Abstract
Purpose
To assess the prevalence of hospital admission related to adverse drug reactions (ADRs) in a third-level hospital, to analyse the associated factors, and to describe the reactions and the drugs involved.
Methods
A cross-sectional study was conducted for a 120-day period. Patients that were urgently hospitalized entered the study. The primary endpoint was the ADR-related urgent admission. A descriptive analysis of demographic, clinical, and drug-related variables was performed. The association between the likelihood of urgent admission due to ADRs and age, gender, and number of drugs used was analysed. A descriptive analysis of the suspected drugs and the reactions in ADR-related admissions was performed.
Results
Overall, 186 out of 4,403 hospital admissions were due to ADRs (prevalence: 4.2 % [95 % CI 3.7–4.8 %]). Age (≥65 years: OR 1.59 [95 % CI 1.10–2.29]) and number of drugs used at the time of admission (3–5 drugs: OR 5.07 [95 % CI 2.71–9.59]; 6–9 drugs: OR 5.90 [95 % CI 3.16–11.0]; ≥10 drugs: OR 8.94 [95 % CI 4.73–16.89]), but not gender, were identified as independent factors associated with ADR-related hospitalization. The overall in-hospital stay for patients admitted with ADRs amounted to 1,785 days. The ADRs were mainly type A reactions (92 %). Acute renal failure related to renin-angiotensin system inhibitors, haemorrhage due to anticoagulants, and upper gastrointestinal bleeding related to antiplatelet drugs and/or non-steroidal anti-inflammatory drugs were the most frequent.
Conclusion
Over 4 % of urgent hospitalizations are caused by ADRs, which are dose-related and predictable in more than 90 % of cases. The main risk factors are advanced age and polypharmacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adverse drug reactions (ADRs) are a major public health problem because of their impact in terms of morbidity, mortality and economic cost. Meta-analyses of studies on the frequency of ADRs as a cause of hospitalization in Western countries provide figures that range between 3.7 and 5.3 % [1–3]. The variability between the studies included in those meta-analyses can be explained, at least in part, by differences in study designs, type of events studied, definition of ADR applied, methods of identifying cases, methods of assessment of causality, length of periods of study and wards included [4]. Although most published studies of ADRs have applied the WHO definition [5], the new European pharmacovigilance legislation has put into force a wider definition [6].
In our hospital, with a Service of Clinical Pharmacology and a prospective pharmacovigilance programme (PhvP) recently set up (i.e. in 2007 and 2008, respectively), the information currently available in the scientific literature on frequency and characteristics of ADR-related hospital admissions did not allow us to properly size up the problem and to plan actions in this regard based on reliable and updated local data. The aim of this study was therefore: (i) to assess the prevalence of ADR-related hospital admission in a third-level teaching hospital, taking into account the current European definition of ADR, (ii) to analyse the factors associated, (iii) to characterize the ADRs, and (iv) to describe the drugs involved.
Methods
Study design
A cross-sectional study was carried out at Bellvitge University Hospital, a Spanish tertiary care teaching hospital. It has approximately 800 beds, covers a population of approximately 1.3 million inhabitants and provides all medical and surgical specialities except for obstetrics, gynaecology, paediatrics, and oncology. The period of study was 120 days. All patients admitted through the emergency room during the first 10 days of each month during a period of 12 consecutive months (from July 2009 to June 2010) were included. The study was approved by the Clinical Research Ethics Committee of Bellvitge University Hospital. All identified cases of ADRs were reported to the Spanish Pharmacovigilance System (SPhVS).
Data collection and variables studied
The source of identification of patients was the daily list of urgent admissions provided by the Admissions Unit. For each patient, demographic data (age and sex), clinical information (admission diagnosis, medical ward and length of hospital stay), as well as information on the number of different drugs used at the time of arrival at the hospital were gathered. The information was obtained from the medical electronic records.
Definition and ascertainment of cases of ADR
The primary endpoint was urgent admission caused by an ADR. We used the definition of ADR utilized by the SPhVS [7] that corresponds with the one currently in force in the regulatory framework of the European Union, which considers as an ADR any response to a drug which is noxious and unintended [6].
