Abstract
Purpose
The purpose of this study was to investigate characteristics, drug use patterns, and predictors for treatment choice in older German patients initiating antidepressant (AD) treatment.
Methods
Using the German Pharmacoepidemiological Research Database, we identified a cohort of AD initiators aged at least 65 years between 2005 and 2011. Potential indications, co-morbidity, and co-medication as well as treatment patterns such as the duration of the first treatment episode were assessed. In addition, a logistic regression model was used to identify independent predictors for initiating treatment with tricyclic ADs (TCAs) compared to selective serotonin reuptake inhibitors (SSRIs).
Results
Overall, 508,810 individuals were included in the cohort. About 55 % of patients initiated AD treatment with TCAs, followed by 22 % receiving SSRIs. During the study period, a decrease of treatment initiation with TCAs was observed. Higher age and male sex as well as being diagnosed with depression were highly associated with SSRI treatment, whereas pain and sleeping disorders were strong predictors for initiating TCA treatment. The duration of the first treatment episode was substantially longer in SSRI users compared to TCA initiators (median 119 vs. 43 days).
Conclusions
Potential indications and drug use patterns in older German AD initiators varied substantially for different drug classes and single agents. Given the anticholinergic and sedative properties of TCAs, the frequent use of this drug class though probably related to indications such as pain was remarkable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decades, antidepressant (AD) use has increased substantially. According to a report for 23 countries by the Organization for Economic Cooperation and Development (OECD), AD consumption per 1000 persons has increased from 31 defined daily doses (DDDs) in 2000 to 56 DDDs in 2011 [1]. In Germany, an incline of DDDs by the factor 1.8 was reported from 2005 to 2011 [2]. While tricyclic ADs (TCAs) remained relatively constant during this time period, use of selective serotonin reuptake inhibitors (SSRIs) more than doubled, and newer drug classes showed even steeper increases [2].
Besides the diagnosis of depression, ADs are increasingly used for other indications such as pain or insomnia [3] that constitute common disorders in the older population [4]. However, in older people, several TCAs such as amitriptyline have been considered potentially inappropriate based on their peripheral and central anticholinergic side effects, association with cognitive deficits, and an increased risk of falling [5, 6]. Other ADs considered potentially inappropriate include the SSRI fluoxetine because of side effects affecting the central nervous system or the risk of hyponatremia [5, 6].
Although ADs are frequently prescribed to older patients, studies investigating utilization of specific AD drug classes and agents in Germany so far have focused on children and adolescents [7, 8] or were restricted to elderly individuals of one urban region [9]. Therefore, we aimed to examine characteristics, drug use patterns, and predictors for treatment choice in a large population-based cohort of older AD initiators from all over Germany.
Methods
Data source
Source of data was the German Pharmacoepidemiological Research Database (GePaRD) established by the Leibniz Institute for Prevention Research and Epidemiology–BIPS. The database contains information from four statutory health insurance providers (SHIs) covering over 20 million insured members across Germany. GePaRD includes demographic characteristics for each person, information on hospitalizations, and outpatient physician visits as well as on outpatient prescriptions. Hospital data encompass the periods of hospitalization, the reasons for admission and discharge, and diagnostic and therapeutic procedures. Reimbursed on a quarterly basis, claims of outpatient physician visits contain diagnoses, treatments, and procedures. All diagnoses from the inpatient and outpatient setting are based on the German modification of the International Classification of Diseases, 10th revision (ICD-10-GM). Prescription data are limited to reimbursable drugs and include prescribing and dispensation dates, the amount of substance prescribed, and information on the prescribing physician. Linkage to a reference database adds information on the anatomical-therapeutic-chemical (ATC) code, the DDD, and the generic and trade names. With a few exceptions, in-hospital medication is not included in GePaRD.
In Germany, the use of health insurance data for scientific research is regulated by the Code of Social Law. All involved SHIs, as well as the federal and regional authorities, approved use of the data for this study. Patient informed consent was not required by law as the study was based on pseudonymous data.
