Abstract
Introduction
Cortical vein thrombosis (CVT) is a rare disorder, and its diagnosis is challenging. The aim of our study was to evaluate the value of different imaging modalities for the detection of CVT.
Methods
Thirteen patients with CVT, either isolated (n = 3) or in combination with sinus thrombosis (n = 10), and 20 control patients without any venous pathologies were included in this study. The analysis was performed independently by three blinded readers who evaluated the following imaging modalities and sequences separately: non-enhanced computed tomography (NCCT); multi-detector row CT angiography (MDCTA); diffusion-weighted (DWI), T1-weighted (T1w), PD-weighted (PDw), T2*-weighted (T2*w), and fluid-attenuated inversion recovery-weighted (FLAIRw) magnetic resonance (MR) sequences; as well as venous MR angiography (vMRA). The sensitivity, specificity, positive (PPV) and negative predictive values, and interobserver agreement of the different modalities were calculated.
Results
T2*w showed the highest sensitivity for the detection of CVT (97.4%), followed by T1w (70%). FLAIRw and vMRA had a sensitivity of 50% and 41.7%, respectively, whereas the sensitivity of NCCT, MDCTA, DWI, and PDw was below 30%. The specificity and PPV of all modalities was 100%, with good to perfect interobserver agreement.
Conclusion
T2*w was the superior MR imaging sequence for diagnosing CVT. Besides T2*w, only T1w reached a sensitivity of over 50% for CVT, followed by FLAIRw, and vMRA. On the contrary, our results suggest that NCCT but also MDCTA might not be suitable for diagnosing CVT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The cortical veins are highly variable in number, size, and localization, which make their radiological evaluation very challenging [1, 2]. A cortical vein thrombosis (CVT) can lead to venous hypertension, edema, infarction, or hemorrhages [2, 3]. Symptoms of CVT include focal or generalized seizures followed by hemiparesis, aphasia, hemianopia, or other focal deficits, often without signs of elevated intracranial pressure [2–4].
CVT can occur either in an isolated form (isolated CVT (ICVT)) or in combination with a thrombotic occlusion of the venous sinuses (combined CVT (CCVT)). ICVT is a very rare diagnosis and has only been reported in case reports or in small series [4–15]. However, it is difficult to diagnose in vivo because of the lack of a gold standard, and thus, it might be overlooked occasionally [7, 14].
Recently, T2*w has been shown to be of great diagnostic value for the detection of cortical vein involvement in cerebral venous thrombosis [6, 7, 15]. Non-enhanced computed tomography (NCCT) and multi-detector row CT angiography (MDCTA) have been shown to be of great value for the diagnosis of deep cerebral venous thrombosis [16] and sinus thrombosis (SVT), respectively [17, 18]. Yet, there are neither any data on the specificity of the different magnetic resonance (MR) sequences for CVT nor any studies available that address the diagnostic value of NCCT and MDCTA for CVT. Thus, we initialized this blinded, multi-reader study on patients with CVT and on control patients to assess the sensitivity, specificity, positive (PPV) and negative (NPV) predictive value, and interobserver agreement of different imaging modalities including NCCT, MDCTA, and different MR imaging (MRI) sequences for the detection of CVT.
Materials and methods
The study was approved by our Institutional Review Board and was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients who participated in the clinical investigations.
Definitions
We defined ICVT as an isolated thrombosis of one or more cortical veins without involvement of sinus or deep cerebral veins, whereas CCVT was defined as a thrombosis of cortical veins in combination with an SVT. The term SVT was used to denote an SVT without an involvement of cortical veins.
To facilitate reading, the item imaging modalities was used not only to indicate NCCT, MDCTA, and MRI but also refers to the different MR sequences we used. The phrase extent of thrombosis specifies the individual veins and sinuses that were affected by a respective occlusion.
Patients
We used our electronic, in-hospital database of clinical records to search for the key words cortical, venous, sinus, cerebral, isolated, and thrombosis to identify all patients with ICVT or CCVT seen in our institution between 2002 and 2007. Only patients in whom direct signs of a CVT were present on at least one imaging modality were included in the study. Three patients with ICVT and ten patients with CCVT matched the inclusion criteria and constituted the study group (mean age, 44.3 years; range, 7–79 years, ten females). Digital subtraction angiography (DSA) was also available for five of the patients. Table 1 shows demographic data, clinical presentation, and details on available imaging. The mean time interval between the symptom onset and initial imaging was 4.4 days (range, 0–15 days).
