sensitivity and specificity for LVEDP ≥ 20 mmHg, making them potentially useful measures to noninvasively identify patients with a clinically significant elevation in LVEDP. Unfortunately, the reliability of obtaining pulmonary vein A wave duration was not complete, with only 12 of 21 studies demonstrating a signal thought to be appropriate for analysis. The other parameters evaluated by this method (mitral valve A velocity, lateral e′ velocity and left atrial volume) had lower specificity when sensitivity was maximized, and would therefore not be as useful in a clinical setting.
Restrictive Cardiomyopathy in Pediatric and Young Adult Patients
Pediatric and young adult patients with RCM present a management dilemma. While natural history data demonstrate a high 5-year mortality that is greatly improved by transplantation [1, 2], the current predicted half-life of the graft in pediatric and adolescent age groups is 15–20 years depending on age at, and indication for, transplantation [18]. Further, recent data suggest that a significant portion of the sudden deaths experienced by the RCM population is arrhythmic in nature and thus may be modifiable by use of implantable cardiac defibrillators [19]. Such a therapy might reduce the rate of sudden death and facilitate a delayed cardiac transplantation evaluation. As such, defining a reliable noninvasive means to track hemodynamic progression of disease could prove useful, allowing patients deferring transplantation an improved quality of life with reduced burden of serial invasive catheterization procedures while reducing the risk of missing hemodynamically significant disease progression.
Prior Validation of Echocardiographic Diastolic Parameters
Early validation studies of simultaneous echocardiographic and invasive measures to assess left ventricular diastolic function investigated left ventricular inflow pattern (mitral valve E and A waves) in adult patients undergoing clinical cardiac catheterization, including those with coronary artery disease, congestive heart failure and RCM [3]. Left ventricular inflow pattern was affected by hemodynamics more than by any particular disease process, and typical Doppler inflow patterns of diastolic dysfunction were described. Subsequently, Doppler tissue imaging of the mitral valve annulus (mitral valve e′) was shown to behave as a preload-independent measure of diastolic function, with the mitral E/e′ correlating with the pulmonary capillary wedge pressure, a right heart surrogate of LVEDP [4, 5]. Reports that followed over the last 15 years have described the utility of left ventricular inflow, tissue Doppler imaging of the mitral valve, left ventricular isovolumic relaxation time, and various mathematical ratios of these characteristics in predicting LVEDP across a variety of disease states in adult patients [6–8, 20, 21].
Echocardiographic Diastolic Indices in Pediatric and Adolescent Patients
Despite multiple reports validating noninvasive parameters of diastolic function in adults, there is evidence that in certain populations the correlation between invasive and noninvasive measures is poor. For example, in symptomatic hypertrophic cardiomyopathy patients, although there is an overall correlation between TTE parameters and directly measured LVEDP, the noninvasive measures do not accurately predict LVEDP in an individual patient [22]. Moreover, in contrast to the evidence from myriad studies in adult populations, the validation of TTE diastolic measures in pediatric and adolescent populations has been more challenging. Savage et al. [10] demonstrated mitral valve E:e′ to be a poor predictor of pulmonary capillary wedge pressure in pediatric patients status post-cardiac transplantation. Meanwhile, in the same population, Goldberg et al. [17] showed that septal E:e′ values above a certain threshold were associated with increased pulmonary capillary wedge pressure, as were lateral tricuspid E:e′ values and mean right atrial pressure. In an attempt to apply adult guidelines defining left ventricular diastolic dysfunction to a pediatric population, Dragulescu et al. [11] found the echocardiographic values used for adults were not informative in following pediatric patients, and agreement among multiple experienced investigators was low. This evaluation included a number of patients with RCM. In contrast, our study found high inter-observer correlation for TTE measurements found to have potential clinical use (i.e., those with strong correlation to LVEDP), strengthening the argument for their inclusion in routine noninvasive evaluation of pediatric and young adult patients with RCM. Sasaki et al. [12] evaluated the utility of adult parameters in a large cohort of pediatric RCM patients and found the echocardiographic values to have very poor sensitivity in identifying left ventricular restrictive physiology and concluded there is a need to develop pediatric specific guidelines for evaluation by TTE. The role of TTE in identifying right ventricular diastolic dysfunction in pediatric patients has more support. Significant correlation between TTE-derived right ventricular diastolic parameters and those derived by high-fidelity micromanometer pressure catheter was demonstrated in populations of pediatric patients with pulmonary arterial hypertension and following heart transplantation [17, 23]. It is notable that our study showed no significant correlation between RVEDP and the TTE parameters measured.