Study population
During the study period of 2005 to 2011, patients aged 65 years or older entered the cohort on the day of their first outpatient AD dispensation (index AD), if they had been continuously insured for a minimum of 1 year before this date and no AD had been dispensed in this time period. Cohort exit was defined as the first of the following dates: (i) interruption of insurance time for more than 3 days, (ii) end of insurance period (including death), or (iii) end of study period.
Drug exposure
ADs were classified as (i) TCAs, (ii) SSRIs, (iii) selective serotonin noradrenaline reuptake inhibitors (SSNRIs), (iv) noradrenergic and specific serotonergic antidepressants (NASSAs), (v) noradrenaline reuptake inhibitors (NARIs), (vi) monoamine oxidase inhibitors (MAOs), (vii) herbal ADs including St. John’s wort, homeopathic, or anthroposophic ADs, and (viii) other ADs (see ESM 1 for further information). The first dispensation was defined as index AD. Patients receiving multiple AD classes on the day of cohort entry were assigned to a separate category. The duration of each dispensation was estimated based on the number of dispensed DDDs. To account for lower doses often used in elderly persons [10], 150 % of the respective DDD supply were added to each dispensation [11]. Continuous treatment of subsequent dispensations was assumed if the calculated end of a dispensation overlapped with the following dispensation [12]. Stockpiling was not considered; i.e., each dispensation was assumed to start immediately and potentially overlapping supply was discarded [13].
Covariates
Based on inpatient and confirmed outpatient diagnoses, co-morbidity was determined in the year before cohort entry. Additionally, the “Charlson co-morbidity index (CCI)” [14] and accommodation in a nursing home or residential care based on hospital discharge information and ambulatory procedural codes were assessed in this time period. Co-medication was ascertained in the year before cohort entry and during time in cohort. Potential indications for AD use including depression, pain, sleeping and anxiety disorders (see ESM 2 for further information) were examined on the day of cohort entry and in the 6 months prior to this date. For patients with a coded depression, we further assessed its severity in a hierarchical approach: (i) severe (recurrent/non-recurrent), (ii) moderate, (iii) mild, (iv) dysthymia, and (v) unspecified.
Data analyses
Descriptive analyses were conducted with respect to sex, age at cohort entry, potential indications, co-morbidity, and co-medication. Over the 7-year study period, we further assessed whether the class of the index dispensation changed over time. Examined treatment patterns encompassed the specialty of the prescribing physician, the number of different AD agents used during follow-up, the duration of the first treatment episode, and the number of treatment episodes during follow-up. In addition, a logistic regression model was used to identify independent predictors for initiating treatment with TCA compared to SSRI including baseline covariates and the specialty of the prescribing physician.
Subgroup analyses were conducted for patients with diagnosed depression. In two sensitivity analyses, 50 and 300 % of supply were added to each dispensation as described above, respectively.
All analyses were performed with SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of AD initiators
During the study period, 508,810 persons aged 65 years or older initiated AD treatment. Median age at cohort entry was 73 years, and 70 % of users were female. About 55 % of patients entered the cohort with a TCA drug, followed by 22 % receiving SSRI treatment as index AD. Women were more likely to receive a TCA on the day of cohort entry compared to men (57.0 vs. 51.4 %). In contrast, they initiated SSRI treatment less often (20.7 vs. 24.7 %). Depression as potential indication for AD use was more common in women than in men (48.5 vs. 41.2 %; Table 1).
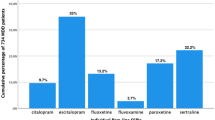
From 2005 to 2011, a decrease in treatment initiation with TCAs from 62.3 to 48.2 % was observed, whereas use of SSRIs and NASSAs increased from 18.9 to 24.8 % and from 9.7 to 17.2 %, respectively (Fig. 1). While amitriptyline and opipramol were the most common index ADs in the overall study population, patients with a diagnosed depression were far more likely to initiate treatment with citalopram (ESM 3).