In addition, we included a control group of 20 consecutive patients who had initially presented with symptoms of venous thrombosis including severe headache (n = 20) and drowsiness (n = 5), but for whom imaging showed no pathological intracranial findings and for whom clinical and imaging follow-up was uneventful (mean age, 33.2 years; range, 16–73 years; 12 females). In ten of these patients, MRI with T2*-weighted (T2*w), PD-weighted (PDw), diffusion-weighted (DWI), T1-weighted (T1w), and fluid-attenuated inversion recovery-weighted (FLAIRw) sequences, as well as venous time-of-flight MR angiography (vMRA) were available; in the other ten patients, NCCT and MDCTA had been conducted.
Imaging parameters
All examinations were conducted under the following clinical routine conditions. Both NCCT and MDCTA were performed on a 4 (n = 7 cases) or 64-detector row CT (n = 16 cases). For NCCT, the following parameters were used: 120 kV, 300 mAs, a collimation of 2.5 mm, a section width of 5 mm, and a reconstruction increment of 5 mm. For MDCTA, the following parameters were used: 120 kV, 120 to 140 mAs, and a collimation of 4 × 1.0 or 64 × 0.62 mm. Venous catheters (18 gauge) were placed in the antecubital vein to apply 120 mL of contrast agent with an iodine concentration of 300 mg/mL after a delay of 35 s at flow rates between 3 and 5 mL/s.
MRI was performed on 1.5 T scanners using the following sequences: DWI (b-values, 0 slice thickness = 5 mm; field of view (FOV) = 210 mm; matrix size = 128; 23 slices) PDw acquired as a dual-echo spin-echo acquisition with T2w (TR = 2,210 ms; TE = 85/14 ms; slice thickness = 6 mm; FOV = 210 mm; matrix size = 256; 23 slices), T1w (TR = 665 ms; TE = 14 ms; slice thickness = 6 mm; FOV = 210 mm; matrix size = 256; 23 slices), T2*w (TR = 1,000 ms; TE = 22 ms; slice thickness = 5 mm; FOV = 210 mm; matrix size = 256; 23 slices), FLAIRw (TR = 7,500 ms; TE = 74 ms; inversion time (TI) = 2,500 ms; slice thickness = 5 mm; FOV = 220 mm; matrix size = 256; 19 slices), and vMRA with arterial saturation pulses (TR = 24 ms; TE = 5.6 ms; flip angle = 50°; slice thickness = 3 mm; FOV = 210 mm; matrix size = 256; 50 slices).
DSA was performed on a biplanar DSA unit including selective catheterizations of both internal carotid arteries and the dominant vertebral artery, late venous phases, and oblique projections.
Image interpretation
A standardized evaluation of the datasets was performed independently on a standard PACS workstation by three experienced neuroradiologists, who were blinded to all clinical data and patient identification information. The different imaging modalities were analyzed separately in randomized reading orders using a standardized evaluation form.
For each modality, the readers evaluated direct and indirect signs of a thrombosis. The absence or presence of the following direct signs of a thrombosis were noted: hyperattenuated cerebral veins (i.e., hyperattenuated vein sign [16]) or sinuses (i.e., cord sign [16]) on NCCT; venous filling defects or missing vein on MDCTA; hyperintense veins or sinuses on DWI, T1w, PDw, and FLAIRw; hypointense veins or sinuses on T2*w (delineated as pronounced, extracerebral “tubular, serpentine, or rounded” [7] hyposignal which is larger in diameter than the vascular structures on other sequences, an appearance which has been described as blooming); and lack of venous flow void on vMRA. Note that both source images and maximum intensity projection reconstructions of the vMRA and the MDCTA were analyzed and that only the DWI images with a b-value of 1,000 were evaluated.
Based on these findings, the readers decided whether they interpreted a respective modality as indicative of a CVT or an SVT and noted the extent of the respective thrombosis.
Means of confirming diagnoses—consensus reading
After having evaluated all datasets, the readers performed a consensus reading to obtain a reference standard. They collaboratively reviewed all available imaging modalities including follow-up imaging and studied the clinical records to take into account all clinical and outcome information. They subsequently determined in consensus (1) the overall presence of an ICVT or a CCVT, (2) the extent of the respective thrombosis, (3) the presence of an edema, or (4) the presence of a hemorrhagic venous infarction.
If there were discrepant findings between the different modalities, the reference standard for the cortical veins was based on the results of the T2*w, and the reference standard for the sinuses was based on the source images of the vMRA or MDCTA. Whenever DSA was available, it was additionally evaluated. PDw and FLAIRw were given precedence for intracerebral edema, and T2*w was given precedence for hemorrhage.
Statistical analysis
All patient and image interpretation data were entered into a database and analyzed with standard software. The sensitivity, specificity, PPV, and NPV of the different modalities were calculated.
