Abstract
Nitrosative stress plays a role in calcium oxalate stone formation, as nitrosated proteins have been identified in stone formers. Nitric oxide (NO•), the common precursor for reactive nitrogen species, is synthesized in the juxtaglomerular apparatus of the kidneys. The present study is aimed to determine the role of nitric oxide synthase (NOS) in an experimental hyperoxaluric condition by histological and biochemical techniques. Hyperoxaluria was induced by 0.75% ethylene glycol in drinking water. L-arginine (L-arg) was supplemented at a dose of 1.25 g/kg body weight orally for 28 days. Nitric oxide metabolites (NOx), protein content in the urine and lipid peroxidation in the kidney were determined at the end of the experimental period. Histopathological examination of the rat kidneys was then carried out. NADPH-diaphorase and eNOS expression studies were carried out in control and hyperoxaluric rat kidneys using histochemical and immunohistochemical techniques. Significant amounts of NOx were present in the urine of hyperoxaluric animals when compared to control rats. Histopathological examinations revealed membrane injury, tubular dilatation and edema in the hyperoxaluric rats, whereas co-supplementation of L-arg to the hyperoxaluric rats significantly reduced these changes. The results of histochemical analysis for NADPH-diaphorase staining demonstrate the role of NOS in hyperoxaluric rats. Hyperoxaluric rats showed intense staining for NADPH-diaphorase when compared to control and L-arg co-supplemented hyperoxaluric rats. Immunohistochemical demonstration confirmed that eNOS expression was markedly increased in L-arg supplemented rats, when compared to EG treated rat kidney sections. Thus, from the present study, we conclude that supplementation of L-arg to the hyperoxaluric animals minimizes the cellular injury mediated by ethylene glycol, prevents oxidative/nitrosative damage to the membranes and reduces the incidence of calcium oxalate stone formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oxalate, an end product of metabolism in humans, is a common constituent of most kidney stones and there is increasing evidence to show the involvement of enhanced lipid peroxidation (LPO) in stone formation [1–3]. Furthermore, depletion of antioxidants and decreased activity of antioxidant enzymes have been noted in the kidneys of experimental urolithic rats [2]. Supplementation of vitamin E or methionine normalizes antioxidant status and has been found to prevent stone formation [1]. Earlier studies carried out in our laboratory confirm the involvement of nitric oxide radicals in stone formation [4]. This further prompted us to study the involvement of nitric oxide synthase (NOS) in experimental hyperoxaluria.
The objective of the present study was to investigate the role of NOS in hyperoxaluria. Nitric oxide (NO) is an important mediator in cell-to-cell communication. Renal vascular NO synthesis is accompanied by the activity of NOS III, which has been localized in the juxtaglomerular apparatus (JGA) and tubules [5]. Bechmann and associates (1995) demonstrated that the release of NO can be visualized histochemically by localizing constitutive NOS in mammalian kidney [6]. Enzymatic activity of NOS was assessed histochemically using the NADPH diaphorase technique, a method based on the ability of NOS to generate oxidized nitroblue tetrazolium in the presence of NADPH. This detection was based on the notion that NO reacts at near-diffusion-limited rates with molecular oxygen or at a more rapid rate with superoxide anion (O2−) to form a powerful oxidant and nitrating agent peroxynitrite (ONOO−). With this technique, NO-related effects have been demonstrated in human atherosclerosis [6], acute lung injury [7] and other conditions [8] in humans.
L-arg can suppress inducible NOS and safeguard renal systems from oxalate mediated oxidative damage [9]. Hence, the present study was designed to evaluate the cytoprotective effect of L-arg in experimental hyperoxaluria with reference to NOS using monocloncal eNOS antibody and NADPH-diaphorase (an indirect histochemical technique) and by comparing the histological changes with normal kidney sections.
Materials and methods
Adult male Wistar albino rats weighing 120–160 g were used in this study. A total of 24 rats was divided into four groups of six rats each. Group I served as a normal control, group II served as a drug control receiving L-arg orally (1.25 g/kg body weight) [10]. In group III rats, hyperoxaluria was induced by feeding 0.75% ethylene glycol (EG) [11], whereas in group IV rats, hyperoxaluria was induced as in group III rats with EG but co-supplemented with L-arg as in group II rats. All of the animals were provided with food and water ad libitum for 4 weeks. Animal experiments were conducted in accordance with the guidelines of the institute animal ethics committee.