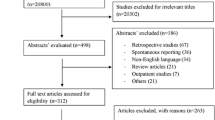
Cases of ADRs included in the present study are a sample of those identified within the context of the prospective PhVP that we have been running in our hospital since 2008. Our PhVP collects cases of ADRs identified by a systematic daily review of admission diagnoses. Patients admitted with diagnoses included in a pre-defined list of diseases or syndromes potentially caused by drugs (see Supplementary Material, Figure 1) are selected for further review. Their medical records are reviewed by a clinical pharmacologist in order to make a clinical judgement about the possibility of an ADR by applying the causality assessment methods and the algorithm of the SPhVS (a modification of the algorithm of Karch-Lassagna) [8], which categorises imputability as improbable, conditional, possible, probable or definite (see Supplementary Material). When an ADR is initially suspected, a trained nurse collects information on the drugs taken and the reaction from the medical record or by direct patient interview. Each case is followed up until discharge to gather enough information to discard or retain it as a case of suspected ADR. A clinical pharmacologist makes a final causality assessment in those cases retained as suspected ADRs. Admissions with insufficient information for a reliable assessment, as well as improbable ADR cases are excluded. The information regarding each individual ADR case is incorporated into a database. Drugs are coded as suspected, not suspected, or suspected of pharmacological interaction. The Anatomical Therapeutic Chemical Classification (ATC) [9] and the Medical Dictionary for Regulatory Activities (MedDRA) version 11.0. are used to code active principles and reactions, respectively. The outcome of the ADR is categorised into recovered, recovered with sequelae, not yet recovered, death from the ADR, death from other causes, or outcome unknown.
For the purposes of this study, cases of ADRs with date of admission within the study period were retrieved from the PhVP database. Additionally, the reactions were classified according to their mechanism of production into type A or type B [10].
Sample size calculation
We calculated that 4,098 patients were needed for inclusion in the study in order to estimate the proportion of patients admitted for an ADR with 95 % confidence interval (CI), and with a CI width of 1.2 % (margin of error: 0.6 %), taking into account an expected frequency of 4 % based on the results of published meta-analyses and previous studies performed in Spain [1–3, 11–13].
Statistical analysis
The prevalence of ADR-related admission was calculated by dividing the number of patients admitted for ADRs and the total number of admissions through the emergency room during the study period. We calculated the 95 % CI for this estimate.
We performed a descriptive analysis of demographic, clinical, and drug-related variables stratified by the condition of interest (ADR-related admission). We calculated absolute and relative frequencies for qualitative variables (gender, age group, number of drugs used at admission categorised, and stay in special units —Intensive Care Unit and Recovery Unit), as well as median, interquartile range (IQR) and range for continuous variables (age, number of medications, total length of hospital stay, and length of stay in special units). The chi-squared test was used to compare the distribution of categorical variables. Continuous variables were tested for normality; the t test or the Mann–Whitney test (when appropriate) was used to compare the distribution of continuous variables. In the subset of patients admitted for ADRs, we performed a descriptive analysis of suspected drugs, type of reactions, mechanism of production, and outcome. Absolute and relative frequencies were calculated.
The association between the likelihood of urgent hospital admission due to ADR and age, gender, and number of drugs being taken at admission—which were defined as covariates a priori—was analysed in a logistic regression model. Covariates that were significant in a Wald test at a p-value of decision 0.1 were selected for the final model.
Statistical analysis was performed with SPSS version 15.0 (Chicago, Illinois, USA).
Results
During the study period, 4,403 patients were urgently admitted to our hospital. There were 1,352 patients with admission diagnoses included on the list of syndromes and diseases suggestive of ADRs. ADRs were actually suspected as the reasons for hospitalization in 186 of these patients, resulting in an estimated prevalence of ADR-related hospital admission of 4.2 % (95 % CI 3.7–4.8 %).
Patients admitted for ADRs were older and were taking a greater number of drugs than those admitted for other reasons. No differences in gender distribution were seen between both groups (Table 1). The length of hospital stay of ADR-related hospital admissions was shorter, but the proportion of patients requiring stay in special units was higher in those admitted for ADRs. Overall, ADR-related hospital admissions resulted in 1,785 days of hospital stay, 150 of them in special units (Table 1). The logistic regression analysis identified the age and the number of drugs being taken at admission as independent factors associated with hospitalization due to ADR (Table 2).