To account for time-dependent signal changes of thrombus material on T1w and PDw, we grouped the patients into either acute thrombosis (imaging performed within 0 to 5 days after symptom onset, n = 5) or subacute thrombosis (imaging performed within 6 to 15 days after symptom onset, n = 8) and then performed subgroup analyses of the sensitivity, specificity, PPV, and NPV. This was not done for FLAIRw due to the limited number of cases for which it was available.
To determine the interobserver agreement regarding the presence of a CVT or SVT, multirater κ values were calculated as described in the literature [19]. Multirater κ values can range from −1.0 to 1.0, with −1.0 indicating perfect disagreement below chance, 0.0 indicating agreement equal to chance, and 1.0 indicating perfect agreement above chance [19].
Results
Consensus reading
Table 2 summarizes the results of the consensus reading. The frontal cortical veins were involved in all but one of the CVT patients, and the superior sagittal sinus (SSS) was affected in all patients with CCVT. On average, 5.9 cortical veins were affected (range, 2–8), as demonstrated by T2*w (Figs. 1, 2, 3, and 4). In all other modalities, a fewer number of cortical veins showed direct signs of CVT.
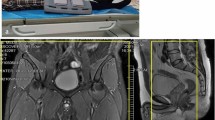
Patient with combined cortical vein thrombosis (patient 4). Thrombosis of superior sagittal sinus (arrowheads) and both frontal and parietal cortical veins (e.g., arrows) is depicted as hypointense signal on T2*-weighted (T2*w) (a), hyperintense signal on T1-weighted (b) and PD-weighted (c), and lack of flow signal on venous magnetic resonance angiography (vMRA; d, source image). Please note that the largest number of affected cortical veins is revealed by T2*w, while the evidence of “missing veins” on vMRA is questionable
Patient with isolated cortical vein thrombosis and large left parietal intracerebral hemorrhage (b) (patient 7). Isolated thrombosis of left frontal and parietal cortical veins (e.g., arrows) is depicted as hypointense signal on T2*-weighted (a, b) and the impression of “missing veins” on the left side compared to right on venous magnetic resonance angiography (d, source image). Please note that there is no hyperintense signal present in the affected veins on PD-weighted (c) and that there is a regular flow signal within superior sagittal sinus on all sequences (a–d, arrowheads)
Patient with isolated cortical vein thrombosis (patient 13). Isolated thrombosis of frontal and parietal cortical veins, bilaterally, is depicted as hypointense signal on T2*-weighted within the affected veins (a). There is an impression of “missing veins” on the left side compared to right on both multi-detector row CT angiography (b source image) and venous magnetic resonance angiography (c, source image), yet this is not easily recognized without knowledge of the T2*-weighted images; digital subtraction angiography shows a delayed venous drainage (d, e)
Patient with combined cortical vein thrombosis (patient 1). Thrombosis of the superior sagittal sinus (arrowheads) and frontal and cortical veins (e.g., arrows) is depicted as hypointense signal on T2*-weighted (a), hyperintense signal on fluid-attenuated inversion recovery and as diffusion restriction on diffusion-weighted, B1000 (c) and apparent diffusion coefficient map (d)
Blinded readings—overall diagnosis of CVT and SVT
Each of the readers performed 160 readings; thus, there were 480 readings in total. A CVT was correctly diagnosed in 105 readings (21.9%) with no false positives, but there were 135 false negatives (28.1%). An involvement of the sinus was correctly found in 129 readings (26.9%), misdiagnosed in three false positive readings (0.6%), and missed in 57 false negatives (11.9%).
T2*w showed the highest sensitivity for CVT with 97.4% (Figs. 1, 2, 3, and 4), followed by T1w (70%, Fig. 1), FLAIRw (50%, Fig. 4), and vMRA (42.7%; Figs. 1, 2, and 3). The sensitivity of NCCT (Fig. 5), MDCTA (Figs. 3 and 5), DWI (Fig. 4), and PDw (Figs. 1 and 2) was below 30%. The subgroup analysis revealed a sensitivity of 25% and 26.7% for PDw and a sensitivity of 60% and 80% for T1w for acute and subacute CVTs, respectively. All modalities showed a specificity of 100%. The κ values ranged from 0.73 (T1w) to 1.0 (FLAIRw) for CVT and from 0.63 (NCCT) to 1.0 (MDCTA and FLAIRw) for SVT. Table 3 details the sensitivity, specificity, PPV, NPV, and interobserver agreement of the different modalities for the diagnosis of CVT or SVT.
