Abstract
Retrograde intrarenal surgery (RIRS) is highly successful at eliminating renal stones of various sizes and compositions. As urologists are taking on more complex procedures using RIRS, this has led to an increase in operative (OR) times. Our objective was to determine the best predictor of OR time in patients undergoing RIRS. We retrospectively reviewed the records of patients undergoing unilateral RIRS for solitary stones over a 10 year time span. Stones were fragmented and actively extracted using a basket. Variables potentially affecting OR time such as patient age, sex, BMI, lower pole stone location, volume, Hounsfield units (HU), composition, ureteral access sheath (UAS) use, and pre-operative stenting were collected. Multivariable linear and stepwise regression was used to evaluate the predictors of OR time. There were 118 patients that met inclusion criteria. The median stone volume was 282.6 mm3 (IQR 150.7–644.7) and the mean OR time was 50 min (±25.9 SD). On univariate linear regression, stone volume had a moderate correlation with OR time (y = 0.022x + 38.2, r 2 = 0.363, p < 0.01). On multivariable stepwise regression, stone volume had the strongest impact on OR time, increasing time by 2.0 min for each 100 mm3 increase in stone volume (p < 0.001). UAS added 13.5 (SE 3.9, p = 0.001) minutes and renal lower pole location added 9 min (SE 4.3, p = 0.03) in each case they were used. Pre-operative stenting, HU, calcium oxalate stone composition, sex, and age had no significant effect on OR time. Amongst the main stone factors in RIRS, stone volume has the strongest impact on operative time. This can be used to predict the length of the procedure by roughly adding 2 min per 100 mm3 increase in stone volume.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Urolithiasis is a common condition in the United States with an overall prevalence of 8.8 % [1]. Retrograde intrarenal surgery (RIRS) is highly successful at eliminating renal stones of various sizes as well as various compositions [2]. The evolving usage of RIRS for difficult stone cases merits investigation into the various factors involved in complexity.
The complexity and difficulty of a case is reflected by the operative room (OR) time [3, 4]. Previous studies have shown individually how location, size, Hounsfield units (HU), composition, ureteral access sheath (UAS) use, and pre-operative stenting affect OR time. A recent study by Ito et al. [5] evaluated these factors together to determine that stone volume was the most significant parameter prolonging OR time. Our objective was to confirm the findings from this single-center analysis as well as to expand on the OR time increases seen with increasing stone volumes. This information could be used to improve the efficiency in the operating room in terms of surgical scheduling.
Materials and methods
After obtaining institutional review board approval, we retrospectively reviewed the charts of consecutive patients undergoing RIRS for renal stones by one urologist specializing in urolithiasis for over 10 years from January 2005 to February 2014. We found 1199 patients available for review. Our inclusion criteria were strict to make for uniform comparisons. We included only unilateral procedures for solitary stones that achieved stone-free status on one single procedure. Patients also must have had pre-operative non-contrast computed tomography (NCCT) scans within 3 months of RIRS. Patients undergoing bilateral RIRS or other concurrent endourologic procedures were also excluded.
The renal stones were defined as stones proximal to the UPJ according to their position documented on the operative report. NCCT scans were independently reviewed by a radiologist blinded to stone composition and stone volume on magnified bone windows using 1.25 mm sliced reconstruction [6]. Stone volume was calculated using the formula π/6 × L × W × H. HU were determined by the average attenuation coefficients measured by placing a freehand region of interest along the inner contours of the stone margins. The OR time was calculated from the procedure start and stop time. Stone-free status was defined as no evidence of residual stones of the ipsilateral collecting system on follow-up imaging with renal ultrasonography and/or plain abdominal films at 2–4 weeks.
Our surgical technique involved use of only a 7.5Fr flexible ureteroscope (Flex-X™, Flex-X2™, Karl Storz, Germany). A retrograde pyelogram was obtained in all cases. Coaxial dilators (8/10Fr) were routinely used to pass the second wire as the safety wire. Ureteral access sheaths (11/13Fr Microvasive or 12Fr Applied Medical) were placed at the discretion of the attending surgeon and were mostly based on the stone volume and whether the ureter safely allowed for passage. The laser settings for power were 0.8–1.0 J and rate 8–10 Hz. Stone fragments were actively retrieved with a 1.9Fr ZeroTip nitinol basket (Boston Scientific, Natick, MA). Successful clearance was determined when all residual fragments were <2 mm by using the diameter of the laser fiber as a rough guide. A double-J ureteral stent was placed at the end of all procedures. Stones were sent to The Lab for Stone Research (Newton, MA) for composition analysis. Stones that were composed of >60 % of the major constituent was given that designation. All others were considered mixed.