Samples of 24 h urine from all experimental groups were collected in ice-jacketed beakers maintained at 0°C in an ice bath. A portion of the processed urine was utilized for the determination of nitric oxide metabolites (NOm). At the end of day 28, all study animals were sacrificed by cervical decapitation and the kidneys were removed. These were utilized for the further analysis. The kidneys were trimmed free of connective tissue and finely minced. A 20% homogenate was prepared in Tris-HCl buffer (0.02 M, pH 7.4) using a Potter-Elvehjem homogenizer fitted with a power driven Teflon pestle.
Determination of protein
Protein was determined using Folin’s reagent spectrophotometrically at 640 nm [12].
Determination of NOx
Nitrate and nitrite in urine was determined spectrophotometrically at 540 nm by the method of Suhulz et al. [13].
Determination of LPO products
LPO of tissue fractions was measured by the release of thiobarbituric acid reactive substances (TBARS) by the method of Devasagayam [14].
Histopathology
A portion of the kidney was taken immediately after animal sacrifice and fixed in 10% buffered formalin. The tissues were washed in running tap water, dehydrated in increasing concentrations of alcohol and cleared in xylene. The tissues were then impregnated and embedded in molten paraffin wax. Sections of 4 μm thickness were cut, stained with hematoxylin and eosin and studied under a Nikon microscope (ECLIPSE-400, Type 115) for histopathological changes.
Alizarin red staining
Alizarin red staining for calcium oxalate deposition was carried out by the method of Bancroft and Cook [15].
NADPH-diaphorase staining
This was carried out by the method of Mundel et al. [16] with modifications. Portions of the kidney were removed immediately after animal sacrifice and embedded using Bright Cryo-Embed. Embedding was done at a quick-freezing temperature of −24°C. Cryostat sections of 7 μm thickness were taken using a rotary microtome at a temperature of −17°C. Cryostat sections were thaw mounted on to chrome-alum gelatin coated slides and cold acetone was added to the sections.
The catalytic activity of NOS was demonstrated by enzymatic oxidation of nitro blue tetrazolium (NBT) in the presence of β-NADPH. For this purpose, slides were washed in PBS and incubated for 30–60 min at 37°C in 0.1 M phosphate buffer containing 0.3% Triton X-100, 0.01% NBT, and 0.1% β-NADPH. After replacing NADPH with NADH, no reaction product was found.
Immunohistochemical detection of endothelial nitric oxide synthase
For immunohistochemistry, rat renal tissue was embedded in Tissue-Tek (Sakura Finetek, Europe, Zoeterwoude, The Netherlands), snap-frozen in liquid nitrogen, and stored at −80°C. Consecutive cryostat sections were cut at 4 µm. Cryosections were fixed in acetone for 10 min at room temperature. Briefly, endothelial nitric oxide synthase (eNOS) activity was blocked by incubation with 1% hydrogen peroxide in PBS for 20 min. Non-specific binding sites were saturated by incubation with 5% bovine serum albumin (BSA) in phosphate buffered saline (PBS) for 30 min. Sections were incubated with primary antibodies diluted in PBS with the addition of 0.2% BSA. All of the subsequent steps were performed according to the manufacturer’s instructions (DAKO LSAB2 kit, Carpinteria, Calif., USA). Sections were counterstained with Mayer’s hematoxylin and mounted in GelMount (Biomeda, Foster City, Calif., USA).
Statistical analysis
Statistical analysis was carried out using ANOVA (SPSS Package for Windows, Version 7.5). The results are expressed as mean±SD for six rats.