The 186 cases included 201 ADRs and 382 suspected drugs. The most common reactions were renal and urinary disorders (29.4 %; n = 59) followed by gastrointestinal and nervous system disorders (26.4 % [n = 53] and 10.4 % [n = 21], respectively). They were type A reactions in 91.9 % of cases (n = 171) and type B in 8.1 % (n = 15). The therapeutic subgroups with a larger number of suspected pharmacological exposures were diuretics (18.1 %; n = 69), antithrombotic drugs (16.5 %; n = 63), renin-angiotensin system (RAS) inhibitors (14.7 %; n = 56) and non-steroidal anti-inflammatory drugs (NSAIDs; 11.3 %; n = 43). A pharmacological interaction was suspected in 95 cases (51.1 %). The most common drug-reaction associations were acute renal failure (ARF) related to RAS inhibitors with or without concomitant diuretics and/or NSAIDs, bleeding from various locations due to anticoagulant therapy, and upper gastrointestinal bleeding (GIB) related to the use of antiplatelet drugs and/or NSAIDs (Table 3).
Most patients recovered or were still recovering when they were discharged (78 % [n = 145] and 14 % [n = 26], respectively). Six patients (3.6 %) had sequelae (permanent pacemaker implantation in five cases of atrioventricular block or bradyarrhythmia; left femoral nerve involvement with residual paresis in a case of retroperitoneal hematoma). Finally, nine patients (4.8 %) died; death was considered to be caused by the ADR in six cases (3.2 %). Five of them were cerebral haemorrhages related to oral anticoagulant drugs and the sixth case was an ARF related to RAS inhibitor and diuretics.
Discussion
Our study showed that 4.2 % of urgent admissions to our hospital are ADR-related and that the risk of hospitalization for this reason increases with age and the number of drugs used. The ADRs causing hospitalization are mainly type A, and the most frequent are RAS inhibitors-related ARF, bleeding caused by oral anticoagulants, and upper GIB induced by antiplatelet drugs and/or NSAIDs.
The point prevalence estimated in our study is similar to that found in meta-analyses of observational studies (which ranged from 4.7–5.3 %) [1–3] and intermediate between those calculated in two studies conducted in Spanish hospitals (3.9 and 6 %) [12, 13]. However, this prevalance is 4-fold the prevalence found in another Spanish study (1.1 %) [11], a difference likely explained by a higher degree of case ascertainment in our study due to a thorough method of identification and a wider definition of ADR.
Advanced age increases the risk of ADRs due to pharmacokinetic and pharmacodynamic changes [14, 15]. Our results showed that the risk of urgent ADR-related hospital admission increases by 60 % in patients ≥65 years. Similarly, prevalence of hospitalization due to ADRs has been found to increase with age in some previous studies [16–18] as well as in meta-analyses [2, 3], though others failed to identify age as an independent risk factor [19–22]. The mean age of patients hospitalised for ADRs has been found to be six to 28 years higher than that of patients admitted for other reasons [16, 19, 23–27]. Likewise, we observed a 9-year difference (average age 75 and 66 years, respectively). However, other studies did not show such a difference between both groups of patients [28–32].
Female gender has also been identified as an independent risk factor for ADR-related hospital admission in the general population [33], as well as in elderly patients [16–20]. Hormonal differences, differences in kinetics, and different attitudes related to the requests of healthcare attention have been proposed as likely related factors [15, 33]. Conversely, ours and other studies [19, 20] did not identify female gender as a risk factor for ADR-related hospital admission. Some studies have found a greater proportion of women among patients admitted with ADRs compared to patients hospitalised for other reasons [16, 23, 27, 31, 32] or a higher frequency of ADR-related hospital admissions in women than in men [34, 35]. Others, like ours, did not find any differences in the gender distribution [19, 25, 26, 28–30].