Limitations
Despite the prospective and protocoled nature of this investigation, several important limitations were present. First, the low prevalence of pediatric RCM and the single-center nature of this study led to inclusion of a modest sample size. Furthermore, there are some inherent technical challenges with TTE that limit acceptable imaging windows and can affect reliable acquisition of images for accurate measurements. This was most evident with the pulmonary vein A wave duration, with 9 studies not having quality deemed good enough to obtain a reliable measurement despite an attempt having been made to record the tracing. Reliable measurements of pulmonary vein tracings can be challenging in older and larger patients due to size, artifact and background noise contaminating the signal. Whether additional time spent obtaining the tracing would improve capture of a clear signal is worth consideration with the knowledge that it may have particular utility. Another potential criticism is that several patients underwent more than 1 procedure, with data from each procedure included in this series. Given that the primary aim of this study was to relate noninvasive TTE measures to invasive measures of diastolic function, and not generate a cross-sectional report of RCM patients, this inclusion should not introduce bias. Finally, the lack of inclusion of patients with normal diastolic function precludes extrapolation of the data presented herein to a non-RCM population. That is to say, this study provides empiric evidence for the clinician as they approach the decision whether or not to invasively study the patient with RCM and evolving diastolic dysfunction; it does not provide evidence to support this decision making in other populations, including those with suspected but not yet proven restrictive physiology.
Conclusion
In the present study, we demonstrate that lateral a′ velocity and pulmonary vein A wave duration are noninvasive measures of diastolic function that could potentially serve as important screening measures to identify RCM patients at risk for an LVEDP ≥ 20 mmHg. Those patients found to be at risk would deserve further evaluation, including consideration of standard catheterization techniques to measure LVEDP as well as other parameters useful in assessing this population such as pulmonary vascular resistance. Using this stepwise clinical approach to follow-up of patients with RCM could reduce cost and patient risk while improving quality of life without adversely impacting long-term outcomes. These findings require validation in a multicenter prospective cohort prior to widespread clinical implementation.
Abbreviations
- IQR:
-
Interquartile range
- LVEDP:
-
Left ventricular end-diastolic pressure
- RCM:
-
Restrictive cardiomyopathy
- ROC:
-
Receiver operating characteristic
- RVEDP:
-
Right ventricular end-diastolic pressure
- TTE:
-
Transthoracic echocardiogram
References
Denfield SW, Webber SA (2010) Restrictive cardiomyopathy in childhood. Heart Fail Clin 6:445–452 (viii)
Webber SA, Lipshultz SE, Sleeper LA, Lu M, Wilkinson JD, Addonizio LJ, Canter CE, Colan SD, Everitt MD, Jefferies JL, Kantor PF, Lamour JM, Margossian R, Pahl E, Rusconi PG, Towbin JA, Pediatric Cardiomyopathy Registry I (2012) Outcomes of restrictive cardiomyopathy in childhood and the influence of phenotype: a report from the pediatric cardiomyopathy registry. Circulation 126:1237–1244
Appleton CP, Hatle LK, Popp RL (1988) Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 12:426–440
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Nagueh SF, Lakkis NM, Middleton KJ, Spencer WH 3rd, Zoghbi WA, Quinones MA (1999) Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation 99:254–261
Diwan A, McCulloch M, Lawrie GM, Reardon MJ, Nagueh SF (2005) Doppler estimation of left ventricular filling pressures in patients with mitral valve disease. Circulation 111:3281–3289
Kasner M, Westermann D, Steendijk P, Gaub R, Wilkenshoff U, Weitmann K, Hoffmann W, Poller W, Schultheiss HP, Pauschinger M, Tschope C (2007) Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 116:637–647
Arteaga RB, Hreybe H, Patel D, Landolfo C (2008) Derivation and validation of a diagnostic model for the evaluation of left ventricular filling pressures and diastolic function using mitral annulus tissue Doppler imaging. Am Heart J 155:924–929
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Savage A, Hlavacek A, Ringewald J, Shirali G (2010) Evaluation of the myocardial performance index and tissue doppler imaging by comparison to near-simultaneous catheter measurements in pediatric cardiac transplant patients. J Heart Lung Transplant 29:853–858