Patient with combined cortical vein thrombosis (patient 3). Upper row (a–c): non-enhanced computed tomography, lower row (d–f): multi-detector row CT angiography (MDCTA). Arrows in a–c indicate hyperdense vein sign in a right parietal cortical vein. Please note that this vein shows no filling defect in MDCTA (arrows in e and f). There is a thrombosis of the superior sagittal sinus (arrowheads in a–c) with a cord sign on non-enhanced computed tomography (a–c) and a filling defect on MDCTA (d–f)
Blinded readings—extent of thrombosis
Concerning the individual venous structures, T2*w showed the highest sensitivity for a thrombotic occlusion of the frontal, parietal, and occipital cortical veins (86.1%, 94.6%, and 50%, respectively), while vMRA was most sensitive for an involvement of the temporal cortical veins (33.3%). With regard to the sinuses, MDCTA was superior for all sinuses except the right transverse sinus, for which FLAIRw and PDw had the highest sensitivity. For details on the sensitivity, specificity, PPV, and NPV of the different modalities regarding the extent of the thrombosis, see Table 4.
Discussion
To our knowledge, this is the first study on CVT to use a blinded, multi-reader set-up and a control group. This is also the first time that a study has reported on the specificity, not just on the sensitivity, of the different modalities for this disease. We found a high sensitivity and specificity for T2*w, followed by T1w, FLAIRw, and vMRA, while the value of both NCCT and MDCTA for diagnosing CVT was poor.
Most of our patients presented with CCVT; we identified only three patients with ICVT. This finding reflects the fact that ICVT is a very rare diagnosis, which has only been reported as single case reports or small series [4–15]. In our patients, the frontal veins were involved in all but one case, followed by the parietal veins as second most frequent localization of CVT. This predilection of the frontal cortical veins is in accordance with available studies on CVT [4–15]. A thrombosis of the temporal or occipital veins was found rarely, and none of our patients presented with an involvement of the anastomotic vein of Labbé. As in the literature, the SSS was the sinus that was most often affected in our CCVT patients, which is easily understood by recognizing that CCVT usually develops secondary to SVT via retrograde thrombus propagation from the occluded sinus [4].
NCCT
In most institutions, NCCT is often performed as the first line of investigation in the emergency setting. While the direct signs on NCCT have a high sensitivity and specificity for a thrombosis of the deep cerebral veins, their sensitivity for the diagnosis of an SVT has been shown to be below 75% [16, 20, 21]. These findings are consistent with our observations regarding the affection of the sinuses. With regard to the involvement of cortical veins, we also found a very low sensitivity of the dense vein sign. This is most probably due to their localization in immediate vicinity to the skull, resulting in partial volume effects [16]. Thus, we must conclude that NCCT is not suitable for the exclusion of CVT, although it has a high PPV for this diagnosis.
Angiographic techniques
DSA
DSA was the gold standard for the diagnosis of cerebral venous occlusive diseases, but it has been replaced by MRI and MDCTA [15, 16, 22, 23]. Although some authors still discuss whether DSA has a higher sensitivity for the diagnosis of CVT than the other imaging techniques [7], no systematic studies on this topic exist.
The DSA diagnosis of CVT relies on indirect signs such as delayed local venous drainage, lack of opacification of the corresponding brain region, “missing” cortical veins, a partially visualized vein that abruptly stops or is surrounded by dilated cortical veins, and cortical collaterals appearing as “corkscrew-vessels” [7, 24]. On angiography, all that may be seen is vascular congestion in the region of drainage of the occluded vein because the thrombosed vein itself often does not opacify. Thus, DSA only allows an indirect visualization of a thrombosis. Another important limitation of DSA in the interpretation of these signs is the high variability of the number and location of the cortical veins both intra- and inter-individually. The pattern of cortical venous drainage is variable and often asymmetric, which impairs the identification of a “missing vein” [1, 2, 7]. The lack of contrast filling of a vessel in a certain cortical region does not necessarily indicate a CVT but can simply indicate the absence of a vein in this specific region as anatomic variation. These drawbacks of DSA, which are true for all angiographic techniques, including MDCTA and vMRA, do not support DSA being superior to MRI for diagnosing CVT.
MDCTA
MDCTA allows the visualization of the cerebral venous structures with a high spatial and temporal resolution [25] and has an excellent sensitivity and specificity for the detection of SVT [17]. Thrombotic material in MDCTA is visualized indirectly, like DSA, by demonstration of contrast filling defects. Therefore, this technique is less prone to flow artifacts than vMRA [17].