Linear regression models were used to evaluate predictors of OR time. Multivariable stepwise regression was used to evaluate the most significant predictors of OR time. STATA v11.0 (College Station, Texas) was used to perform the statistical analysis.
Results
There were 118 patients that met the inclusion criteria. The demographics of the cohort are listed in Table 1. There were slightly more females vs. males for this cohort (58 vs. 42 %). The median stone volume was 282.6 mm3 (IQR 150.7–644.7) and the mean OR time was 50 min (±25.9 SD). UAS was used in 41 % of the cases, pre-operative stents were placed in 31 % of cases, and both were placed in 16 % of cases. Stone composition analysis was only available in 75 patients (64 %). There were seven different stone compositions (Table 2) with calcium oxalate monohydrate being the most common. Uric acid stones were not only larger (1758.5 mm3) than both calcium oxalate monohydrate (424.2 mm3) and dihydrate (300.0 mm3) stones, but also required more operative time (91.3 vs. 50.2 and 32.8 min, respectively, p < 0.01).
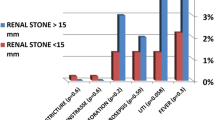
On linear regression analysis, operative times significantly increased with larger stone volumes (Fig. 1, y = 0.022x + 38.2, r 2 = 0.363, p < 0.01). Pre-operative stenting shown in Fig. 2 was not associated with lower operative times (p = 0.63). Use of a UAS did have a significant increase on operative times shown in Fig. 3 (y = 0.02x + 46.4, r 2 = 0.389). This may have been confounded with use of UAS mostly with larger stones (336.5 vs. 835.7 mm3, p < 0.001).
Linear regression analysis comparing operative time to stone volume by pre-operative stenting. The blue solid line represents the patients who were pre-stented (y = 0.027x + 38.5, r 2 = 0.186). The black dashed lines represents the patients who were not pre-stented (y = 0.022x + 37.4, r 2 = 0.433). Pre-stenting did not make a significant difference on operative time (p = 0.63)
Linear regression analysis comparing operative time to stone volume by use of an access sheath. The dashed line represents the patients with a UAS (y = 0.02x + 46.4, r 2 = 0.389). The solid line represents the patients who did not have a UAS (y = 0.01x + 37.4, r 2 = 0.07). Ureteral access sheath use did significantly increase operative time (p < 0.001)
Analyzing all the stone factors on multivariable linear regression, stone volume and lower pole location were significant predictors of increased operative time (Table 3). Age, BMI, sex, pre-operative stenting, HU, and calcium monohydrate stone composition did not have a significant effect on operative time. On multivariable stepwise regression, stone volume had the strongest impact on operative time, increasing time by 2.0 min for each 100 mm3 increase in stone volume (p < 0.001). Stones in the lower pole added 9 min (SE 4.3, p = 0.03) in each case they were used. UAS was found to be only significant in the stepwise model and added 13.5 (SE 3.9, p < 0.001) minutes for each case.
Discussion
Operative time can be used as a measure of operative difficulty and complexity [3, 4]. While this can certainly reflect increased complications with increased operative time as shown in our data, it was not the focus in our study. Most surgeons who book and perform RIRS cases intuitively know that increased stone volume will lead to a longer operation. This notion was also recently confirmed by a retrospective analysis by Ito et al. [5] who showed that larger stone volume, lower experience level of the surgeon, higher HU, and lack of pre-operative stenting all contributed to increasing OR time. But exactly how much longer was the driving force behind our study. With our large cohort, we show for the first time that adding approximately 2 min per each 100 mm3 increase in stone volume will provide a good estimate of time required to perform RIRS. While stone volume is often not reported on NCCT, it is a relatively simple and more representative measure of true stone burden compared to the 1-dimensional maximum axial measurement that is often given [7]. This is important information in scheduling the cases and effective use of operating room time to improve the quality of care.
Previous studies on operative time for ureteroscopy have mostly assessed stone size instead of stone volume. While the results may not be totally applicable given that one 10 cm stone may have a drastically different stone volume compared to another 10 cm stone [7], the findings are still interesting to note. Deters et al. [8] previously showed that stone location had a significant impact on operative time. They retrospectively reviewed 213 cases (115 ureteral stone and 98 renal stones). Renal stones required a significantly increased mean operative time (112 min) than did the ureteral stones (70 min; p < 0.001). Amongst ureteral stones, the proximally located stones required a significantly longer operative time compared to the distally located ones (87 vs. 58 min, respectively; p < 0.001). The stone size was predictive of the operative time in both groups (renal r 2 = 0.2691, ureteral r 2 = 0.3227), and this was significant only in the ureteral cohort (p = 0.0432). In their series, renal stones (11.3 mm) were larger than the ureteral stones (7.7 mm), yet in a separate analysis for size-matched comparison, renal stones required a longer operative time than did their ureteral counterpart (104 vs. 74 min; p < 0.0001). Pre-operative stenting was more common in renal cases, yet had longer operative times. The authors conclude that location is the most significant factor rather than size or pre-operative stenting.