Dragulescu A, Mertens L, Friedberg MK (2013) Interpretation of left ventricular diastolic dysfunction in children with cardiomyopathy by echocardiography: problems and limitations. Circ Cardiovasc Imaging 6:254–261
Sasaki N, Garcia M, Ko HH, Sharma S, Parness IA, Srivastava S (2015) Applicability of published guidelines for assessment of left ventricular diastolic function in adults to children with restrictive cardiomyopathy: an observational study. Pediatr Cardiol 36:386–392
Seckeler MD, Hirsch R, Beekman RH 3rd, Goldstein BH (2014) Validation of cardiac output using real-time measurement of oxygen consumption during cardiac catheterization in children under 3 years of age. Congenit Heart Dis 9:307–315
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK, Lai WW, Geva T (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23:465–495 (quiz 576-467)
Weller RJ, Weintraub R, Addonizio LJ, Chrisant MR, Gersony WM, Hsu DT (2002) Outcome of idiopathic restrictive cardiomyopathy in children. Am J Cardiol 90:501–506
Border WL, Michelfelder EC, Glascock BJ, Witt SA, Spicer RL, Beekman RH 3rd, Kimball TR (2003) Color M-mode and Doppler tissue evaluation of diastolic function in children: simultaneous correlation with invasive indices. J Am Soc Echocardiogr 16:988–994
Goldberg DJ, Quartermain MD, Glatz AC, Hall EK, Davis E, Kren SA, Hanna BD, Cohen MS (2011) Doppler tissue imaging in children following cardiac transplantation: a comparison to catheter derived hemodynamics. Pediatr Transplant 15:488–494
Dipchand AI, Edwards LB, Kucheryavaya AY, Benden C, Dobbels F, Levvey BJ, Lund LH, Meiser B, Yusen RD, Stehlik J, International Society of H, Lung T (2014) The registry of the International Society for Heart and Lung Transplantation: seventeenth official pediatric heart transplantation report—2014. J Heart Lung Transplant 33:985–995
Walsh MA, Grenier MA, Jefferies JL, Towbin JA, Lorts A, Czosek RJ (2012) Conduction abnormalities in pediatric patients with restrictive cardiomyopathy. Circ Heart Fail 5:267–273
Dagdelen S, Eren N, Karabulut H, Akdemir I, Ergelen M, Saglam M, Yuce M, Alhan C, Caglar N (2001) Estimation of left ventricular end-diastolic pressure by color M-mode Doppler echocardiography and tissue Doppler imaging. J Am Soc Echocardiogr 14:951–958
Mi YP, Abdul-Khaliq H (2013) The pulsed Doppler and tissue Doppler-derived septal E/e’ ratio is significantly related to invasive measurement of ventricular end-diastolic pressure in biventricular rather than univentricular physiology in patients with congenital heart disease. Clin Res Cardiol 102:563–570
Geske JB, Sorajja P, Nishimura RA, Ommen SR (2007) Evaluation of left ventricular filling pressures by Doppler echocardiography in patients with hypertrophic cardiomyopathy: correlation with direct left atrial pressure measurement at cardiac catheterization. Circulation 116:2702–2708
Okumura K, Slorach C, Mroczek D, Dragulescu A, Mertens L, Redington AN, Friedberg MK (2014) Right ventricular diastolic performance in children with pulmonary arterial hypertension associated with congenital heart disease: correlation of echocardiographic parameters with invasive reference standards by high-fidelity micromanometer catheter. Circ Cardiovasc Imaging 7:491–501
Acknowledgements
The authors wish to acknowledge support from the Heart Institute Research Core, as well as the dedicated sonographers and cardiac catheterization laboratory personnel who made performance of this study possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TD Ryan, PC Madueme, JL Jefferies, EC Michelfelder, JA Towbin, JG Woo, RD Sahay, EC King, R Brown, RA Moore, MA Grenier, BH Goldstein declares that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
Intra-class correlation coefficient (ICC) for selected echocardiogram values. Measurement of ICC was taken in 10 studies (47%). Higher values represent stronger agreement, with 0.0–0.2 indicating very little agreement, 0.2–0.4 little agreement, 0.4–0.6 moderate agreement, 0.6–0.8 strong agreement and 0.8–1.0 very strong agreement (DOCX 11 kb)
Rights and permissions
About this article
Cite this article
Ryan, T.D., Madueme, P.C., Jefferies, J.L. et al. Utility of Echocardiography in the Assessment of Left Ventricular Diastolic Function and Restrictive Physiology in Children and Young Adults with Restrictive Cardiomyopathy: A Comparative Echocardiography-Catheterization Study. Pediatr Cardiol 38, 381–389 (2017). https://doi.org/10.1007/s00246-016-1526-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1526-0