While we confirmed the diagnostic value of MDCTA for the sinuses, we revealed a low sensitivity for the detection of CVT. Our findings indicate that when MDCTA is the only imaging modality, it is difficult for the reader to distinguish between a “missing vein” that indicates a CVT and one that indicates an anatomic variation. Furthermore, we observed cases in which MDCTA did not show a filling defect in cortical veins that clearly demonstrated direct signs of thrombotic occlusions on the other imaging modalities (Fig. 5). This might be due to the small diameter of the cortical veins and to partial volume effects from the enhancing walls of the vessels as suggested by the empty delta sign on a prior contrast-enhanced CT [20]. Our results suggest that MDCTA—although of great value for SVT—might not be suitable for the diagnosis of CVT, a finding that should be validated in further studies.
Venous MRA
While the sensitivity of vMRA for SVT was 81.5%, it was below 50% for CVT in our patients, which is comparable to the previous report by Idbaih et al. (37%, [15]). We used two-dimensional time-of-flight vMRA, because it is widely used both in clinical routine and in studies on CVT [6, 7, 15]. In this sequence, a thrombosis presents as a lack of flow signal in the respective venous structure. With regard to CVT, vMRA in general suffers from the same limitations as DSA and MDCTA, namely, the considerable anatomical variations of the CVs. There are two additional reasons for this limited value of time-of-flight vMRA: a subacute, hyperintense thrombus could potentially simulate normal venous flow signal [26], and a lack of flow signal in a respective vessel might result from in-plane flow [27]. Promising, new vMRA techniques exist such as high-resolution contrast-enhanced gradient-echo MRA, time-resolved MRA [28], and their potential value for CVT, especially at higher field strengths, should be addressed in future studies.
T1w, PDw, FLAIRw, and DWI
Although MRI is regarded as the current gold standard for cerebral venous occlusions [15, 22, 23], it has several diagnostic pitfalls due to the complex, time-dependent signal characteristics of the thrombotic material in the different MR sequences [7, 29, 30], which are similar for ICVT and for SVT [4, 7].
In the case of an acute thrombosis, the intravasal clot shows a hypointense signal on T2w or FLAIRw and an iso- or slightly hyperintense signal on T1w in most case [7, 15, 30, 31]. Thus, the clot may be poorly distinguished from the normal blood flow signal, resulting in a low sensitivity of these sequences during the first days of a thrombosis, especially if small veins are affected. Within the second week after symptom onset, the thrombus material is reported to be typically hyperintense in both T1w and T2w or FLAIRw, which makes these sequences potentially more valuable for the diagnosis of a subacute thrombosis [7, 15, 30].
In accordance with the literature [15], T1w was the second most sensitive sequence for CVT (70%) independent of thrombus age and was also found to have a high specificity for CVT. We found a higher sensitivity of T1w for subacute CVT (80%) than for acute CVT (60%). Regarding sinus involvement, T1w was considerably more sensitive in the acute phase (91.7%) than in the subacute phase (41.7%) in the blinded readings. The last finding is somewhat surprising: the consensus reading revealed direct signs of SVT in all subacute cases. The most probable explanation for this discrepancy is a misinterpretation of the hyperintense signal in the sinuses on T1w as flow signal in some of the blinded readings. This underlines the challenge radiologists are faced with in interpreting MR sequences for venous system thrombosis.
The sensitivity of FLAIRw in our patients (50%) was considerably higher than has been reported [15], yet FLAIRw was only available in six of our patients, which limits the interpretation of these results. Interestingly, we found no data on clot appearance on PDw in the literature. The consensus reading showed that time-dependent signal intensities of thrombus material in CVs on PDw are similar to those reported for T2w and FLAIRw: mostly hypointense in the acute phase, mostly hyperintense in the subacute phase, but with considerable variation. This resulted in a higher sensitivity of PDw for an involvement of the sinuses in the subacute phase (91.7%) compared to the acute phase (88.9%), but resulted in almost no time-dependent difference with regard to CVT (25% for acute CVT and 26.7% for subacute CVT).
On DWI, diffusion restriction within an intravasal clot resulting in a hyperintense signal on images with a b-value of 1,000 and in a lowered apparent diffusion coefficient value has been reported for both SVT and CVT [15, 32, 33]. Data on its sensitivity vary from 3% to 39% for CVT ([15, 33]; 13.9% in our patients) and from 3.7% (our study) to 41% for SVT [32]. In accordance with the literature, hyperintense clot signal on DWI was only present in cases in which the thrombus was also hyperintense on FLAIRw and T1w [32, 33], indicating that it provides little additional information for the diagnosis of CVT or SVT. Yet, DWI has been proposed to be of prognostic value for potential recanalization of occluded veins [32]. Further studies are necessary to clarify the value of clot imaging in DWI for CVT.
In order to access not only the sensitivity but also the specificity of the different modalities, we chose a study design that included a control group. We would like to point out that the presence of direct signs on any of the MR sequences had a high specificity for CVT (100%) even if their sensitivity was very low, e.g., as low as that of PDw or DWI.