Class of index AD dispensation from 2005 to 2011. AD antidepressant, MAO monoamine oxidase inhibitor, NARI noradrenaline reuptake inhibitor, NASSA noradrenergic and specific serotonergic antidepressant, SSNRI selective serotonin noradrenaline reuptake inhibitor, SSRI selective serotonin reuptake inhibitor, TCA tricyclic antidepressant
Potential indications, clinical characteristics, and co-medication
Depression as potential indication was found in less than 40 % of patients with a tricyclic index AD, whereas about 70 % of patients initiating treatment with herbal ADs and nearly 60 % starting therapy with SSRIs had that diagnosis (Table 2). Sleeping disorders were diagnosed in more than 21 % of NASSA or TCA users and in only 14 % of patients treated with SSRIs or herbal ADs. Pain as potential indication was most often found in initiators of SSNRI and TCA (76.9 and 72.3 %, respectively).
With regard to co-morbidity, cerebrovascular disease and dementia were far more common in SSRI initiators than in patients starting TCA treatment (33.9 vs. 20.2 % and 14.1 vs. 3.7 %, respectively). Cardiovascular co-morbidity such as congestive heart failure or coronary heart disease was most often found in users of SSRI or NASSA and was comparatively rare in patients initiating tricyclic or herbal ADs. Accordingly, the highest CCI (median 3) was observed for SSRI and SSNRI initiators, and the lowest value was found in patients receiving herbal ADs (median 1). Further, the highest proportion of nursing home residents was observed among SSRI users (9.1 %). More than half of the patients treated with SSNRI had a diagnosis of diabetes. The highest prevalence of opioid co-medication was found in SSNRI users (49.4 %) followed by those receiving TCAs (46.6 %). In contrast, hypnotic or sedative drugs were most often co-prescribed to patients initiating NASSAs.
Regarding specific ADs, depression was most common among users of citalopram (62.0 %) and least frequently diagnosed in patients initiating amitriptyline treatment (38.4 %; ESM 4). Sleeping disorders were most common in users of trimipramine (31.6 %), whereas pain was most often diagnosed in those treated with amitriptyline (78.3 %), and the highest prevalence of anxiety diagnoses was observed in opipramol initiators (17.2 %).
Predictors for treatment choice
Higher age and male sex were associated with SSRI treatment initiation (Fig. 2). Considering potential indications for AD use, sleeping disorders were found to be the strongest predictor for initiating AD treatment with TCAs (adjusted odds ratio (aOR) 1.80; 95 % CI 1.76–1.83) followed by pain (aOR 1.59; 95 % CI 1.56–1.61), whereas being diagnosed with depression increased the probability of SSRI therapy. Dementia and cerebrovascular disease as well as living in a nursing home (aOR 0.54; 95 % CI 0.52–0.55) were highly associated with SSRI treatment as compared to TCA therapy.
Predictors of treatment with TCA vs. SSRI. CI confidence interval, EPM extrapyramidal and movement disorders, GP general practitioner, OR odds ratio, SSRI selective serotonin reuptake inhibitor, TCA tricyclic antidepressant. Note that the reference group “GP/other” includes the specialties “GP/internist,” “other/unknown,” and “multiple physician specialties.” The specialty of the prescribing physician refers to the index dispensation. Adjusted ORs <1.0 predict treatment initiation with SSRIs, and adjusted ORs >1.0 predict treatment inititation with TCAs
Treatment patterns
Different ADs during the study period were most often prescribed to patients initiating herbal ADs and least often to those with NASSA index ADs (Table 3). Nearly one quarter of SSRI or SSNRI index prescriptions was issued by neurologists or psychiatrists, whereas only 14.3 % of index TCAs were prescribed by this physician specialty. Though overall low, the highest proportion of anesthesiologists as index prescribers was found among SSNRI and TCA users.