Our study only looked at renal stones and those patients with ureteral stones were excluded given that the comparison between the two groups would require comparing a semi-rigid to a flexible instrument. However, within the renal stone cohort we evaluated the effects of the lower pole stone location and not surprisingly found that this variable did increase operative time for these cases. The lower pole stone can be considered a clinical challenge especially with a longer lower pole infundibulum and the deflection limitation seen when the working channel is used [9, 10]. A nitinol basket may be used to reposition the stone toward locations where fragmentation is easier [11]. Although, we did not use this technique in our series, it would certainly increase the time needed to perform RIRS by adding an extra step. Jacquemet et al. [10] compared ureteroscopy for lower pole stones (n = 232) versus stones in locations other than lower pole (n = 139) and found the efficacy and morbidity were not impacted by stone location. The authors did find the duration of the procedure did not differ between the two groups; however, since the groups combined multiple stones per renal unit as well as the use of basket repositioning for lower pole stones, it is hard to draw definitive conclusions. Our inclusion criteria were strict to only look at single stones and maybe a more realistic representation.
Ureteral access sheaths provide repetitive access to the upper tract, decreased intrarenal pressures, and improved visibility and clearance of small stone fragments [12]. The effect on operative time was previously looked at by Kourambas et al. [13] in a prospective randomized cohort of 47 patients undergoing ureteroscopy for both renal and ureteral stones. Although the mean stone burden in UAS group was larger (13.7 vs. 10.1 mm), the mean OR time was actually 10 min shorter (p < 0.05). On the contrary, we actually found that UAS increased OR time; adding on average 13.5 min (p < 0.001) in each procedure it was used. The discrepancy in our findings may be from our larger cohort with UAS compared to the previous study (48 vs. 23 patients, respectively) Furthermore, the presence of a UAS may make surgeons take extra time to clear out all fragments. Nonetheless, we feel the benefits of the UAS itself are much more important than its effects on operative time to warrant its use on larger stones.
Wiener et al. [14] looked at whether stone composition had any effects on operative time. This study looked at 187 ureteroscopy cases and measured operating room time per gram of stone removed of various soft and hard crystalline compositions in vivo. The authors found no statistical significance on stone composition and operating room time using the holmium: YAG laser for fragmentation. However, the study was limited by a small sample size, and using patients that had staged procedures which could have effected OR time.
Hounsfield units have been shown to be a good predictor of stone composition both in vitro and in vivo. Using this principle of HU, Ito et al. [15] showed that increased HU on NCCT scans lead to significantly longer OR times for stones <20.0 mm. The authors retrospectively analyzed 219 cases and found that when maximum HU exceeded 1389, OR times were on average 29.4 min longer. However, when stone burden ≥20.0 mm, there was no statistical significant difference in OR times. While a harder stone such as brushite may have longer OR time compared to a calcium stone individually, we found that neither HU nor calcium stone composition were good predictors of OR time on multivariable analysis. Again, it appears that it is the stone volume rather than composition that is driving the overall increase in the OR time.
Pre-operative stenting did not have an association with decreased OR times in our study. Patients may have had different durations of indwelling stent time and this may have impacted the degree of dilation making non uniform comparisons. A recent retrospective review by Chu et al. [16] looked at 104 patients who underwent ureteroscopy for both renal and ureteral stones (45 pre-stented vs. 59 matched non-stented). They found that pre-operative stenting only significantly reduced operative times when the stone size was >1 cm (149 vs. 257 min, p = 0.01). They also found a lower re-operative rate for the pre-stented cohort when stone burden ≥1 cm. This finding is in contrast to Shields et al. [17] who only found a positive association, but no statistical significance with pre-operative stenting reducing number of procedures. We did not evaluate the effect of pre-operative stenting on re-operative rates for RIRS as all patients in our study were rendered stone-free. However, given that stone volume is likely the most important predictor of OR time it would also likely predict the need for a staged procedure. Nonetheless, pre-operative stenting allows passive dilation of the ureter, allowing a bigger UAS, and thus better irrigation, vision, and washout of small fragments to make RIRS easier. We would not recommend routine pre-operative stenting, as the morbidity of a stent does not appear to contribute to any gains in OR time for RIRS. As a tertiary referral center, a lot of our patients are already pre-stented (from sepsis, painful obstruction, difficulty with access, etc.), and knowing this information may improve counseling on need for staged procedure but likely no gains in OR time.