T2*w
T2*w was superior to all other modalities for both the presence of a CVT and the involvement of individual cortical veins, with a sensitivity of 97.4% for CVT even in the blinded reader set-up and a specificity of 100% for both CVT and SVT. It was the only sequence that was positive in all CVT cases, and its sensitivity for SVT was also considerably high (96.6%). Our findings are in accordance with recent imaging studies on CVT that showed that T2*w improved the diagnosis of CVT, especially at the acute stage of the disorder when the intraluminal thrombus is not yet hyperintense on T1w [6, 7, 11, 15, 34, 35]. Selim et al. reported that T2*w echo-planar sequences can enhance the detection of intravasal clots [34]. Others showed that conventional T2*w gradient-echo sequences have an even higher sensitivity for CVT because they exhibit considerably higher sensitivity to susceptibility differences [6]. An advantage of T2*w compared to other MR sequences is that the thrombus material shows a hypointense signal for a relatively long time interval from symptom onset. In some cases, T2*w has even been shown to be positive up to 1 year after symptom onset and in the case of complete clinical recovery, which has to be taken into account if T2*w is interpreted solely [7, 15].
In one of the control patients, both frontal and temporal cortical veins were judged as hypointense on T2*w by one of the readers. Although this did not result in a false positive diagnosis of CVT, we would like to comment on the potential pitfalls on T2*w. In our opinion, the most important sources for false positive results are acute or chronic subarachnoid hemorrhages [36] or superficial siderosis, which present with a hypointense lineal signal within the subarachnoid space or the superficial layers of the cortex, respectively [37]. To distinguish these findings from a hypointense clot, we strongly recommend that only an extracerebral, “well-delineated tubular,” and “rounded” hyposignal ([7], “blooming”) should be judged as indicative for CVT.
Our study further enhances the reported value of T2*w for CVT, as we proved that its sensitivity for CV involvement remains very high even in a blinded reader set-up and that it not only has a high sensitivity but also a high specificity for CVT.
Interobserver agreement
The interobserver agreement for CVT was perfect for FLAIRw (κ = 1), good for T1w and vMRA (κ = 0.73 and 0.75, respectively), and excellent (κ > 0.80) for all other modalities [19, 38], which is considerably higher than has been reported previously for cortical veins [38]. This was most probably due to the fact that our readers were especially focused on the evaluation of the cortical veins. The interobserver agreement for sinus involvement was good to perfect for all modalities, which is consistent with data in the literature [38].
Limitations
Some limitations of our study need to be taken into account. First, the most important problem for the definite extent of the thrombosis is that the final diagnosis was obtained based on a consensus reading and not on an external reference standard. This is due to the fact that there is no gold standard available for the diagnosis of a CVT besides brain tissue examination. As mentioned in the “Introduction,” this is an intrinsic problem of all imaging studies on this topic, which seems to have been neglected in some previous studies. We used T2*w as an internal gold standard in the consensus reading, which is reasonable because all available data on CVT in the literature consistently shows the superiority of T2*w for CVT. Yet, we cannot completely exclude that some affected cortical veins were missed. Second, the presence of indirect signs such as edema or hemorrhage in most patients with CVT might bias the reader towards the diagnosis of CVT or SVT. Third, the retrospective design of the study resulted in the data sets not always being complete for all imaging modalities. The sample size of our study was relatively small, especially with regard to MDCTA. Yet, CVT, especially if isolated, is a rare disease; the 13 patients were assessed by a multiple blinded reader approach, and we included a control group. Thus, the number of cases may not necessarily impair the scope of our observations.
In addition to these limitations, it has to been taken into account that the analysis of isolated MR sequences, as performed here, does not reflect daily clinical practice, in which the complementary information of several sequences is used to establish a diagnosis. Yet, we choose this study design intentionally in order to determine the most useful sequences for CVT and thus to identify an appropriate MR sequence protocol for this challenging diagnosis.
In recent years, susceptibility-weighted sequences, which are more sensitive compared to conventional T2*w sequences with regard to susceptibility artifacts, are used to assess the cerebral venous system [39]. To date, only a very limited number of case reports on its use in patients with cerebral venous occlusions are available, in which the technique yielded promising results [40, 41]. Yet, care has to be taken, as both normal and occluded veins appear hypointense on this sequence. Further research should address the value of SWI, the potential of higher field strengths, and high-resolution contrast-enhanced vMRA for CVT, using T2*w as gold standard.