Polypharmacy has been pointed out as a risk factor for ADRs as well [14, 15]. In our study, the risk of ADR-related hospital admission increased by 5-fold in patients treated with more than three drugs and by 9-fold in those using more than 10, when compared to patients taking less than three drugs. Similar results have been found in some studies in the general population [19, 20] and also in the elderly [21, 22, 36]. In our study, patients admitted due to ADRs took more drugs than patients admitted for other reasons (median of 7 and 4 drugs, respectively), similarly to the findings of other investigations [19, 23–26, 28, 29, 31].
The therapeutic subgroups with a greater number of suspected pharmacological exposures in our study were diuretics, antithrombotics, RAS inhibitors and NSAIDs, which accounted for 61 % of the overall suspected pharmacological exposures. Diuretics, antithrombotics and NSAIDs stand out among the most common suspected drugs in several studies [13, 16, 18, 20, 21, 26–28, 30, 35–42] and also in a systematic review of drug-related problems causing preventable admissions to the hospital [43]. As a striking novelty, we found that the RAS inhibitors group was one of the therapeutic subgroups with a greater number of suspected exposures. They accounted for more than 10 % of suspected drugs only in two studies [26, 41].
A drug interaction was suspected in half of our cases, which fits with the results of another recent study [40]. The pattern of the drugs most frequently involved and significant polypharmacy likely explain this result found in our population. Other analyses of the proportion of drug interactions have found lower figures (17–33 %) [24, 27, 30, 36, 41].
The reactions that we most frequently identified were renal and gastrointestinal, and accounted for 60 % of cases. In other studies, digestive disorders [11, 13, 16, 18, 21, 25, 28, 29, 39, 41, 44, 45] but also renal [19–40] and haemorrhagic reactions [16, 19, 21, 40, 41, 44, 46] usually appeared among the most common reactions. The three most frequent drug-reaction associations in our study account for almost half the cases and they were ARF induced by RAS inhibitors with or without other drugs, bleeding from various locations due to oral anticoagulants, and upper GIB related to antiplatelet drugs and/or NSAIDs. In other studies, the most common association was GIB induced by either ASA [25, 27], antithrombotic drugs [18] or NSAIDs [16, 41], and the frequency of bleeding induced by anticoagulants also stood out in some of them [16, 41]. However, as far as we know, no study but ours has identified RAS inhibitor-related ARF as the most frequent ADR leading to hospital admission.
The published proportion of fatal cases ranges between 0 and 12 % [11, 16, 18, 21, 27, 28, 30–32, 38, 39, 41, 44, 46], while it was 3.2 % in our study. Most of our fatal cases were cerebral haemorrhages associated with the use of oral anticoagulants, and this is a matter of concern for us. Similar results were found in other studies where cerebral haemorrhages induced by anticoagulants were either the most frequent cause of fatal or life-threatening ADRs or one of the most frequent ADRs leading to death [18, 46].
A key aspect in the study of ADRs is the possibility of prevention. Two meta-analyses of observational studies showed an overall proportion of preventable ADR-related hospital admissions ranging between 29 and 52 % [2, 47]. A limitation of our study is failing to assess the avoidability of the ADRs identified, for which purpose different criteria have been proposed [15]. However, the classification in type A and type B reactions represents an approach to such an assessment, since type A reactions are considered predictable while type B reactions are thought to be unpredictable unless the patient has a history of previous reactions with the same drug or with related drugs [10]. Overall, 92 % of cases of ADRs identified in our study were type A reactions, in line with the results of others that have reported proportions ranging from 79 to 100 % [19, 23, 24, 27, 28, 30, 39, 40, 44].
ADRs cause a considerable consumption of health resources. In our study, the overall in-hospital stay of the 186 patients admitted with ADRs amounted to 1,785 days, 150 of them in special units for critical or semi-critical patients. Although most studies that have analysed the length of in-hospital stay have found no differences between ADR- and non-ADR-related hospital admissions [19, 23, 28, 30–32], we found a lower length of stay in patients admitted for ADRs. It has been suggested that early recognition and diagnosis of ADRs leads to early withdrawal of the suspected drugs with a subsequent quick clinical improvement that makes an early discharge easier [19]. We think that such an explanation is plausible for our results.