The median duration of the first treatment episode was 204 days in patients initiating herbal ADs and 191 days in SSRI users, whereas TCA initiators revealed substantially shorter median treatment duration (43 days). More than 63 % of patients initiating treatment with herbal ADs or SSRIs had only one treatment episode, whereas this applied to only 46 % of TCA users.
Adding 50 % of supply to each dispensation revealed shorter median treatment episodes compared to the main analysis, whereas allowing 300 % of supply between subsequent dispensations prolonged the assumed duration of treatment, respectively (ESM 5). However, as in the main analysis, the shortest durations were observed for TCA users, whereas patients treated with herbal ADs or SSRIs revealed substantially longer treatment episodes in both sensitivity analyses.
Patients with depression
Among patients with a diagnosed depression, the proportion of TCA initiators was lower compared to the overall study population (43.5 vs. 55.3 %). A severe episode was more common in patients treated with SSNRIs or NASSAs, whereas moderate episodes were most often diagnosed in patients initiating herbal ADs (ESM 6). Overall, about 60 % of patients with depression only had unspecific diagnoses. Other potential indications such as pain, anxiety, and sleeping disorders were slightly higher in patients with depression compared to the overall cohort. For example, about three quarters of TCA or SSNRI users with depression were also diagnosed with pain. The duration of the first treatment episode was longer in patients with depression than in the overall study population (median 85 vs. 64 days), although the short median duration of 43 days for TCAs was also observed in this subgroup. Further, patients with depression were more likely to receive different ADs during the study period.
Discussion
To our knowledge, this is the first study assessing characteristics and drug use patterns of AD drug classes and agents in a large cohort of older AD initiators from all over Germany. In this study, we found a remarkably high proportion of TCA-treated patients, although recommendations generally tend towards other drug classes in this age group [5, 6]. In contrast to our findings, several studies from other countries observed lower proportions of TCA use in older patients [10, 15, 16]. Though not restricted to a specific age group, a study reporting annual prevalences for AD use in seven European electronic health care databases found that SSRIs were prescribed more often than TCAs in all except the German population [17].
Although TCAs constituted the largest index AD class in all seven study years, we observed a trend towards more frequent treatment initiation with SSRIs and NASSAs over the years probably mirroring respective recommendations for older persons [5]. Besides the year of cohort entry, the decision for the first AD class was highly influenced by the potential indication for use with sleeping disorders and pain predicting TCA use, whereas depression was strongly associated with SSRI treatment. The specialties of the prescribing physicians and also the prevalences regarding co-medication supported these findings.
Overall, the potential reasons for treatment choice observed in our study were in line with formally approved indications or known use of the respective agents of each class. One example is the use of TCAs as well as ADs with combined serotonergic and noradrenergic effects such as mirtazapine, venlafaxine, or duloxetine in pain therapy [18]. Approval of the latter drug for pain due to diabetic polyneuropathy probably explains the remarkably high prevalence of diabetes among SSNRI initiators. Further, the sedative properties of the TCAs trimipramine and doxepin but also the NASSA mirtazapine promote their use in sleeping disorders in the setting of geriatric psychiatry [19]. The overall tendency to prescribe ADs for indications other than depression was also observed in a Dutch study, which reported a decreasing percentage of depression as an indication from 65 % in 1996 to 47 % in 2012 [20].
Given that SSRIs are generally considered first-line treatment in older patients with depression, the high proportion of TCA initiators among patients with that diagnosis was remarkable. However, the large proportion of other potential indications in this subgroup suggests that also in these patients, ADs may have been used to treat pain, insomnia, or other conditions. Especially the high overlap of diagnosed depression and pain reflecting the complex relationship between those two disorders [21] was noteworthy. Though in older patients, TCAs such as amitriptyline have been considered inappropriate because of their strong anticholinergic and sedative properties [5, 6], it has been discussed whether indications related to pain should be exempt from these recommendations [22]. As a consequence, the “Screening Tool of Older Persons’ potentially inappropriate Prescriptions” (STOPP) highlights the clinical situations where prescribing any TCA is potentially inappropriate, e.g., in older patients with dementia or cardiac conduction abnormalities but allows freedom to use these ADs in situations where their use may be indicated, such as low-dose amitriptyline in chronic pain syndromes [23]. With respect to co-medication, also the high proportion of hypnotic or sedative use in more than one quarter of TCA-treated patients with depression warrants attention given the sedative properties of this AD class.