Conclusion
Our study demonstrated that T2*w is the superior MR sequence for CVT. Besides T2*w, only T1w reached a sensitivity of over 50%, followed by FLAIRw and vMRA. Thus, we recommend that radiologists perform these four sequences if CVT is suspected and that T2*w should be considered as the future gold standard for diagnosing CVT. On the contrary, our results suggest that NCCT but also MDCTA might not be suitable for diagnosing CVT. Furthermore, we would like to raise the radiologist's awareness to the direct signs of CVT, because the presence of these signs was highly specific for CVT on all studied imaging modalities.
References
Oka K, Rhoton AL Jr, Barry M, Rodriguez R (1985) Microsurgical anatomy of the superficial veins of the cerebrum. Neurosurgery 17:711–748
Renowden S (2004) Cerebral venous sinus thrombosis. Eur Radiol 14:215–226
Linn J, Brückmann H (2009) Differential diagnosis of nontraumatic intracerebral hemorrhage. Klin Neuroradiol 19:45–61
Jacobs K, Moulin T, Bogousslavsky J, Woimant F, Dehaene I, Tatu L, Besson G, Assouline E, Casselman J (1996) The stroke syndrome of cortical vein thrombosis. Neurology 47:376–382
Chang R, Friedman DP (2004) Isolated cortical venous thrombosis presenting as subarachnoid hemorrhage: a report of three cases. AJNR Am J Neuroradiol 25:1676–1679
Fellner FA, Fellner C, Aichner FT, Mölzer G (2005) Importance of T2*-weighted gradient-echo MRI for diagnosis of cortical vein thrombosis. Eur J Radiol 56:235–239
Boukobza M, Crassard I, Bousser MG, Chabriat H (2009) MR imaging features of isolated cortical vein thrombosis: diagnosis and follow-up. AJNR Am J Neuroradiol 30:344–348
Albayram S, Kara B, Ipek H, Ozbayrak M, Kantarci F (2009) Isolated cortical venous thrombosis associated with intracranial hypotension syndrome. Headache 49:916–919
Rathakrishnan R, Sharma VK, Chan BP (2009) Isolated cortical vein thrombosis in a patient with arteriovenous malformation. J Clin Neurosci 16:856–857
Thamburaj K, Choudhary A (2009) Hyperintense vessel sign: isolated cortical venous thrombosis after L-asparaginase therapy. Pediatr Radiol 39:757
Cakmak S, Hermier M, Montavont A, Derex L, Mauguière F, Trouillas P, Nighoghossian N (2004) T2*SW-weighted MRI in cortical venous thrombosis. Neurology 63:1698
Duncan IC, Fourie PA (2005) Imaging of cerebral isolated cortical vein thrombosis. AJR Am J Roentgenol 184:1317–1319
Dorndorf D, Wessel K, Kessler C, Kömpf D (1993) Thrombosis of the right vein of Labbé: radiological and clinical findings. Neuroradiology 35:202–204
Urban PP, Müller-Forell W (2005) Clinical and neuroradiological spectrum of isolated cortical vein thrombosis. J Neurol 252:1476–1481
Idbaih A, Boukobza M, Crassard I, Porcher R, Bousser MG, Chabriat H (2006) MRI of clot in cerebral venous thrombosis. High diagnostic value of susceptibility-weighted images. Stroke 37:991–995
Linn J, Pfefferkorn T, Ivanicova K, Müller-Schunk S, Hartz S, Wiesmann M, Dichgans M, Brückmann H (2009) Noncontrast CT in deep cerebral venous thrombosis and sinus thrombosis: comparison of its diagnostic value for both entities. AJNR Am J Neuroradiol 30:728–735
Linn J, Ertl-Wagner B, Seelos KC, Strupp M, Reiser M, Brückmann H, Brüning R (2007) Diagnostic value of multidetector-row CT angiography in the evaluation of thrombosis of the cerebral venous sinuses. AJNR Am J Neuroradiol 28:946–952
Rodallec MH, Krainik A, Feydy A, Hélias A, Colombani JM, Jullès MC, Marteau V, Zins M (2006) Cerebral venous thrombosis and multidetector CT angiography: tips and tricks. Radiographics 26(Suppl 1):5–18
Randolph JJ (2005) Free-marginal multirater kappa: an alternative to Fleiss' fixed-marginal multirater kappa. Joensuu University Learning and Instruction Symposium 2005, October 14–15th, 2005, Joensuu, Finland
Virapongse C, Cazenave C, Quisling R, Sarwar M, Hunter S (1987) The empty delta sign: frequency and significance in 76 cases of dural sinus thrombosis. Radiology 162:779–785