Results
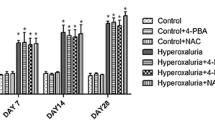
NOx metabolites in L-arginine and experimentally induced hyperoxaluric rats
Figure 1 shows the levels of nitrite/nitrate in the urine of control and experimental animals. The EG treated rats exhibited a significant increase (P<0.001) in the level of nitrate/nitrite when compared with that of the control rats. NOx levels in control rats were 1.53 μmol/24 h urine, which significantly increased to 2.01 μmol/24 h urine in hyperoxaluria induced animals. In L-arg co-supplemented hyperoxaluric rats, the NOx level was 1.74 μmol/24 h urine, whereas in L-arg supplemented rats the level was 1.8 μmol/24 h urine sample.
LPO in experimental animals
Figure 2 shows the level of LPO products in control and experimental animals. LPO was significantly increased at the level of P<0.001 in EG treated rats when compared to control rats. Whereas in rats supplemented with L-arg alone, the LPO levels were maintained near normal. In L-arg co-supplemented hyperoxaluric rats, the levels of LPO products decreased significantly (P<0.001) when compared to the EG induced rats.
Histopathological changes in experimental animals in relation to protein content and kidney weight
Hyperoxaluria was induced under experimental conditions by feeding rats with EG for 28 days. On gross examination, the kidneys were enlarged in hyperoxaluric rats. The cut surface revealed extensive edema and congestion. Examination of the gross and cut surface in control, L-arg supplemented and hyperoxaluric rats co-supplemented with L-arg were unremarkable. The average kidney weight in control rats was 1.33 g. It was significantly increased to 1.49 g in hyperoxaluric rats, whereas in hyperoxaluric rats co-supplemented with L-arg it was 1.41 g (Table 1) and the cut surface was unremarkable. The protein content in hyperoxaluric kidneys was approximately 163 mg/g tissue, whereas in control rats the average value was 152 mg/g tissue. In L-arg co-supplemented EG induced rats, protein content was 154 mg/g of tissue.
Histopathological changes in kidney were analyzed in control and L-arg supplemented rats and compared with hyperoxaluric rats. These changes were corroborated with hyperoxaluric rats co-supplemented with L-arg. On microscopic examination, control (Fig. 3a) and L-arg supplemented (Fig. 3b) rats show normal glomeruli and tubules. In hyperoxaluric rats (Fig. 3c), there was denudation and shedding of the epithelial lining, deposition of tiny crystals and a marked dilatation of proximal and distal tubules. In hyperoxaluric rats co-supplemented with L-arg (Fig. 3d), there was only mild damage to the epithelial lining and minimal dilatation of the tubules.
Histopathological sections of control and experimental rat kidneys. a Control sections from the renal cortex showing glomeruli and tubules (H and E, ×50).b L-arginine supplemented rats showing normal architecture similar to control sections (H and E, ×50). c Hyperoxaluric rats show marked tubular dilatation, extensive shedding and denudation of epithelial lining. Occasional crystal deposits are seen in tubules (H and E, ×50). d Ethylene glycol and L-arginine co-supplemented sections show near normal appearance of glomeruli and tubules (H and E, ×5
Alizarin red staining for calcium oxalate crystal deposition in control and experimental animals
Figure 4a confirms the presence of calcium oxalate crystal deposits in the medullary region of the hyperoxaluria induced rat kidney. Numerous foci of crystal deposition were identified in the region of the distal convoluted tubules in EG treated rats, but such deposition was absent in EG-treated and L-arg co-supplemented rats (Fig. 4b).
Alizarin red staining for the calcium oxalate deposition in EG treated animals. a Sections from EG treated rat renal tubules show calcium oxalate crystal deposition in distal convoluted tubules (×50). b Sections from EG and L-arg co-supplemented rat kidney show resemblance to control kidney sections and no calcium oxalate deposition (×50)
Histochemical localization and expression of NOS (NADPH-diaphorase staining) in control and experimental animals
Our study confirmed the presence of NOS at the JGA and tubules in control kidney sections (Fig. 5a). L-arg supplemented animals maintained low expression of NADPH-diaphorase, similar to the control sections (Fig.5b). In hyperoxaluric rats, the cytochemical expression of NADPH-diaphorase staining showed that the level of NOS was significantly increased (Fig. 5c). In rats in which L-arg was co-supplemented with EG, there was marked reduction in cytochemical expression of NADPH-diaphorase (Fig. 5d).