Overall, the proportion of mild depression for which mainly non-pharmacological treatment is recommended [24, 25] was similar across most AD classes. However, the comparatively low proportion of moderate and severe episodes among TCA users again supports the assumption that TCAs might have been prescribed for other indications.
Cerebrovascular diseases, dementia, and living in a nursing home were more prevalent in users of SSRIs compared to TCAs and the other AD classes. These findings are plausible since TCAs are not recommended for use in patients with dementia because of their anticholinergic properties. Further, SSRIs such as citalopram have been shown to reduce agitation in patients with probable Alzheimer’s disease [26], supporting use in these patients. With respect to cardiovascular co-morbidity, the tendency to prescribe SSRIs we observed is probably explained by the fact that those ADs are considered to have a superior cardiovascular safety profile compared to TCA [27].
Median treatment durations differed substantially depending on the index drug class. For the subgroup of patients with depression, not unexpectedly longer treatment periods were observed, since treatment for an overall duration of 6 to 12 months is recommended to reduce the risk of relapse in these patients [3]. In line with our findings, a cohort study of AD initiators in the Australian veteran population from 2005 and 2008 found a median duration for SSRI treatment of 184 days [28]. Although in our study the median treatment duration differed based on the assumed duration of supply, overall patterns were similar with longer durations observed for users of SSRIs and shortest durations for users of TCAs reflecting the different treatment indications for these classes.
In our study, patients receiving ADs recommended for the treatment of depression in older patients such as SSRIs were most likely to have only one treatment episode, which was also shown by an Italian study reporting the highest proportion of continuous users in SSRI-treated older patients [15]. In contrast, we found multiple treatment episodes for index ADs used for a broader spectrum of indications. The largest proportion of multiple treatment episodes, for example, was observed in users of trimipramine, for whom also the highest prevalence of sleeping disorders was found implying that these drugs were likely used “as needed” and/or at lower daily dosages compared to the DDD [29].
Overall, a comparison of the different AD classes to other studies is hampered by AD availability across countries. For example, opipramol, the second most common TCA in our study contributing substantially to the large proportion of this AD class, is very popular in Germany and other European countries but not approved in the USA [30]. Further, indications but also warnings and contraindications can differ. A study analyzing the concordance of prescribing information of psychiatric drugs across four major drug markets, for example, observed especially large variations for the TCAs doxepin and amitriptyline [31].
The main strength of this study is the size of GePaRD, which covers approximately 20 % of the German population. By using pharmacy dispensing data for exposure information recall bias can be ruled out even for older patients with dementia or living in nursing homes and information is regarded to be precise in time, product, and dispensed dose [32]. As ADs are available on prescription only, ascertainment of exposure is assumed to be complete with the exception of St. John’s wort which is also sold over the counter.
As a limitation, it is not clear if persons filling a prescription actually take the drug as indicated or if it is used at all. Further, GePaRD does not provide prescribed daily doses or intended treatment durations. Thus, ADs might have been used in lower doses or only as needed, which was hinted at in our sensitivity analyses. Although we assessed potential indications examining inpatient and outpatient diagnoses, a validation of the actual reason for the respective AD treatment through chart review was not possible. Therefore, the large overlap of indications as, for example, observed for depression and pain limits the evaluation of appropriate AD use with respect to recent recommendations.
In conclusion, potential indications and drug use patterns in older German AD initiators varied substantially for different drug classes and single agents with overall plausible treatment patterns. The frequent use of TCAs in our study might raise concerns; however, the high proportion of potential indications other than depression and the observed treatment patterns indicate that TCAs might have been used to treat pain or insomnia. Still, the anticholinergic and sedative properties of this drug class have to be kept in mind, and recommendations with respect to co-morbidity, co-medication, and dosage for older patients should be considered.