There are several limitations of our study. First, the retrospective nature of the study precludes the ability to randomize patients into groups of sheath use or pre-operative stenting. However, our strict inclusion criteria is a strength as only solitary stones not requiring staged procedures were used to eliminate biases. Another limitation is our single-center single-surgeon experience. As a tertiary center, our patient population might have been more complex than the general population. Also patients had pre-operative stents for various amount of time before they got RIRS which may have affected the amount of dilation. Stone composition analysis was also not available for all patients and brushite and struvite stone compositions were rare.
Conclusion
Amongst the main stone factors in RIRS, stone volume has the strongest impact on operative time. This can be used to predict the length of the procedure by roughly adding 2 min per 100 mm3 increase in stone volume. Patients who are curious about the time of procedure may benefit during pre-operative counseling. Also, the surgeon’s schedule in the operating room can be rendered more efficient by scheduling the exact time increase needed for larger stones.
References
Scales CD Jr, Smith AC, Hanley JM et al (2012) Prevalence of kidney stones in the United States. Eur Urol 62:160
Preminger GM, Tiselius HG, Assimos DG et al (2007) 2007 guideline for the management of ureteral calculi. J Urol 178:2418
Jackson TD, Wannares JJ, Lancaster RT et al (2011) Does speed matter? The impact of operative time on outcome in laparoscopic surgery. Surg Endosc 25:2288
Jenkins ED, Yom VH, Melman L et al (2010) Clinical predictors of operative complexity in laparoscopic ventral hernia repair: a prospective study. Surg Endosc 24:1872
Ito H, Kuroda S, Kawahara T et al (2015) Clinical factors prolonging the operative time of flexible ureteroscopy for renal stones: a single-center analysis. Urolithiasis 43:467
Eisner BH, Kambadakone A, Monga M et al (2009) Computerized tomography magnified bone windows are superior to standard soft tissue windows for accurate measurement of stone size: an in vitro and clinical study. J Urol 181:1710
Patel SR, Stanton P, Zelinski N et al (2011) Automated renal stone volume measurement by noncontrast computerized tomography is more reproducible than manual linear size measurement. J Urol 186:2275
Deters LA, Pais VM Jr (2013) Difference in operative time according to stone location for endoscopic management of ureteral and renal stones. Urology 81:522
Grasso M, Ficazzola M (1999) Retrograde ureteropyeloscopy for lower pole caliceal calculi. J Urol 162:1904
Jacquemet B, Martin L, Pastori J et al (2014) Comparison of the efficacy and morbidity of flexible ureterorenoscopy for lower pole stones compared with other renal locations. J Endourol 28:1183
Kourambas J, Delvecchio FC, Munver R et al (2000) Nitinol stone retrieval-assisted ureteroscopic management of lower pole renal calculi. Urology 56:935
L’Esperance JO, Ekeruo WO, Scales CD Jr et al (2005) Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology 66:252
Kourambas J, Byrne RR, Preminger GM (2001) Does a ureteral access sheath facilitate ureteroscopy? J Urol 165:789
Wiener SV, Deters LA, Pais VM Jr (2012) Effect of stone composition on operative time during ureteroscopic holmium:yttrium-aluminum-garnet laser lithotripsy with active fragment retrieval. Urology 80:790
Ito H, Kawahara T, Terao H et al (2012) Predictive value of attenuation coefficients measured as Hounsfield units on noncontrast computed tomography during flexible ureteroscopy with holmium laser lithotripsy: a single-center experience. J Endourol 26:1125
Chu L, Sternberg KM, Averch TD (2011) Preoperative stenting decreases operative time and reoperative rates of ureteroscopy. J Endourol 25:751
Shields JM, Bird VG, Graves R et al (2009) Impact of preoperative ureteral stenting on outcome of ureteroscopic treatment for urinary lithiasis. J Urol 182:2768
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sorokin, I., Cardona-Grau, D.K., Rehfuss, A. et al. Stone volume is best predictor of operative time required in retrograde intrarenal surgery for renal calculi: implications for surgical planning and quality improvement. Urolithiasis 44, 545–550 (2016). https://doi.org/10.1007/s00240-016-0875-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-016-0875-8