Histochemical expression of NADPH diaphorase for nitric oxide synthase in cryosections of control and experimental animal kidneys. a Control kidney sections show normal expression of NADPH-diaphorase staining in the region of JGA and tubules (×50). b L-arginine supplemented sections show normal expression of NADPH-diaphorase in the region of JGA and tubules (×50). c Ethylene glycol sections show increased expression of NADPH-diaphorase in JGA apparatus and tubules (×50). d Ethylene glycol and L-arginine co-supplemented sections show reduced expression of NADPH-diaphorase in JGA apparatus and tubules (×50)
Immunohistochemical detection of eNOS in control and experimental kidney sections
Control and L-arg supplemented rat kidney sections showed expression of eNOS in interstitial, endothelial and macula densa cells (Fig. 6a, b), while decreased expression was obtained in kidney sections of hyperoxaluric rats (Fig. 6c). eNOS expression was similar to the control sections in EG-treated and L-arg co-supplemented rat sections (Fig. 6d).
Immunohistochemical detection of endothelial nitric oxide synthase in control and experimental kidney sections. a Sections from control rat kidney show expression of eNOS in endothelial cells of interstitial and peritubular capillaries (×50). b Sections from L-arg supplemented rat kidney show increase in expression of eNOS in endothelial and tubular cells (×50). c Sections from ethylene glycol treated rat kidney show reduced expression of eNOS (×50). d Sections from EG and L-arg co-supplemented rat kidney show expression of eNOS in endothelial cells and tubular region very similar to normal rats (×50)
Discussion
The possible involvement of a free radical mediated LPO reaction in the etiology of stone formation has been investigated by our group [1]. Though several hypotheses have been advocated, cellular injury is considered to be one of the predisposing factors responsible for the retention of crystals. This has been experimentally proved in hyperoxaluric rats [17], in which tubular injury is followed by the excretion of marker enzymes in the urine. Our earlier study has already demonstrated peroxynitrite induced kinetic and functional modification of nitrated Tamm-Horsfall glycoprotein, a urinary protein involved in calcium oxalate stone formation [4].
The protein content and weight of the kidney decreased in hyperoxaluric animals. Earlier studies from our laboratory revealed that the induction of hyperoxaluria results in a reduction of protein content in the kidneys of hyperoxaluric animals [18]. A negative correlation was observed between the protein and LPO products of hyperoxaluric rats. Co-supplementation of L-arg increases the level of protein in the EG induced rats. It has already been reported that supplementation of L-arg increases the protein content in experimental animals [19]. Supplementation of L-arg to the experimental animals increases protein synthesis. This is well supported by the fact that its metabolites are involved in cell replication, collagen synthesis and tissue repair [20].
The final products of NO in vivo are nitrate and nitrite. The relative proportion of these two compounds cannot be predicted with certainty. Thus, the best index of total NO production is the sum of both NO3− and NO2−. Their levels are found to be increased in end stage renal failure and decreased in hypertension, atherosclerosis and angina pectoris [21]. An earlier report suggested that supplementation of L-arg in experimental animals quenches superoxide radical generation and limits the formation of peroxynitrite [22]. In support of this, in L-arg co-supplemented EG treated rats, NOx levels were reduced when compared to EG treated rats. In EG treated rats, significant levels of NOx were excreted in the urine, suggesting the involvement of NO and its radicals in hyperoxaluria [23]. We suggest that in EG treated rats, due to low levels of L-arg in the kidney tubules, there is the possibility of the formation of peroxynitrite, which refluxed urinary excretion of increased NOx compared to the L-arg supplemented animals. Thus, during chronic EG administration, urinary NOx reflect NO production despite ongoing reactive oxygen species (ROS) mediated inactivation of NO [24].