References
Organisation for Economic Cooperation and Development (OECD) (2013) Health at a Glance 2013 OECD INDICATORS. doi:10.1787/health_glance-2013-en
Lohse MJ, Müller-Oerlinghausen B (2012) Psychopharmaka. In: Schwabe U, Paffrath D (eds) Arzneiverordnungs-Report 2012. Berlin, Heidelberg, pp 833–879
Benkert O, Hippius H (2015) Kompendium der Psychiatrischen Pharmakotherapie. doi:10.1007/978-3-642-54769-0
Maercker A (2015) Alterspsychotherapie und klinische Gerontopsychologie. doi:10.1007/978-3-642-54723-2
Holt S, Schmiedl S, Thürmann PA (2010) Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int 107:543–551. doi:10.3238/arztebl.2010.0543
Renom-Guiteras A, Meyer G, Thürmann PA (2015) The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. doi:10.1007/s00228-015-1860-9
Dörks M, Langner I, Dittmann U et al (2013) Antidepressant drug use and off-label prescribing in children and adolescents in Germany: results from a large population-based cohort study. Eur Child Adolesc Psychiatry 22:511–518. doi:10.1007/s00787-013-0395-9
Hoffmann F, Glaeske G, Bachmann CJ (2014) Trends in antidepressant prescriptions for children and adolescents in Germany from 2005 to 2012. Pharmacoepidemiol Drug Saf 23:1268–1272. doi:10.1002/pds.3649
Riedel-Heller SG, Matschinger H, Schork A, Angermeyer MC (2001) The utilization of antidepressants in community-dwelling and institutionalized elderly—results form a representative survey in Germany. Pharmacopsychiatry 34:6–12. doi:10.1055/s-2001-15186
Coupland C, Dhiman P, Morriss R, Arthur A (2011) Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 343:d4551. doi:10.1136/bmj.d4551
Gardarsdottir H, Souverein PC, Egberts TCG, Heerdink ER (2010) Construction of drug treatment episodes from drug-dispensing histories is influenced by the gap length. J Clin Epidemiol 63:422–427. doi:10.1016/j.jclinepi.2009.07.001
Schmedt N, Jobski K, Kollhorst B et al (2016) Treatment patterns and characteristics of older antipsychotic users in Germany. Int Clin Psychopharmacol. doi:10.1097/YIC.0000000000000119
Greevy RA, Huizinga MM, Roumie CL et al (2011) Comparisons of persistence and durability among three oral antidiabetic therapies using electronic prescription-fill data: the impact of adherence requirements and stockpiling. Clin Pharmacol Ther 90:813–819. doi:10.1038/clpt.2011.228
Quan H, Li B, Couris CM et al (2011) Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682. doi:10.1093/aje/kwq433
Sultana J, Italiano D, Spina E et al (2014) Changes in the prescribing pattern of antidepressant drugs in elderly patients: an Italian, nationwide, population-based study. Eur J Clin Pharmacol 70:469–478. doi:10.1007/s00228-013-1636-z
Trifiro G, Dieleman J, Sen EF et al (2010) Risk of ischemic stroke associated with antidepressant drug use in elderly persons. J Clin Psychopharmacol 30:252–258
Abbing-Karahagopian V, Huerta C, Souverein PC et al (2014) Antidepressant prescribing in five European countries: application of common definitions to assess the prevalence, clinical observations, and methodological implications. Eur J Clin Pharmacol 70:849–857. doi:10.1007/s00228-014-1676-z
Lemmer B, Brune K (2010) Pharmakotherapie, 14th ed. doi:10.1007/978-3-642-10541-8
Kamphuis J, Taxis K, Schuiling-Veninga CCM et al (2015) Off-label prescriptions of low-dose quetiapine and mirtazapine for insomnia in the Netherlands. J Clin Psychopharmacol 35:468–470. doi:10.1097/JCP.0000000000000338
Noordam R, Aarts N, Verhamme KM et al (2015) Prescription and indication trends of antidepressant drugs in the Netherlands between 1996 and 2012: a dynamic population-based study. Eur J Clin Pharmacol 71:369–375. doi:10.1007/s00228-014-1803-x