Some limitations that are inherent to our method of identification of ADR cases could have led us to an underestimation of the prevalence of ADR-related hospitalization. Since our method is based on the selection of patients whose admission diagnoses are included in a predefined list, we could have failed to identify diseases or medical conditions not therein included but induced by drugs. However, the number of lost cases by this reason would have been low since our list can be considered broad enough. On the other hand, admission diagnoses may be only presumptive diagnoses after an initial approach at the emergency room. A final and more accurate diagnosis is supposed to be reached during hospitalization. It is possible that some patients with admission diagnoses not included in our predefined list are eventually discharged with a listed diagnosis and some or them are ADRs. Another limitation of our study is that we did not analyse impaired renal function or comorbidity. The deterioration of renal function is a risk factor for developing ADRs, since type A reactions frequently occur if doses of drugs with renal elimination are not adjusted [15]. Impaired renal function was identified as a risk factor of ADR-related admission [20, 22]. The risk associated with comorbidity has not been investigated in depth; although it was identified in one study as one of the most important risk factors [20], several others failed to find any association [19, 21, 22]. Finally, since our study was conducted in a single, third-level teaching hospital, the generalization of our results to other settings is not possible and they could only be extrapolated to similar centres.
In contrast, several points have to be highlighted among the strengths of our study. The prospective identification of ADR cases is the first one. The second one is the use of the ADR definition currently in force in the regulatory framework of the European Union. Thirdly, our method of sample selection is supposed to have avoided the bias of seasonality over the pattern of drug use. Finally, this is the first study on ADR-related hospital admissions conducted in Spain in the last few years and provides updated quantitative and qualitative information that may allow the design of preventive strategies in our milieu. This updated information reflecting the reality of drug toxicity in a third-level hospital should allow the design of preventive strategies whose results should be analysed in future studies. In our opinion, such studies should prioritise ADRs with a fatal outcome, those related to drug interactions, and those induced by RAS inhibitors.
References
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients. A meta-analysis of prospective studies. JAMA 279:1200–1205
Beijer HJM, de Blaey CJ (2002) Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci 24:46–54
Kongkaew C, Noyce PR, Ashcroft DM (2008) Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother 42:1017–1025
Leendertse AJ, Visser D, Egberts ACG, van den Bemt PMLA (2010) The relationship between study characteristics and the prevalence of medication-related hospitalizations. Drug Saf 33:233–244
Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356:1255–1259
Commission Directive 2010/84/EU of the European Parliament and the Council of 15 December 2010 amending as regards pharmacovigilance, Directive 2001/83/EC on the Community code relating to medicinal products for human use. Official Journal of the European Union 31.12.2010: L348/74-L348/99. http://ec.europa.eu/health/files/eudralex/vol-1/dir_2010_84/dir_2010_84_en.pdf. Accessed 17 September 2013
Real Decreto 1344/2007, de 11 de octubre, por el que se regula la farmacovigilancia de medicamentos de uso humano. Boletín Oficial de Estado 1/11/2007: 44631-4460. http://www.boe.es/boe/dias/2007/11/01/pdfs/A44631-44640.pdf. Accessed 17 September 2013
Meyboom RHB, Royer RJ (1992) Causality classification at pharmacovigilance centres in the European Community. Pharmacoepidemiol Drug Saf 1:87–97