LPO is thought to be an important consequence of oxidative cellular damage [25]. The destruction of unsaturated fatty acids via LPO has been linked with an altered membrane structure [26] and enzyme inactivation [27]. It has already been reported that LPO was induced in hyperoxaluric rats [28]. Supplementation of L-arg releases NO that can attenuate membrane dysfunction and tissue injury, owing to its ability to bind transition centers participating in Fenton-type processes and to efficiently scavenge free radical species that propagate peroxidation chain reactions [29]. On the other hand, when generated at higher concentrations in the presence of oxygen, superoxide and other ROS, NO can be converted into a range of potent oxidants, such as nitrogen dioxide and peroxynitrite which may amplify and exacerbate the noxious effects of LPO [30]. Supplementation of L-arg reduces the level of lipoperoxides produced in hyperoxaluric rats and it has been documented to protect the membrane, thereby proving that L-arg has cytoprotective activity. It has already been reported by Lubec et al., that L-arg supplementation reduces the levels of LPO in diabetic patients [31].
Administering EG to experimental animals leads to the formation of glycolaldehyde, glycolic acid, calcium oxalate and hippuric acid, all of which have cytotoxic effects on the renal tubular cells [32]. Earlier studies from our laboratory revealed that induction of EG to experimental animals causes tubular degeneration and cells casts [33]. CaOx crystal deposits are evident in Alizarin red stained sections of EG treated rats and are present in the region of distal convoluted tubules. Earlier reports also confirm the presence of calcium oxalate crystals in EG treated animals in the region of distal convoluted tubules and collecting duct of experimental urolithic animals [34]. Supplementation of L-arg to the experimental animals provides cytoprotection to the renal epithelial cells and reduces the cytotoxic properties of EG induction. Moreover, L-arg metabolic products have wound healing capacity [35]. Results of our histopathological and histochemical analyses indicates that supplementation of L-arg to EG-treated animals minimizes the crystal deposition and tubular damage. Similarly supplementation of L-arg alone to the experimental animals does not cause any change in the architecture of kidney sections. The hyperoxaluria that is induced ultimately results in the production of free radicals and oxidative injury to the epithelial lining. It has already been reported that peroxidised protein acts as a heterogeneous nucleator for the nucleation and aggregation of calcium oxalate stone formation [36]. The renal tissue, which is damaged due to peroxide stress, is more prone to calcium oxalate crystal retention. This paves the way for heterogeneous nucleation with minerals at the injured epithelial surface. These oxidation-induced changes are reversed under experimental conditions by feeding rats with L-arg, demonstrating the antioxidative and antilithic property of L-arg.
NO is produced by the conversion of oxygen and L-arg to NO and L-citrulline. This reaction is catalyzed by NOS, of which there are three different isoforms: eNOS, inducible nitric oxide synthase (iNOS) and neuronal nitric oxide synthase (nNOS) in almost all types of cells [37]. eNOS and nNOS are constitutive and Ca2+-calmodulin dependent isoforms that are involved in cellular signaling. iNOS is an inducible isoform produced only in response to a stimulus and is not Ca2+ dependent. NADPH diaphorase activity can be used as a marker for NOS [38]. NOS can produce NO in NADPH-dependent fashion in response to changes in intracellular calcium by deimidating arginine to citrulline [39]. The NOS-positive cells stained for NADPH diaphorase, show localization at the JGA and tubules of the kidney. In the absence of NADPH, no staining was observed. Our findings suggest that macula densa cells of the JGA could produce increased amounts of NO in hyperoxaluric rats.
The present study demonstrates the strongly enhanced signal for NADPH-diaphorase staining in hyperoxaluric animals at the macula densa cells of the JGA, suggesting the role of NOS in the free radical mediated urolithic condition. Moreover, the decreased expression of eNOS in the hyperoxaluric condition and its normal expression in L-arg co-supplemented hyperoxaluric animals confirm the involvement of iNOS in the pathogenesis of stone formation. It has already been reported that oxidative stress results in the production of a large amount of NO originating from the induction of inducible type II NOS, and it reacts with locally generated superoxide to form ONOO− [40], which in turn can damage proteins and cause membrane injury.