Masuhr F, Mehraein S, Einhäupl K (2004) Cerebral venous and sinus thrombosis. J Neurol 251:11–23
Stam J (2005) Current concepts: thrombosis of the cerebral veins and sinuses. N Engl J Med 352:1791–1798
Chang YJ, Huang CC, Wai YY (1995) Isolated cortical venous thrombosis—discrepancy between clinical features and neuroradiologic findings. A case report. Angiology 46:1133–1138
Wetzel SG, Kirsch E, Stock KW, Kolbe M, Kaim A, Radue EW (1999) Cerebral veins: Comparative study of CT venography with intraarterial digital subtraction angiography. AJNR Am J Neuroradiol 20:249–255
Lafitte F, Boukobza M, Guichard JP, Hoeffel C, Reizine D, Ille O, Woimant F, Merland JJ (1997) MRI and MRA for diagnosis and follow-up of cerebral venous thrombosis (CVT). Clin Radiol 52:672–679
Ayanzen RH, Bird CR, Keller PJ, McCully FJ, Theobald MR, Heiserman JE (2000) Cerebral MR venography: normal anatomy and potential diagnostic pitfalls. AJNR Am J Neuroradiol 21:74–78
Cashen TA, Carr JC, Shin W, Walker MT, Futterer SF, Shaibani A, McCarthy RM, Carroll TJ (2006) Intracranial time-resolved contrast-enhanced MR angiography at 3 T. AJNR Am J Neuroradiol 27:822–829
Roland T, Jacobs J, Rappaport A, Vanheste R, Wilms G, Demaerel P (2010) Unenhanced brain CT is useful to decide on further imaging in suspected venous sinus thrombosis. Clin Radiol 65:34–39
Teasdale E (2000) Cerebral venous thrombosis: making the most of imaging. J R Soc Med 93:234–237
Connor SE, Jarosz JM (2002) Magnetic resonance imaging of cerebral venous sinus thrombosis. Clin Radiol 57:449–461
Hinman JM, Provenzale JM (2002) Hypointense thrombus on T2-weighted MR imaging: a potential pitfall in the diagnosis of dural sinus thrombosis. Eur J Radiol 41:147–152
Favrole P, Guichard JP, Crassard I, Bousser MG, Chabriat H (2004) Diffusion-weighted imaging of intravascular clots in cerebral venous thrombosis. Stroke 35:99–103
Lövblad KO, Bassetti C, Schneider J, Guzman R, El-Koussy M, Remonda L, Schroth G (2001) Diffusion-weighted MR in cerebral venous thrombosis. Cerebrovasc Dis 11:169–176
Selim M, Fink J, Lingante I, Kumar S, Schlaug G, Caplan LR (2002) Diagnosis of cerebral venous thrombosis with echo-planar T2*SW-weighted magnetic resonance imaging. Arch Neurol 59:1021–1026
Leach JL, Strub WM, Gaskill-Shipley MF (2007) Cerebral venous thrombus signal intensity and susceptibility effects on gradient recalled-echo MR imaging. AJNR Am J Neuroradiol 28:940–945
Spitzer C, Mull M, Rohde V, Kosinski CM (2005) Non-traumatic cortical subarachnoid haemorrhage: diagnostic work-up and aetiological background. Neuroradiology 47:525–531
Linn J, Herms J, Dichgans M, Brückmann H, Fesl G, Freilinger T, Wiesmann M (2008) Subarachnoid hemosiderosis and superficial cortical hemosiderosis in cerebral amyloid angiopathy. AJNR Am J Neuroradiol 29:184–186
Ferro JM, Morgado C, Sousa R, Canhão P (2007) Interobserver agreement in the magnetic resonance location of cerebral vein and dural sinus thrombosis. Eur J Neurol 14:353–356
Haacke EM, Mittal S, Wu Z, Neelavalli J, Cheng YC (2009) Susceptibility-weighted imaging: technical aspects and clinical applications, part 1. AJNR Am J Neuroradiol 30:19–30
Kawabori M, Kuroda S, Kudo K, Terae S, Kaneda M, Nakayama N, Iwasaki Y (2009) Susceptibility-weighted magnetic resonance imaging detects impaired cerebral hemodynamics in the superior sagittal sinus thrombosis—case report. Neurol Med Chir (Tokyo) 49:248–251
Linn J, Bruckmann H (2010) Cerebral vein and dural sinus thrombosis—state of the are imaging. Klin Neuroradiol (in press)
Acknowledgments
We thank Dr. V. Schöpf for reviewing the statistics and T. Wesemann for technical assistance.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linn, J., Michl, S., Katja, B. et al. Cortical vein thrombosis: the diagnostic value of different imaging modalities. Neuroradiology 52, 899–911 (2010). https://doi.org/10.1007/s00234-010-0654-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-010-0654-0