WHO Collaborating Centre for Drug Statistics Methodology. Norwegian Institute of Public Health. The Anatomical Therapeutic Chemical (ATC) classification system. http://www.whocc.no. Accessed 17 September 2013
Gruchalla RS (2000) Clinical assessment of drug-induced disease. Lancet 356:1505–1511
Ibañez L, Laporte J-R, Carné X (1991) Adverse drug reactions leading to hospital admissions. Drug Saf 6:450–459
Garijo B, de Abajo FJ, Castro MA, Lopo CR, Carcas A, Frías J (1991) Hospitalizaciones motivadas por fármacos: un estudio prospectivo. Rev Clin Esp 188:7–12
Martín MT, Codina C, Tuset M, Carné X, Nogué S, Ribas J (2002) Problemas relacionados con la medicación como causa de ingreso hospitalario. Med Clin (Barc) 118:205–210
Routledge PA, O’Mahony MS, Woodhouse KW (2003) Adverse drug reactions in elderly patients. Br J Clin Pharmacol 57:121–126
Davies EC, Green CF, Mottram DR et al (2007) Adverse drug reactions in hospitals: a narrative review. Curr Drug Saf 2:79–87
Ruiter R, Visser LE, Rodenburg EM, Trifirò G, Ziere G, Stricker BH (2012) Adverse drug reaction-related hospitalizations in persons aged 55 years and over. A population-based study in the Netherlands. Drugs Aging 29:225–232
Pouyanne P, Haramburu F, Imbs JL, Bégaud B, for the French Pharmacovigilance Centres (2000) Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. Br Med J 320:1036
Van der Hooft CS, Dieleman JP, Siemes C, Aarnoudse AJLHJ, Verhamme KMC, Stricker BHCH, Sturkenboom MCJM (2008) Adverse drug reaction-related hospitalisations: a population-based cohort study. Pharmacoepidemiol Drug Saf 17:365–371
Alexopoulou A, Dourakis SP, Mantzoukis D, Pitsariotis T, Kandyli A, Deutsch M, Archimandritis AJ (2008) Adverse drug reactions as a cause of hospital admission: a 6-month experience in a single center in Greece. Eur J Intern Med 19:505–510
Leendertse AJ, Egberts ACG, Stoker LJ, van den Bemt PMLA, for the HARM Study Group (2008) Frequency of and risk factors for presentable medication-related hospital admissions in the Netherlands. Arch Intern Med 168:1890–1896
Onder G, Pedone C, Landi F, Cesari M, Della Vedova C, Bernabei R, Gambassi G (2002) Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc 50:1962–1968
Caamaño F, Pedone C, Zuccalà G, Carbonin P (2005) Socio-demographic factors related to the prevalence of adverse drug reaction at hospital admission in elderly population. Arch Gerontol Geriatr 40:45–52
Moore N, Lecointre D, Noblet C, Mabille M (1998) Frequency and cost of serious adverse drug reactions in a department of general medicine. Br J Clin Pharmacol 45:301–308
Von Euler M, Eliasson E, Öhlén G, Bergman U (2006) Adverse drug reactions causing hospitalization can be monitored from computerized medical records and thereby indicate the quality of drug utilization. Pharmacoepidemiol Drug Saf 15:179–184
Brvar M, Fokter N, Bunc M, Mozina M (2009) The frequency of adverse drug reaction related admissions according to method of detection, admission urgency and medical department speciality. BMC Clin Pharmacol 9:8
Ahern F, Sahm LJ, Lynch D, McCarthy S (2013) Determining the frequency and preventability of adverse drug reaction-related admissions to an Irish University Hospital: a cross-sectional study. Emerg Med J. doi:10.1136/emermed-2012-201945
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients. Br Med J 329:15–19
Mjörndal T, Boman MD, Hägg S, Bäckström M, Wiholm B-E, Wahlin A, Dahlqvuist R (2002) Adverse drug reactions as a cause for admissions to a department of internal medicine. Pharmacoepidemiol Drug Saf 11:65–72
Olivier P, Boulbés O, Tubery M, Lauque D, Montastruc J-L, Lapeyre-Mestre M (2002) Assessing the feasibility of using and adverse drug reaction preventability scale in clinical practice. A study in a French emergency department. Drug Saf 25:1036–1044
Hopf Y, Watson M, Williams D (2008) Adverse-drug-reaction related admissions to a hospital in Scotland. Pharm World Sci 30:854–862
Lagnaoui R, Moore N, Fach J, Longy-Boursier M, Bégaud B (2000) Adverse drug reactions in a department of systemic diseases-oriented internal medicine: prevalence, incidence, direct costs and avoidability. Eur J Clin Pharmacol 56:181–186