To conclude, L-arg, an inducer of eNOS, is found to suppress the release of NO by iNOS and formation of ONOO−. By maintaining the antioxidant and thiol status of the proteins, L-arg prevents antioxidant enzyme inactivation and membrane damage. It also effectively curtails LPO and reduces the membrane injury mediated by EG. Thus, L-arg acts as an effective antioxidant and cytoprotectant in experimental hyperoxaluric rats.
References
Selvam R (2002) Calcium oxalate stone disease. Role of lipid peroxidation and antioxidants. Urol Res 30: 35
Adhirai M, Selvam R (1993) Effect of cyclosporin A on tissue lipid peroxidation and membrane bound ATPases in hyperoxaluric rats and the protection by vitamin E treatment. Jpn J Med Sci Biol 50: 9
Scheid C, Honeyman T, Kohjimoto Y, Cao LC, Jonassen J (2000) Oxalate induced changes in renal epithelial cell function: role in stone disease. Mol Urol 4: 371
Pragasam V. Kalaiselvi P, Sumitra K, Subhashini B, Varalakshmi P (2005) Structural and functional modification of THP on nitration: comparison with stone formers THP. Nephron Physiol 99: 28
Hope BT, Vincent SR (1989) Histochemical characterization of neuronal NADPH-diaphorase. J Histochem Cytochem 37: 653
Bachmann S, Bosse HM, Mundel P (1995) Topography of nitric oxide synthesis by localizing constitutive NO synthases in mammalian kidney. Am J Physiol 268: F885
Haddad IY, Pataki G, IIu P, Galliani C, Beckman JS, Matalon S (1994) Quantification of nitrotyorosine levels in lung sections of patients and animals with acute lung injury. J Clin Invest 94: 2407
Crow JP, Beckamn JS (1995) Reactions between nitric oxide, superoxide, and peroxynitrite footprints of peroxynitrite in vivo. Adv Pharmacol 34: 17
Pragasam V, Kalaiselvi P, Sumitra K, Srinivasan S, Varalakshmi P (2005) Counter action of nitrosative stress in hyperoxaluric animals by supplementation ofL-arginine: a potent antilithic agent. Clin Chem Acta 354: 159
Can C, Sen S, Boztok W, Tugular I (2000) Protective effect of oralL-arginine administration on gentamicin induced renal failure in rats. Eur J Pharmacol 390: 327
Khan SR (1997) Animal models of kidney stone formation-an analysis. World J Urol 15: 236
Lowry OH, Rosenbrough NJ, Farr AL, Randall RJ (1951) Protein determination using Folin-Ciocalteau reagent. J Biol Chem 19: 265
Suhulz K, Kerber S, Kelm M (1999) Re-evaluation of the Griess method for determining NO/NO2− in aqueous and protein containing samples. Nitric Oxide 3: 225
Devasagaym TPA (1986) Lipid peroxidation in rat uterus. Biochim Biophys Acta 876: 507
Bancroft JD, Cook HC (1995) Manual of histological techniques and their diagnostic application. Livingstone, Edinburgh
Mundel P, Bachmann S, Bader M, Fischer A, Kummer W, Mayer B, Kriz W (1992) Expression of nitric oxide synthase in kidney macula densa cells. Kidney Int 42: 1017
Khan SR, Finlayson B, Hackett RL (1982) Experimental calcium oxalate nephrolithiasis in the rat, role of renal papilla. Am J Pathol 107: 59
Selvam R, Bijikurien T (1991). Methionine feeding prevents kidney stone deposition by restoration of free radical mediated changes in experimental rat urolithiasis. J Nutr Biochem 2: 644
Guoy WU, Morris SMJr (1998) Arginine metabolism: nitric oxide and beyond. Biochem J 336: 1
Natita I, Border WA, Ketteler M, Ruoslahti E, Noble NA (1995)L-arginine may mediate the therapeutic effects of low protein diets. Proc Natl Acad Sci U S A 92: 4552
Hambrcht R, Hilbrich L, Erbs S (2000). Correction of endothelial dysfunction in chronic heart failure: additional effects of exercise training and oralL-arginine supplementation. J Am Coll Cardiol 35: 701