Goesling J, Clauw DJ, Hassett AL (2013) Pain and depression: an integrative review of neurobiological and psychological factors. Curr Psychiatry Rep. doi:10.1007/s11920-013-0421-0
Gehling M (2010) Correspondence (letter to the editor): pain therapy. Dtsch Ärzteblatt Int 107:900 . doi:10.3238/arztebl.2010.0900a author reply 900–901
Gallagher P, O’Mahony D (2008) STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with beers’ criteria. Age Ageing 37:673–679. doi:10.1093/ageing/afn197
Deutsche Gesellschaft für Psychiatrie Psychotherapie und Nervenheilkunde (DGPP (2009) S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression-Kurzfassung. https://www.dgppn.de/fileadmin/user_upload/_medien/download/pdf/kurzversion-leitlinien/s3-nvl-unipolare-depression-kf.pdf. Accessed 7 Feb 2016
Deutsche Gesellschaft für Psychiatrie Psychotherapie Psychosomatik und Nervenheilkunde (DGPPN) (2015) S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression. http://www.leitlinien.de/mdb/downloads/nvl/depression/depression-2aufl-vers2-lang.pdf. Accessed 7 Feb 2016
Porsteinsson AP, Drye LT, Pollock BG et al (2014) Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA 311:682–691. doi:10.1001/jama.2014.93
Spina E, Trifirò G (2016) Pharmacovigilance in psychiatry. doi:10.1007/978-3-319-24741-0
Lu CY, Roughead E (2012) New users of antidepressant medications: first episode duration and predictors of discontinuation. Eur J Clin Pharmacol 68:65–71. doi:10.1007/s00228-011-1087-3
Wiegand MH (2008) Antidepressants for the treatment of insomnia: a suitable approach? Drugs 68:2411–2417. doi:10.2165/0003495-200868170-00001
Wehling M (2013) Drug Therapy for the Elderly. doi:10.1007/978-3-7091-0912-0
Pfistermeister B, Schenk C, Kornhuber J et al (2013) Different indications, warnings and precautions, and contraindications for the same drug-an international comparison of prescribing information for commonly used psychiatric drugs. Pharmacoepidemiol Drug Saf 22:329–333. doi:10.1002/pds.3389
Schneeweiss S, Avorn J (2005) A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol 58:323–337. doi:10.1016/j.jclinepi.2004.10.012
Acknowledgments
The authors would like to thank all statutory health insurances for providing data for this study, namely, the TK, AOK Bremen/Bremerhaven, DAK-Gesundheit, and the Handelskrankenkasse. They also want to thank Inga Schaffer, Sandra Ulrich, and Marieke Niemeyer for contributing to the statistical analyses and Heike Gerds for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was funded by the Federal Institute for Drugs and Medical Devices. Kathrin Jobski, Niklas Schmedt, Tania Schink, Bianca Kollhorst, and Edeltraut Garbe, as employees of the Leibniz Institute for Prevention Research and Epidemiology–BIPS, have performed research studies sponsored by pharmaceutical companies (Bayer-Schering, Celgene, GSK, Mundipharma, Novartis, Purdue, Sanofi-Aventis, Sanofi-Pasteur MSD, Stada, and Takeda) unrelated to this study. Edeltraut Garbe has been consultant to Bayer, Nycomed, Takeda, Astellas, Novartis, and GSK unrelated to the subject of this study. Jutta Krappweis declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Jobski, K., Schmedt, N., Kollhorst, B. et al. Characteristics and drug use patterns of older antidepressant initiators in Germany. Eur J Clin Pharmacol 73, 105–113 (2017). https://doi.org/10.1007/s00228-016-2145-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2145-7