Fattinger K, Roos M, Vergères P, Holenstein C, Kind B, Masche U, Stocker DN, Braunschweig S, Kullak-Ublick GA, Galeazzsi RL, Follath F, Gasser T, Meier PJ (2000) Epidemiology of drug exposure and adverse drug reactions in two Swiss departments of internal medicine. Br J Clin Pharmacol 49:158–167
Zopf Y, Rabe C, Neubert A, Gabmann KG, Rascher W, Hahn EG, Brune K, Dormann H (2008) Women encounter ADRs more often than do men. Eur J Clin Pharmacol 64:999–1004
Rodenburg EM, Stricker BHC, Visser LE (2011) Sex-related differences in hospital admissions attributed to adverse drug reactions in Netherlands. Br J Clin Pharmacol 71:95–104
Budnitz DS, Loovegrove MC, Shehab N, Richards CL (2011) Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 365:2002–2012
Olivier P, Bertrand L, Tubery M, Lauque D, Montastruc J-L, Lapeyre-Mestre M (2009) Hospitalizations because of adverse drug reactions in elderly patients admitted though the emergency department. A prospective study. Drugs Aging 26:475–482
McDonnell J, Jacobs MR (2002) Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 36:1331–1336
Wu WK, Pantaleo N (2003) Evaluation of outpatient adverse drug reactions leading to hospitalization. Am J Health Syst Pharm 60:253–259
Rottenkolber D, Schmiedl S, Rottenkolber M, Farker K, Saljé K, Mueller S, Hippius N, Thuermann PA, Hasford J, for the Net of Regional Pharmacovigilance Centers (2011) Adverse drug reactions in Germany: direct costs of internal medicine hospitalizations. Pharmacoepidemiol Drug Saf 20:626–634
Hofer-Dueckelmann C, Prinz E, Beindi W, Szymanski J, Fellhofer G, Pichler M, Schuler J (2011) Adverse drug reactions (ADRs) associated with hospital admissions—elderly female patients are at higher risk. Int J Clin Pharmacol Ther 49:577–586
Franceschi M, Scarcelli C, Niro V, Seripa D, Pazienza AM, Pepe G, Colusso AM, Pacilli L, Pilotto A (2008) Prevalence, clinical features and avoidability of adverse drug reactions as cause of admission to a geriatric unit. A prospective study of 1756 patients. Drug Saf 31:545–556
Hartholt KA, van der Velde N, Looman CWN, Panneman MJM, van Beek EF, Patka P, van der Cammen TJM (2010) Adverse drug reactions related hospital admissions in persons aged 60 years and over, The Netherlands, 1981-2007: less rapid increase, different drugs. PLoS ONE 5:e13977
Howard RL, Avery AJ, Slavenburg S, Royal S, Pipe G, Licassen P, Pirmohamed M (2007) Which drugs cause presentable admissions to hospital? A systematic review. Br J Clin Pharmacol 63:136–147
Schneeweiss S, Hasford J, Göttler M, Hoffmann A, Riethling A-K, Avorn J (2002) Admissions caused by adverse drug events to internal medicine and emergency departments in hospitals: a longitudinal population-based study. Eur J Clin Pharmacol 58:258–291
Conforti A, Constantini D, Zanetti F, Moretti U, Grezzana M, Leone R (2012) Adverse drug reactions in older patients: an Italian observational prospective hospital study. Drug Healthc Patient Saf 4:75–80
Patel KJ, Media MS, Bajpai D, Mehta SS, Kshirsagar NA, Gogtay NJ (2007) Evaluation of the prevalence and economic burden of adverse drug reactions presenting to the medical emergency department of a tertiary referral centre: a prospective study. BMC Clin Pharmacol 7:8
Hakkarainen KM, Hedna K, Petzold M, Hägg S (2012) Percentage of patients with preventable adverse drug reactions and preventability of adverse drug reactions—A meta-analysis. PLoS ONE 7:e33236
Acknowledgments
The authors would like to thank the staff of the Admissions Unit of Bellvitage University Hospital, who on a daily-basis, and always on time, provided us with the daily list of urgent admissions.
Conflict of interest
No sources of funding were used to assist in the development of this study. The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 57 kb)
Rights and permissions
About this article
Cite this article
Pedrós, C., Quintana, B., Rebolledo, M. et al. Prevalence, risk factors and main features of adverse drug reactions leading to hospital admission. Eur J Clin Pharmacol 70, 361–367 (2014). https://doi.org/10.1007/s00228-013-1630-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-013-1630-5