Suessenbacher A, Lass A, Mayer B, Brunner F (2002) Antioxidative and myocardial protective effects ofL-arginine in oxygen radical-induced injury of isolated perfused rat hearts. Naunyn-Schmiedeberg’s Arch Pharmacol 365: 269
Toblli GE, Stella I, De Cavangh E, Angerosa M, Inserra F, Ferder L (1999) Enalapril prevents tubulointestinal lesions by hyperoxaluria. Hypertension 33: 225
Poderoso JJ, Carreras MC, Lisdero C, Riobo N, Schopfer F, Boveris A (1996) Nitric oxide inhibits electron transfer and increases superoxide radical production in rat heart mitochondria and submitochondrial particles. Arch Biochem Biophys 328: 85
Plaa GL, Witschi H (1976) Chemicals, drugs and lipid peroxidation. Annu Rev Pharmacol Toxicol 16: 125
Selvam R, Ravichandran V (1991) Effect of oral methionine and vitamin E on blood lipid peroxidation in vitamin B6 deficient rats. Biochem Int 23: 1007
Muthukumar A, Selvam R (1997) Renal injury mediated calcium oxalate nephrolithiasis: role of lipid peroxidation. Renal Failure 19: 401
Bijikurian T, Selvam R (1989). Induction of lipid peroxidation in calcium oxalate stone formation. Indian J Exp Biol 27: 450
Mori M, Gotoh T (2000) Regulation of nitric oxide production by arginine metabolic enzymes. Biochem Biophys Res Commun 275: 715
Kroncke KD, Fehsel K, Kolb-Bachofen V (1997) Nitric oxide: cytotoxicity versus cytoprotection—how, why, when and where? Nitric Oxide Biol Chem 1: 107
Lubec B, Hayn M, Kitzmuller E, Vierhrapper H, Lubec G (1997)L-arginine reduces lipid peroxidation in patients with diabetes mellitus. Free Radic Biol Med 22: 355
Hallson PC (1988) Oxalate crystalluria. In: Rose GA (ed) Oxalate metabolism in relation to urinary stone. Springer Verlag, Heidelberg New York, p 131
Selvam R, Vijiya A (2000) Effects of renal ischaemia reperfusion on calcium oxalate retention. Indian J Med Res 111: 62
Wesson JA, Johnson RJ, Mazzali M, Beshensky AM, Stietz S, Giahelli C, Liaw L, Alpers CE, Courser WG, Kleimann JG, Hughes J (2003) Osteopontin is a critical inhibitor of calcium oxalate crystal formation and retention in renal tubules. J Am Soc Nephrol 14: 139
Guoyao WU, Morris SMJr (1998) Arginine metabolism: nitric oxide and beyond. Biochem J 336: 1
Govindaraj A, Selvam R (2001) Increased calcium oxalate crystal nucleation and aggregation by peroxidised protein of human kidney stone matrix and renal cells. Urol Res 29: 194
Griffith OW, Stuehr DJ (1995). Nitric oxide synthases: properties and catalytic mechanism. Annu Rev Physiol 57: 707
Wang Y, Marsden PA (1995). Nitric oxide synthases: biochemical and molecular regulation. Curr Opin Nephrol Hypertens 4: 12
Knowles RG, Palacios M, Palmer RM, Moncada S (1989) Formation of nitric oxide fromL-arginine in the central nervous system: a transduction mechanism for stimulation of the soluble guanylate cyclase. Proc Natl Acad Sci U S A 86: 5159
Beckman JS, Koppenol WH (1996) Nitric oxide, superoxide and peroxynitrite: the good, the bad, and the ugly. Am J Physiol 271: C1424
Acknowledgements
The first author gratefully acknowledges the Indian Council of Medical Research for the financial assistance in the form of SRF. This work was partially supported by the ICMR grant no. 52/3/98-BMS II. The authors are thankful to Mr. A. Dalton Vinod for technical assistance in histological studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pragasam, V., Sakthivel, R., Kalaiselvi, P. et al. Detection of endothelial nitric oxide synthase and NADPH-diaphorase in experimentally induced hyperoxaluric animals. Urol Res 33, 301–308 (2005). https://doi.org/10.1007/s00240-005-0477-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-005-0477-3